
Advances in Pediatric Research
Open Access
ISSN: 2385-4529

ISSN: 2385-4529
Case Report - (2022)Volume 9, Issue 5
Lipoblastoma is a rare, encapsulated tumor that originates from the embryonal fat tissue. Intraabdominal lipoblastoma is less commonly encountered, accounting for less than 10% of all Lipoblastomas. These tumours exhibit excellent long-term prognosis and gross total resection remains the mainstay treatment. Here we present a 2 year old girl with extraordinary 1,505 gram abdominal Lipoblastoma who initially presented with a painless abdominal distention. The patient was successfully treated with gross total resection.
Abdominal mass; Lipoblastoma; Lipoblastomatosis; Lipoma; Libosarcoma
Lipoblastoma is a rare, encapsulated tumor that originates from the embryonal fat tissue. lipoblastoma and lipoblastomatosis can involve several areas in the body but Intra-abdominal lipoblastoma is less commonly encountered, accounting for less than 10% of all lipoblastomas. These tumors exhibit excellent long-term prognosis and gross total resection remains the mainstay treatment. Abdominal CT is sufficient to carry out the diagnosis without the need for an MRI abdomen or other lab investigations. No specific tumor markers or metastatic work up are required to be carried out as Lipoblastoma is a benign tumor. Even-though CT abdomen maybe sufficient to diagnose Lipoblastoma, a dilemma in diagnosis is usually faced with small size ones located on the uncommon locations. Grading lipoblastoma upon size and location hasn’t been well documented in literature. Reluctance in grading could have been related to the good prognosis and to no need for adjuvant chemotherapy or radiotherapy in treatment.
A 2 year old child was referred to the emergency room by her pediatrician due to a large abdominal mass. The child had no previous medical history and had reached her developmental milestones. Remarkably, her family reported that their daughter had a distended abdomen ever since birth, with a slowly progressive increase in her abdominal circumference. Otherwise, she was asymptomatic, and denied abdominal pain, constipation, decreased oral intake, or vomiting. On presentation, the child appeared active and playful. Her growth parameters were appropriate to age. Vital signs were within the normal range. Physical exam revealed a soft non-tender abdomen, with a palpable right-predominant midline mass. No hepato-splenomegaly was noted. Abdominal circumference measured 50 cm. She had normal bowel sounds, and no other appreciated pertinent positives on physical exam. All laboratory tests including complete blood count, electrolytes, liver function tests, uric acid and lactate dehydrogenase were within normal limits.
Abdominal CT scan was performed and revealed a large lipomatous right retroperitoneal mass occupying most of the right aspect of the abdomen and extending beyond the midline to the left (Figures 1a-1c), measuring approximately 15 × 13 × 15 cm. The mass showed heterogeneous fat density with multiple linear and hazy areas of soft tissue density. The mass extended from the sub-hepatic and right perinephric space to the right pelvic inlet. Posteriorly, the mass appeared to compress the right kidney and the Inferior Vena Cava (IVC).
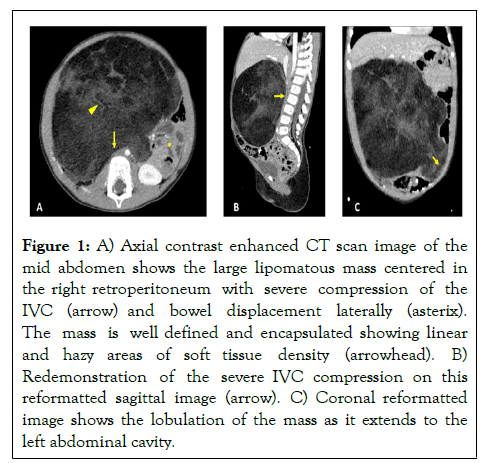
Figure 1: A) Axial contrast enhanced CT scan image of the mid abdomen shows the large lipomatous mass centered in the right retroperitoneum with severe compression of the IVC (arrow) and bowel displacement laterally (asterix). The mass is well defined and encapsulated showing linear and hazy areas of soft tissue density (arrowhead). B) Redemonstration of the severe IVC compression on this reformatted sagittal image (arrow). C) Coronal reformatted image shows the lobulation of the mass as it extends to the left abdominal cavity.
Subsequently, she underwent laparotomy and complete surgical resection of the mass. The tumor was completely squeezing the IVC to a slit-like opening, and a tortuous retrocecal appendix appeared stuck to it. Grossly, the mass was encapsulated, weighed 1,505 grams, and measured 25 × 16 × 13 cm. It was lobulated and completely enveloped by a thin smooth layer of fibrous tissue (Figure 2). Cross sections revealed a homogeneous tan-white moderately firm cut surface with scattered areas of minute hemorrhages.
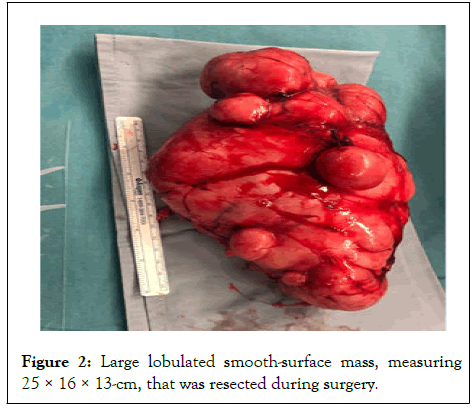
Figure 2: Large lobulated smooth-surface mass, measuring 25 × 16 × 13 cm, that was resected during surgery.
On histopathologic examination, the mass had a diffuse to vaguely lobulated growth pattern. The neoplastic cells were mostly composed of mature adipocytes admixed with some immature spindle cells and rare interspersed lipoblasts. There were variable amounts of myxoid stroma associated with a plexiform capillary network (Figure 3). Therefore, the diagnosis of lipoblastoma was confirmed.
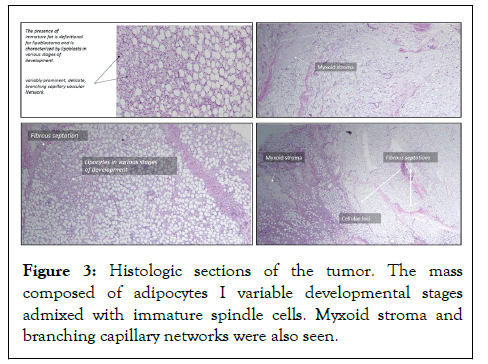
Figure 3: Histologic sections of the tumor. The mass composed of adipocytes I variable developmental stages admixed with immature spindle cells. Myxoid stroma and branching capillary networks were also seen.
The patient had uneventful surgery, and was discharged from hospital after four days. The patient still has regular follow up to the clinic for physical examination and for ultrasound abdomen for follow up.
Lipoblastoma is a rare, encapsulated tumor that originates from the embryonal fat tissue [1]. It exhibits two forms: malignant (liposarcoma) and benign (lipoma, lipoblastoma, lipoblastomatosis) [2]. Lipoblastoma is primarily seen in children below 3 years of age and for unknown reasons it is more common in males. As evident in various case series and case reports, lipoblastoma and lipoblastomatosis can involve several areas in the body including extremities, thorax, abdomen and even the neck. In fact, Shih-Ming has suggested the neck to be the most common presenting site for lipoblastoma [3].
The lipoblastoma masses can grow to achieve more than 20 cm in diameter with weight exceeding 1-kg [4]. Intra-abdominal lipoblastoma is less commonly encountered, accounting for less than 10% of all lipoblastomas [1]. They commonly present aspainless progressively increasing abdominal mass in Patients may also exhibit clinical manifestations secondary to the tumor size and location such as vomiting, lethargy and abdominal pain. Hernia may also be seen with large size tumors [3]. Acute manifestations, such as volvulus or intussusception, although rare, are also reported by David [5].
Grossly, the tumor can appear circumscribed, such as lipoblastoma, or can diffuse with ill-defined shape, such as lipoblastomatosis. Histologically, it can be difficult to differentiate lipoblastoma and liposarcoma; in some cases, molecular and cytogenetic studies might be required to reach the final diagnosis [6].
Nevertheless, liposarcoma remains extremely rare in young children.These tumors exhibit excellent long-term prognosis. Gross total resection remains the mainstay treatment for both types. Although both forms are non-metastatic in nature, they exhibit high recurrence rate, reaching up to 25% of diagnosed cases. Diffuse tumor is associated with higher chance of recurrence [7].
The majority of patients are managed with complete surgical resections, while few display unresectable tumor. Surgical resection can be specifically challenging, as some are deep seated, intertwined with the small intestines, or are adhering to the mesentery [8].
Due to the benign nature of the tumor, preserving adjacent significant structures is prioritized over extensive surgical excision. Mognato even suggested spontaneous resolution of lipoblastoma with conservative management [9]. Other modalities of treatment such as radiation therapy and chemotherapy are not routinely employed in the management of these tumors [1]. Despite many publications recommending follow-up with regular ultrasound for 3 years Emmanulle Seguir- Lipsyc et al. has proposed to follow-up with MRI, and for longer duration. This stems from the finding that recurrence has been detected as late as 10 years after resection [1]. Incompletely resected tumors and lipoblastomatosis have more chances of recurrence; therefore, longer follow up period is recommended.
In short, abdominal lipoblastoma although rare, should remain in the differential of young children presenting with painlessabdominal mass. Complete surgical resection and careful follow up continue to be the standard of care. No rule for chemotherapy or Radiation therapy in this disease. Prognosis after surgery usually caries excellent results. They don’t metastasize or invade other solid organs. They can develop to enormous sizes exceeding 1000 gram without causing acute abdominal symptoms. Updating the grading and the guidelines of treating abdominal lipoblastoma can be developed with further cohort studies.
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
Citation: Fahad N, Abboud M, Zareef R, Akel S, Natout M, Sakr R (2022) A 2-Year-Old with an Enormous Abdominal Lipoblastoma: A Case Report and a Literature Review. Adv Pediatr Res. 9:040.
Received: 30-Aug-2022, Manuscript No. LDAPR-22-19034; Editor assigned: 02-Sep-2022, Pre QC No. LDAPR-22-19034 (PQ); Reviewed: 19-Sep-2022, QC No. LDAPR-22-19034; Revised: 27-Sep-2022, Manuscript No. LDAPR-22-19034 (R); Published: 05-Oct-2022 , DOI: 10.35248/2385-4529.22.9.040
Copyright: © 2022 Fahad N, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.