Endovascular Treatment of an Unruptured Posterior Inferior Cerebellar Artery Incorporating Fusiform Vertebral Artery Aneurysm using Simultaneous Trans Circulatory Bilateral Vertebral Artery Access and, Kissing Vertebral Artery and PICA Stents and Pla
Abstract
A fusiform intracranial aneurysm can be defined as a diffuse dilatation of an arterial segment such that a large percentage of the vessel’s circumference is pathologically dilated. These aneurysms are distinguished form saccular (aka: berry) intracranial aneurysms in that they do not harbor an aneurysm neck that aids with surgical exclusion of the lesion from the native circulation. Treatment of fusiform intracranial aneurysms is technically challenging because of the lesion’s broad involvement of the arterial lumen and the absence of a distinct aneurysm neck that can help during lesion obliteration. These lesions often present with critical branch vessels arising from the fusiform segment. Preservation of flow through the branch vessel can be difficult because elimination of the fusiform segment may lead to branch vessel occlusion and subsequent ischemic stroke in the branch vessel’s supplied brain territory.
This article describes a patient with an unruptured fusiform Vertebral Artery (VA) aneurysm where the Posterior Inferior Cerebellar Artery (PICA) arose from the diseased segment of the aneurysmal. Aneurysm treatment was achieved using multiple catheters, stents, and coils through a transcirculatory approach.
Keywords
Aneurysm • Vertebral artery • Posterior inferior cerebellar artery • Endovascular • Stents • Coils
Introduction
A fusiform intracranial cerebral aneurysm that incorporates a critical cortical branch artery can be particularly difficult to treat due to the need to eliminate the aneurysm while at the same time preserve patency of the branch vessel that arise from the lesion which in turn supplies blood flow to critical cerebral tissue. The following manuscript describes management of an unruptured, fusiform, intracranial vertebral artery aneurysm that incorporated the posterior inferior cerebellar artery origin in the fusiform lesion. Aneurysm treatment was achieved using a combination of neck remodeling devices (aka: aneurysm stents), platinum coils and dual trans- circulatory catheter placement.
Case Presentation
A 56-year-old man presented with vague neurologic complaints that suggested a transient ischemic event. Imaging demonstrated an unruptured right Vertebral Artery (VA) V4 9 × 6 mm fusiform aneurysm involving the Posterior Inferior Cerebellar Artery (PICA) segment such that the PICA arose from the aneurysm’s fundus near its equator (Figure 1A and 1B). A second 10 mm fusiform aneurysm involving the right cervical Internal Carotid Artery (ICA) was also identified. The patient’s past medical history was notable for a motor vehicle accident at the age of 17 which involved an ejection through the car’s windshield which left the patient comatose for 7 days and hospitalized for 1 month. For treatment of the VA lesion, the patient selected endovascular therapy as opposed to clip reconstruction or sacrifice with right PICA-left PICA side to side anastomosis. Previous diagnostic arteriography had demonstrated a more dominant left VA, left and right VA that independently opacified the right PICA, and an extra cranial upper cervical left internal carotid artery aneurysm. There was no history of trauma and subsequent connective tissue disorder testing was negative. Bilateral fusiform aneurysms, however, suggested an unrecognized traumatic etiology and raised the specter of both lesions being dissecting in origin. The patient understood that while the therapeutic goal was preservation of his right PICA and right VA, the fallback option was right VA sacrifice, partial aneurysm embolization and right PICA preservation. PICA loss was not considered an acceptable outcome shown in the Figure 1C.
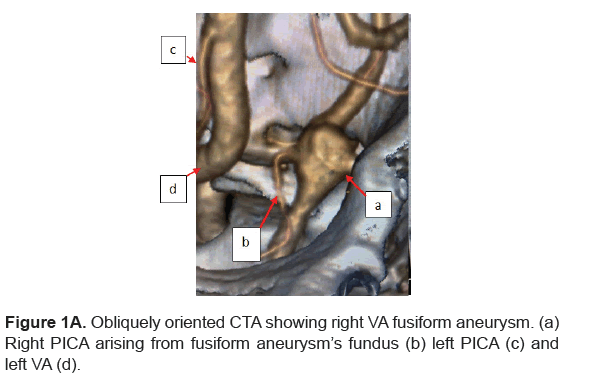
Figure 1A: Obliquely oriented CTA showing right VA fusiform aneurysm. (a) Right PICA arising from fusiform aneurysm’s fundus (b) left PICA (c) and left VA (d).
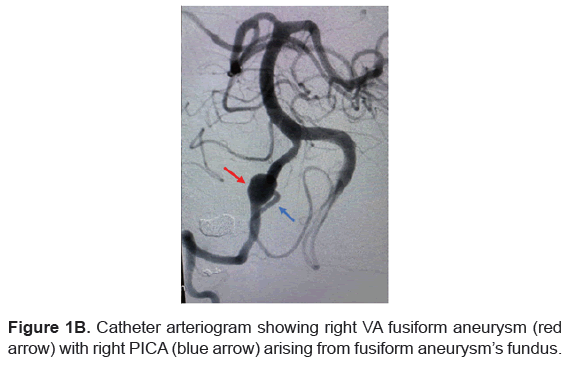
Figure 1B: Catheter arteriogram showing right VA fusiform aneurysm (red arrow) with right PICA (blue arrow) arising from fusiform aneurysm’s fundus.
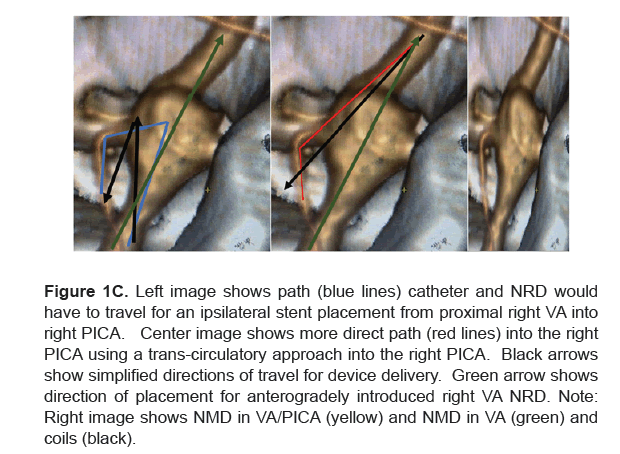
Figure 1C: Left image shows path (blue lines) catheter and NRD would have to travel for an ipsilateral stent placement from proximal right VA into right PICA. Center image shows more direct path (red lines) into the right PICA using a trans-circulatory approach into the right PICA. Black arrows show simplified directions of travel for device delivery. Green arrow shows direction of placement for anterogradely introduced right VA NRD. Note: Right image shows NMD in VA/PICA (yellow) and NMD in VA (green) and coils (black).
Following induction of general anesthesia and establishing SSEP, BAER, and EEG neurophysiologic monitoring, the patient’s right and left common femoral arteries were Seldinger accessed with 6F sheaths. 6F straight Envoy (Codman Neuro, Rayntham, MA) catheters were then each advanced into the right and left VAs. The patient was heparinized to maintain ACT 260. Digital subtraction and road mapped images were then obtained of the posterior circulation. A 0.010-inch micro-catheter was advanced from the left VA to the right VA, into the right VA aneurysm and then into the right PICA (trans-circulatory approach). A second microcatheter and wire were advanced into the right VA traversing the aneurysm and positioned in the right VA distal to the aneurysm. An Atlas (Stryker Medical, Kalamazoo, MI) 4 mm × 21 mm neck remodeling device was advanced into the PICA microcatheter and an Atlas 4 mm × 23 mm was advanced into the right VA microcatheter. The patient was administered a? mg I.V. Aggrastat bolus. Each stent was now deployed such that the distal VA housed kissing stents, one of which extended into the proximal right VA and the second of which extended from the distal right VA into the right PICA (retrograde insertion) (Figure 2). With the stents in position to reconstruct the native vascular anatomy, the stent delivery catheters were removed. A 0.010- inch microcatheter was now advanced into the right VA stent lumen and cross walled into the fusiform aneurysm. Target coils (Stryker Medical, Kalamazoo, MI) were deposited into the fundus until obliteration was achieved. Final angiographic imaging demonstrated right VA and right PICA preservation. The right PICA opacified from both the left and right post-treatment VA angiographic runs (Figure 2). Catheters were removed and the patient awakened at his neurologic baseline. He was discharged on Plavix 75 mg QD and ASA 81 mg QD and a therapeutic P2Y12 assay.
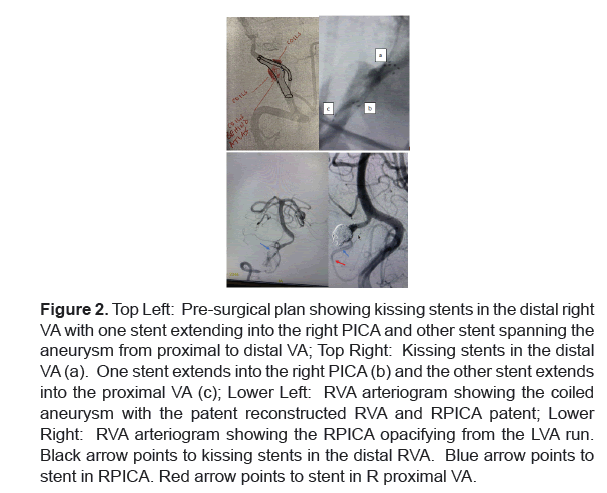
Figure 2: Top Left: Pre-surgical plan showing kissing stents in the distal right VA with one stent extending into the right PICA and other stent spanning the aneurysm from proximal to distal VA; Top Right: Kissing stents in the distal VA (a). One stent extends into the right PICA (b) and the other stent extends into the proximal VA (c); Lower Left: RVA arteriogram showing the coiled aneurysm with the patent reconstructed RVA and RPICA patent; Lower Right: RVA arteriogram showing the RPICA opacifying from the LVA run. Black arrow points to kissing stents in the distal RVA. Blue arrow points to stent in RPICA. Red arrow points to stent in R proximal VA.
Follow-up angiography 6 months later (Figure 3) revealed patency of the proximal right VA, complete aneurysm obliteration, a patent right PICA continuing to opacify from the right vertebral artery injection even though the PICA arose from a mid-position on the fusiform VA aneurysm, and patency of the distal right VA which opacified from the left VA arteriographic injection.
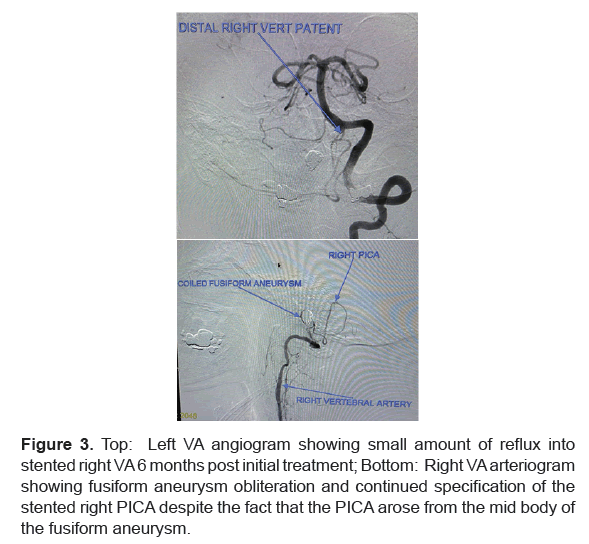
Figure 3: Top: Left VA angiogram showing small amount of reflux into stented right VA 6 months post initial treatment; Bottom: Right VA arteriogram showing fusiform aneurysm obliteration and continued specification of the stented right PICA despite the fact that the PICA arose from the mid body of the fusiform aneurysm.
Results and Discussion
A fusiform intracranial aneurysm can be defined as a diffuse dilatation of and arterial segment such that a large percentage of the vessel’s circumference is pathologically dilated. These aneurysms are distinguished form saccular (aka: berry) intracranial aneurysms in that they do not harbor an aneurysm neck that aids with surgical exclusion of the lesion from the native circulation. Treatment of fusiform intracranial aneurysms is technically challenging because of the lesion’s broad involvement of the arterial lumen and the absence of a distinct aneurysm neck that can help during lesion obliteration. These lesions often present with critical branch vessels arising from the fusiform segment. Preservation of flow through the branch vessel can be difficult because elimination of the fusiform segment may lead to branch vessel occlusion and subsequent ischemic stroke in the branch vessels supplied brain territory.
Eleven percent of posterior circulation aneurysms and 3%-5% of subarachnoid hemorrhages are due to VA aneurysms. VA aneurysms that involve the PICA have higher rates of progression and rupture and high morbidity. Treatment of VA/PICA aneurysms requires simultaneous PICA preservation and aneurysm obliteration. While this can be difficult to achieve when the aneurysm involves the VA/PICA branch point or the PICA alone, it is even more vexing when the VA itself is fusiform and the PICA takes its origin from the VA aneurysm’s fundal wall. In such situations, preservation of the PICA and occlusion of the VA aneurysm requires complex reconstructions because VA fusiform aneurysm trapping, and VA sacrifice will not preserve PICA’s patency. For this reason, surgeons often resort to open (exovascular) fenestrated clip VA reconstruction. This procedure is technically difficult, often injures CN’s 6,8,9,10,11 and 12 and, by necessity, includes aneurysmal tissue as part of the reconstructed VA’s lumen. This abnormal tissue can continue to expand leading to aneurysm recurrence and rupture. Alternatively, exovascular aneurysm trapping and VA sacrifice can be utilized when the contralateral VA and PICA are patent and PICA-to-PICA side wall anastomoses can be performed. While this strategy seems straightforward, it is complicated by the difficulties inherent in anastomosing and keeping patent vessels that have a mean diameter of 1.84 mm [1].
In 1994, coil embolization of intracranial aneurysms obtained US FDA approval. This event led to a gradual paradigm shift in the management of a major neurologic anatomic disorder. In 1998, the corresponding author MH) published a review of 38 consecutive PICA aneurysms treated using open clipping (exovascular approach) at a major cerebrovascular center. This study shed light on the morbidity and mortality (66% post-surgical new neurologic deficits) surrounding such therapy and raised the concept of whether endovascular approaches could reduce complications by negating the necessity of cranial nerve manipulations required for clipping [2].
Since 1994, endovascular surgeons have adapted trans arterial catheter therapy to a variety of intracranial aneurysms including PICA lesions. As devices improved, more difficult lesions were chosen for transcatheter therapy. These included small aneurysms, fusiform aneurysms, dissecting aneurysms, and aneurysms that incorporated vessels such as the VA and PICA.
The approval of intracranial Neck Remodeling Devices (NRD; stents) for the endovascular coiling of wide necked aneurysm which were classically defined as lesions with a fundus: neck ratio greater than 2.0 expanded endovascular treatment options. Once NRDs became available, neuroendovascular surgeons quickly realized the utility such devices had for arterial reconstruction.
Since 2011 (and perhaps earlier) many authors have published their and others’ experience using coils and stents to treat PICA aneurysms. A review of select publications that shed light on our decision-making process prior to and during trans-circulatory kissing stent treatment of our patient’s pathology. The contralateral VA approach (aka: trans circulatory) for treatment of two PICA aneurysms was described by Albuquerque, et al in 2011 [3]. In 2012, Jeon, et al. outlined the benefits of a contralateral VA approach for contralateral PICA catheterization to take advantage of more favorable anatomic geometry [4]. These authors noted that PICA origin aneurysm treatment can be difficult because PICA preservation is paramount. The authors felt that in certain situations PICA preservation was best achieved using VA-PICA arterial stenting, but noted that such placement was often thwarted because the PICA could arise at an acute angle from the VA. The authors, therefore, suggested that in select cases ipsilateral approach for coil delivery and contralateral “cross-over” (aka: trans-circulatory) approach for stent delivery might prove more viable. Ecker, et al. added to the literature by describing a successful contralateral PICA stent approach in two patients [5]. In 2013, Cho, et al. documented ipsilateral and contralateral approaches for placement of VA-PICA stents during successful coil embolization of seven PICA aneurysms [6]. Samaniego, et al. [7], subsequently reported on seven patients who had ruptured and unruptured PICA aneurysms treated with stents without procedural complications, with Glasgow outcomes of 5, and with excellent angiographic results.
Regarding kissing stents, a 2016 literature review of kissing Y stent reconstruction of intracranial vessels for aneurysm embolization, identified a single case in which the technique was utilized to treat a PICA/VA aneurysm [8].
In 2014, Zhao, et al. reported on their group’s experience using single VA stents and coils to treat vertebral artery dissecting aneurysms that incorporated the PICA [9]. After reviewing outcomes in 113 such aneurysms treated over 10 years, the authors concluded that long term obliteration rates were negatively influenced when the dissecting VA aneurysm involved the PICA and when the lesion was incompletely treated during the initial surgery. These well-known failure factors influenced our decision in the case described above to perform PICA and VA reconstruction and coil embolization with the hope that complete obliteration could be achieved. We felt a single VA or single VA-PICA stent would not permit for PICA or VA preservation and noted that even VA sacrifice would not permit for complete aneurysm obliteration if the PICA were to be preserved. The authors concluded that flow diverters might provide future solutions. The use of diverters has since been reported by Fu, et al. whose team successfully treated 32 aneurysms with the Pipeline device (Medtronic Minneapolis, MN) [10]. While off label use of a flow diverter was considered in this case, we believed that the diverter would not oppose the fusiform wall at the point where the PICA arose from the fundus and that flow through the patent PICA would inhibit thrombosis of the portion of the aneurysm fundus that gave rise to the PICA, thus increasing the likelihood of progressive aneurysm growth and perhaps rupture [11].
Conclusion
This report is the author’s second to document unusual management of a VA-PICA aneurysm. Documents the application of a simultaneous trans- circulatory and ipsilateral circulatory approach for the treatment of an unruptured large fusiform VA/PICA potentially dissecting type aneurysm. Placement of kissing stents into the VA and PICA reconstructed the native arterial anatomy. This was immediately followed by coil embolization of the aneurysm using platinum coils thus maintaining VA and PICA patency while occluding the VA’s aneurysmal segment. Six month follow up angiography demonstrated aneurysm occlusion and continued patency of the stent protected right PICA, despite the fact that this vessel arose from a position along the equator of the fusiform vertebral artery lesion.
Declarations
Ethics approval and consent to participate
This case report and literature review is devoid of any personal identifying information. It is a retrospective report and required no patient consent.
Consent for publication
No individual personal data was contained in this study.
Availability of data and materials
The data analyzed for this report is available from the corresponding author on reasonable request.
Competing Interests
The author has no financial or other interests associated with this case report.
Funding
This case report was written without the assistance of outside funding.
Disclosures
The authors have no prior or potential financial conflicts-of-interest to disclose.
References
- Akgun, V, et al. ‘’Normal anatomical features and variations of the vertebrobasilar circulation and its branches: An analysis with 64-detector row CT and 3T MR angiographies.’’ Scientific World Journal (2013):620162.
[Cross ref] [Google scholar] [PubMed]
- Horowitz, M, et al. ‘’Posteroinferior cerebellar artery aneurysms: Surgical results for 38 patients.’’ Neurosurgery 43.5(1998):1026-1031.
[Cross ref] [Google scholar] [PubMed]
- Albuquerque, FC, et al . ‘’Transcirculation endovascular treatment of complex cerebral aneurysms: Technical considerations and preliminary results.’’ Neurosurgery 68.3(2011):820-830.
[Cross ref] [Google scholar] [PubMed]
- Jeon, S, et al. ‘’Bilateral approach for stent-assisted coiling of posterior inferior cerebellar artery aneurysms-two cases.’’ J Cerebrovasc Endovasc Neurosurg 14.3(2012): 223-227.
[Cross ref] [Google scholar] [PubMed]
- Ecker, R, et al. ‘’Contralateral vertebral approach for stenting and coil embolization of a large, thrombosed vertebral–posterior inferior cerebellar artery aneurysm: Case report.’’ J Cerebrovasc Endovasc Neurosurg
[Cross ref] [Google scholar] [PubMed]
- Cho, YD, et al. ‘’Stent-assisted coil embolization of wide-necked posterior inferior cerebellar artery aneurysms.’’ Neuroradiology 55(2013):877-882.
[Cross ref] [Google scholar] [PubMed]
- Samaniego, EA, et al. ‘’Endovascular treatment of PICA aneurysms with a Low-profile Visualized Intraluminal Support (LVIS Jr) device.’’ J Neurointerv Surg 8(2016):1030-1033.
[Cross ref] [Google scholar] [PubMed]
- Brassel, F, et al. ‘’Kissing-Y stenting for endovascular treatment of complex wide necked bifurcation aneurysms using Acandis Acclino stents: Results and literature review.’’ J Neurointerv Surg 8(2016):386-395.
[Cross ref] [Google scholar] [PubMed]
- Zhao, KJ, et al. ‘’The Interaction between stent(s) implantation, PICA involvement, and immediate occlusion degree affect symptomatic intracranial spontaneous vertebral artery dissection aneurysm (sis-VADA) recurrence after reconstructive treatment with stent(s)-assisted coiling.’’ European Radiol 24(2014):2088-2096.
[Cross ref] [Google scholar] [PubMed]
- Fu, W, et al. ‘’Treatment of unruptured vertebral artery aneurysm involving posterior inferior cerebellar artery with pipeline embolization device.’’ Front Neurol 12:622457.
[Cross ref] [Google scholar] [PubMed]
- Vora, N, et al. ‘’Retrograde back-coiling technique for a ruptured aneurysm of a double posterior inferior cerebellar artery.’’ J Neurointerv 19(2009):65-67.
[Cross ref] [Google scholar] [PubMed]
Author Info
HCA Florida First Coast Neurosurgery, HCA Florida Orange Park Hospital, 1825 Kingsley Avenue, Florida, United StatesReceived: 22-Sep-2022, Manuscript No. JBTW-22-75523; Editor assigned: 26-Sep-2022, Pre QC No. JBTW-22-75523 (PQ); Reviewed: 10-Oct-2022, QC No. JBTW-22-75523 (QC); Revised: 17-Oct-2022, Manuscript No. JBTW-22-75523 (R); Published: 27-Oct-2022, DOI: 10.35248/2322-3308.11.6.002
Citation: Horowitz MB. Endovascular Treatment of an Unruptured Posterior Inferior Cerebellar Artery Incorporating Fusiform Vertebral Artery Aneurysm using Simultaneous Trans Circulatory Bilateral Vertebral Artery Access and, Kissing Vertebral Artery and PICA Stents and Platinum Coils: Case Report and Literature Review J Biol Today's World, 2022, 11(6), 001-004
Copyright: © 2022 Horowitz MB. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.