Advances in Medical Ethics
Open Access
ISSN: 2385-5495
ISSN: 2385-5495
Research Article - (2016)Volume 3, Issue 1
Systematic ethics work and ethics discussions may help practitioners handle the many ethical challenges and dilemmas that have been described in the scientific literature pertaining to nursing homes. This review is based on a selective literature search of relevant publications retrieved from PubMed and CINAHL. In addition, relevant articles from the Internet or reference lists of articles and books, and other sources were included. Several methods and ways of approaching the discussion of ethics, and the implementation of ethics work in nursing homes, were identified. Frequently used methods and models to address ethical challenges were ethics peer groups, ethics consultation, or ethics committees. In conclusion, systematic ethics work in nursing homes is needed. The implementation should be individualized to meet different needs, as well as geographical and cultural conditions.
Cloning, Stem cells, Treatment, Moral problems
The development of biology, genetics, medicine, pharmacy at the end of XX century, bring along cloning of mammals, made the map of the human genome, genetic investigation and gene therapy reach new successes, assisted reproduction to become available procedure
“Respect for individual persons is the ethical thread that runs through the care of nursing home residents.” [1]
There are many ethical challenges in nursing homes, for example a lack of resources, coercion, autonomy, decision-making for residents without capacity, and end-of-life care issues [2-11]. Modern medicine has led to complex ethical challenges because of a greater number of people living with chronic illnesses, and the possibility to extend life using continually invasive therapies such as tube feeding, dialysis and respiratory therapy – even at home [12]. As the population of elderly and people suffering with dementia is increasing worldwide [13] the need for surrogate decision-making in nursing homes is also increasing. In advanced dementia, residents can no longer make their own decisions, so physicians, nurses and relatives have to make them on the residents’ behalf. Often, these decisions are made without knowing the resident’s true wishes because of a lack of advanced care planning (ACP), and inadequate preparatory conversations about their wishes and preferences for the end-of-life [14,15].
However, decisions to withhold or withdraw lifesustaining therapy cannot be based on medical fact alone, but must respect the patient’s own values and wishes. In people with advanced dementia, ACP, ethics consultation or ethics committees can be useful decision-making tools [16,17]. Daily, systematic ethics work in nursing homes is needed, yet is not standard in many nursing homes [5,11]. The term ‘systematic ethics work’ has been defined as “the organization’s systematic use of different measures, tools and places to enhance ethics discussions and ways to handle ethically difficult situations and choices in nursing homes, e.g. ethics education, ethical deliberation, different arenas for ethics discussions, ethics consultants and ethics committees.” [11].
The aim of this article is to provide an overview of different approaches to implement systematic ethics work in nursing homes. Challenges and obstacles in the implementation of systematic ethics work will also be addressed.
Using the databases PubMed and CINAHL, a selective literature search was carried out with a combination of the search terms: ‘nursing homes’, ‘long-term care facilities’, ‘implementation’ and ‘ethics’. In addition, relevant articles from the Internet, or from reference lists of articles and books or articles found via other sources as lectures or personal communications were included. Reflections on own experiences with implementation and research on systematic ethics work in nursing homes were also used to describe and discuss the topic.
Ethical challenges and dilemmas in nursing homes
Ethical problems in nursing homes are often more complex than those in hospitals [7,18,19]. There are two major groups of ethical issues in nursing homes. The first group can be described as “everyday ethical issues”, such as autonomy-related problems, informed consent, use of restraints, offensive behavior, or refusing medication, food and bathing [6,8,10,11,20]. The second group consists of “big ethical issues”, mostly dealing with life-or-death matters, such as decisions to withhold or withdraw life-sustaining treatment, including artificial nutrition and hydration [2,3,9,10,11,14,15]. According to Reitinger et al. [20] ethical issues can arise from situations such as admission to the nursing home, running away, bathing, conflicts with relatives, admission to hospital, treatment with nutrition and fluids, dying with dementia, or bereavement. Competence in decision making in patients with cognitive impairment, communication, shared decision-making with relatives, and issues about end-of-life care are often described in the literature as ethical challenges [2,5,10]. Whereas “everyday ethical issues” are important and need attention, the case discussions of ethics committees and ethics consultant teams mostly deal with “big ethical issues” such as withdrawal of life-sustaining treatment [2,21]. Staff members often describe end-of-life issues, lack of resources and coercion as frequent ethical challenges in nursing homes [9,11]. A recent study has shown that everyday ethical challenges seem to be most important from the residents’ point of view [22]. Another problem is the fact that in many Central European long term facilities, it is general practitioners who selectively provide medical expertise and treatment; some countries e.g. the Netherlands and Norway, are an exception to this in that they have specialized nursing home physicians. In many European long-term facilities, day-to-day treatment is mostly provided by caregivers and non-medically trained staff. These circumstances suggest that different methods of ethical communication are needed, other than the one commonly practiced in hospitals.
Strategies to handle ethical challenges in nursing homes
Places for both staff and patients to engage in discussion of ethical challenges should be established throughout primary care sites [23]; such discussions require inter-professional collaboration of all staff members, relatives and residents. Healthcare professionals should remember that the choice of treatment should be guided by what the resident would want and not what they would want for themselves [24]. Therefore, one important factor is to recognize, reconstruct and consider the wishes and values of the resident. In addition relatives’ views should be heard and taken into account. More timely and effective discussions about planning for the endof- life should be routine in nursing homes [14,15]. Planning for the end-of-life should be a process including continued discussions, rather than a single meeting where all future decisions are made at once. ACP should be the result of a series of such discussions [25]. Continuity of ethical communications involving the parties concerned is therefore crucial. Strategies for enhancing end-of-life discussions are most productively linked to the physicians’ interpersonal communication skills, a patient-centered model of care, a focus on the quality of remaining life, and innovative clinical models for implementing these discussions earlier in the care process [25].
Methods and ways of organizing systematic ethics work
Several methods and ways of organizing systematic ethics work are used or proposed to handle ethical problems in nursing homes (Box 1).
| (In)formal discussions |
| Reflection-groups (ethics peer groups) |
| Moral case deliberation |
| Ethics consultant/ethics team |
| Ethics committee |
| Ethics café |
| Ethics rounds |
| Gaming/role play |
| Advance care planning (as a tool to improve resident autonomy) |
Box 1. Methods to handle ethical problems in nursing homes
A systematic review on ethics support mechanisms concluded that ethics support is often connected to local contexts [26]. In present nursing home practice, informal or formal discussions between healthcare professionals (nurses and physicians) alone or with the resident and/or his relatives are often used [11]. Hayley et al. [1] suggested that most ethical issues in the nursing home could be resolved in an open discussion between the resident, relevant family members, legal advisors, the physician, and nursing home staff members. ACP and preparatory conversations [15,17,27] between residents, relatives, physicians and nursing home staff about the resident’s wishes and views about different treatment options and acceptable outcomes can be useful to avoid unnecessary life-prolonging treatments and hospital admissions. Reflection groups (ethics peer groups) and moral case deliberation (ethics reflection groups with an ethicist as facilitator) with colleagues or a multidisciplinary team are used in some nursing homes, e.g. in Norway and the Netherlands [28–31]. Staff from community health and elderly care services appreciate reflection groups as means to discuss ethical challenges, and the use of reflection groups can improve daily practice [28,30,31]. Use of an ethics consultant or a team of ethics specialists, who give advice or help with immediate consultations on a ward, is rarely used in nursing homes. The team can consist of members from the disciplines of social work, nursing, medicine and administration [21]. In general, nursing home ethics committees fulfill the same tasks as hospital ethics committees, even though they are often made up differently and known for being less attached to specific hospital ethics committees. Their tasks are education, case review and analysis, and policy development [2,7,18,24,32–34]. A survey of nursing home ethics committees in the USA revealed that, of the 29% who responded, few (8%) had established ethics committees. Their tasks were policy review (in 81%), advisory case review (67%) and education (45%) [18]. Ethics cafés [35,36] aim at discussing ethical issues with different groups (physicians, nurses, residents and relatives). The discussion is usually led by a moderator, often a professional ethicist, who encourages the discussion. This approach is called “Mäeutik” [35]. Ethics rounds [37] are meetings for healthcare professionals, residents and relatives, which aim at encouraging a dialogue across disciplines, education, and discussion of ethical issues for a broad range of people. Gaming and role-play have been used as educational tools for health care professionals and other nursing home staff. By acting out different roles, one may enhance the understanding of others’ values and positions, including the difficulties and dilemmas involved in decision-making related to long-term care and care for the elderly [38].
Development in Norway
In 2007 the Norwegian Association of Local and Regional Authorities (Kommunesektorens organisasjon, KS) started a series of projects to raise competence in ethics, and to implement reflection on ethics or ethics committees in nursing homes [39]. Examples of ethical tools used in these projects are an ethics handbook [40], and simple methods as the “traffic light approach” or “take a card” to discuss ethical challenges in a group. Furthermore an elearning program for learning and discussing ethics in a peer group has been developed [39]. An evaluation of this Norwegian project showed that there is a need for competence in ethics and systematic reflection beside support from the municipality [29].
Challenges of implementation of ethics work in nursing homes
The first step in dealing with ethical dilemmas is to be aware of the ethical aspects of a given situation and to recognize a problem as an ethical one: “…critical appraisal in ethics needs training in ‘you don’t perceive what you don’t perceive.’” [23]. Another challenge is that situations which do not necessitate immediate medical action are not considered ethically relevant. Examples might be the staff situation, the great lack of time, or the implementation of processes according to mere economic standards, which often means a direct contrast of caregiving standards.
Issues concerning organizational ethics usually need to be dealt with in a different context, where leadership should also be involved. Organizational ethics is the ethics of the whole organization and is interdependent with the organization’s culture [41]. To implement systematic ethics work in nursing homes it is paramount to sensitize and educate the whole nursing home staff (including those working in administration, technical personnel, and others who do not work at the bedside), but probably also residents, relatives and the public, about the importance of ethical issues in the care of the elderly. To reach that many people will involve a huge effort, since teaching and education is a challenge in terms of resources, time, and organization. One of the many obstacles in the implementation of systematic ethics work in nursing is a lack of resources. To implement ethics education and ethical reflection in nursing homes, time and financial support is needed. In times of cost effectiveness and economical restraints one should remember that: “Ethics cost, whether you have them or not” [42].
Obstacles of implementing ethics work in nursing homes
Organizational change is always a challenge and is accompanied by many obstacles. There will always be people who are afraid of change, and who will use a variety of arguments against systematic ethics work. Some of the most frequently used arguments against ethics consultation are [43]:
• “There is not enough time.”
Indeed, sufficient time is needed to establish systematic ethics work. However, discussions about ethics are likely to help save time since conflicts that are not properly addressed may cost yet more time and lead to communication problems, burn-out, etc.
• “Disturbance of the trustful relationship between physician and patient.”
Physicians might be afraid of others making “their decisions”; however, a multidisciplinary discussion helps to ensure that different points of view are taken into account. Ethics consultation can lead to a recommendation based on ethical deliberation. The physicians are still responsible for their decisions, but they can then be based on a thorough investigation of all aspects of the case.
• “More unnecessary bureaucracy.”
Many healthcare professionals are afraid of more paperwork and more meetings instead of working with patients. Ethics consultation can be offered and used voluntarily. The needs of patients, relatives and health care professionals shall be at the center of ethics consultation, which should be a tool in make good decisions. Information from the staff, patients and relatives can be used to clarify the aims and the process of ethics consultation.
• “Something that only the management wants.”
If a top-down model of implementation is used then employees might get the impression that ethics consultation is something desired only by management. A combined top-down and bottom-up approach can help to include all employees in the implementation process. Joint efforts between the management and interested employees have a greater chance of leading to sustainable changes within an organization. Presumptions for ethics consultation should be trustworthiness, acceptance, competence and independence.
Another obstacle may occur if healthcare personnel are afraid to highlight a case with ethical problems because of a fear that this could lead to negative consequences for themselves or their organization. A common misunderstanding is that an ethics committee is a court that makes decisions in case of conflicts; i.e. it is often misinterpreted as an attempt to sue someone. To avoid such misunderstandings, information is needed about the work of ethics committees to reassure staff that they do not make decisions; rather they reflect on ethical aspects of possible decisions, and give advice to the ones who have to make those decisions, e.g. physicians and residents.
Many methods to handle ethical problems, and ways to organize ethics work in nursing homes, are described in the literature. These are introduced in the Results section and an overview is shown in Box 1.
Different methods and approaches to systematic ethics work
A combination of different approaches to systematic ethics work is likely to be most useful, for example, discussion groups on the wards, and ethics committees where people are able to transfer certain problems to a higher level of ethics competence, or to reflect with a broader perspective. Systematic ethics work may be implemented using different measures, tools and places to enhance ethics discussions and ways to handle ethically difficult situations and choices in nursing homes [11]. There is evidence that different methods, for example ethics reflection groups, or moral case deliberation to discuss and reflect on ethical challenges can be useful in nursing homes [2,7,9–11,18,19,21,26,28–32]. If ethical challenges are complex and local ethics discussion does not lead to a consensus about a certain case, it could be helpful to have an ethics committee to discuss the case [18,32]. The best option must be adapted to suit local needs.
Based on a review of the literature and the authors’ experiences, our suggestion is a three-step approach to ethical decision-making in nursing homes (Figure 1, modified and adapted from [10]). The steps can be individualized to meet different needs as well as geographical conditions. For a small rural nursing home, education and open discussions might be a good start, whereas large institutions in big cities might need their own ethics committee or ethics consultation team. It is possible to use all three steps in one nursing home. A model of good practice for systematic ethics works, which includes all three steps shown in Figure 1, is the Caritas Socialis (CS) in Vienna, Austria, which has nursing homes, palliative care and home care services [44, p. 146–150]. The CS has successfully included systematic ethics work throughout the whole organization since 2007, and frequently uses ethics meetings with residents to aid decision-making for frail residents [11,44]. In Norway in 2006, Bergen Red Cross Nursing Home established its own ethics guidelines [45].
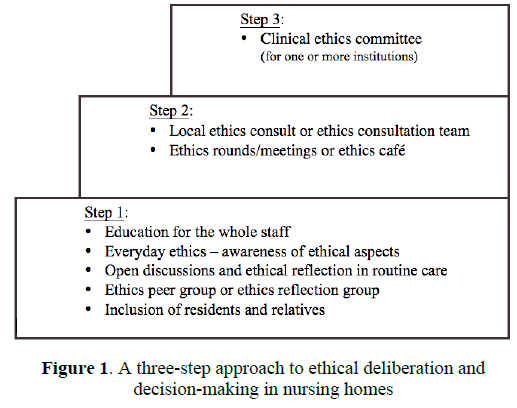
Figure 1: A three-step approach to ethical deliberation and decision-making in nursing homes
Planning the implementation of systematic ethics work in nursing homes
The organization of ethics consultation should be clarified before its implementation in the nursing home. It is necessary to discuss the following questions [43, p. 71–-75]:
• Who shall be able to ask for an ethics consultation (staff, resident, relatives, others)?
• Who will be the secretary and coordinator for the meetings?
• Who decides if the issue is relevant to be discussed in an ethics consultation, or if it should be discussed elsewhere?
• Who shall participate in case reflections?
• Which method shall be used for ethics reflection?
• How shall the results be documented?
These considerations underline that there is much work to do before one can start ethical case discussions. The usual tasks (education, development of guidelines and case review) should be defined, and a decision made as to whether they will be performed within the organization, or if there might be a need to collaborate with others. In other words, Step 1 and Step 2 of the three-step approach (Figure 1) may be used in small nursing homes, whereas to implement Step 3 might mean establishing a joint ethics committee together with other nursing homes. This approach has been used in Oslo, Norway, and in Frankfurt, Germany [46,47].
Views of the residents, relatives and nursing home staff
Before implementing an ethics process it may be wise to explore the views and needs of the staff, the residents, and their next of kin. But what do leaders and nursing home/homecare services staff want? Staff members and leaders from Norwegian nursing homes and primary care services want ethics education for health care personnel and administrators, meeting places, and time to discuss ethical problems in order to improve systematic ethics work [5,9,11]. A recent study found that only 18% of nursing home staff members consider internet-based learning a meaningful option in ethics education [11]. This is in contrast to the finding that internet-based learning is growing and is included in university ethics courses. One approach used in Norway is an Internet-based course that can be used by groups of healthcare personnel to facilitate ethics education and discussion [48]. This option likely spreads education using the Internet, and – importantly – ensures that groups can have a dialogue. Use of Internet platforms in ethics discussions may become more frequent in the future. An obstacle against the use of the Internet is that many of the staff in Norwegian nursing homes at present are not familiar with the Internet as an educational tool.
Factors for successful implementation
An essential factor for the successful implementation of systematic ethics work is that the management encourages and supports the work [29,30]. If a project starts from a bottom-up approach, one must try to involve the management at as early a stage as possible. In our opinion, the combination of a topdown and bottom-up approach, with assignment and support from management and inclusion of the employees, is the best option to make implementation and organizational change possible and durable. Ethics must become a part of the everyday life of the organization, and will lead to change the organization as a whole. Some authors use the term ‘organizational ethics’ for this type of common ethics within an organization such as a nursing home or hospital [41]. To ensure a change and a common concept of organizational ethics within ones own institution, discussion about values and ethics education are cornerstones of the implementation process. Residents and their relatives should be encouraged to participate in ethics discussions whenever possible. A recent study from our group has shown that relatives participate in ethics meetings, whereas the residents themselves usually do not [11]. To our knowledge, the residents are often excluded from ethics meetings. Reasons for that may be that staff members are afraid that the experience might be harmful or irritating for the residents. One major challenge for the future will therefore be to include both relatives and residents in ethics discussions and ethical decision-making in nursing homes [11].
Summary and suggestions for the implementation of systematic ethics work in nursing homes
In summary, implementation of ethics in nursing homes is both needed and possible, as Weston et al. [2] have already shown. The implementation of systematic ethics work can help to ascertain the resident’s wishes, and enable the physician, staff and others to discuss ethical problems in the course of decision-making. Hopefully this could lead to a reduction of conflicts between the resident, their relatives, care staff and the physician, and greater complicity with the resident’s wishes regarding their treatment and care. Possible outcome measures could be the number of cases in which consent could be reached with ethical deliberation, or the percentage of people who perceive that they have reached a “good decision”. Good decisions may be reached more often if options and ethical issues are discussed openly before making a decision. Experiences from Austria have shown that consensus about a practical solution was reached in each of 29 cases in which a resident ethics meeting was held [11]. As there is not, as yet, a gold standard protocol for the implementation of systematic ethics work and ethical deliberation in nursing homes, research must be an essential part of the process. Different approaches in different regions should be investigated in order to learn more about the topic. Surveys from nursing homes should be combined with qualitative, in-depth interviews in order to evaluate the different approaches, such as ethics peer groups/reflection groups, ethics consultation services, and ethics committees. Interviews with nursing home residents and relatives help us to learn more about their views and wishes regarding ethical challenges and decision-making in nursing homes [15,22]. Nursing home residents are most concerned about “everyday ethical issues” [22]. From our point of view there are three key factors for the implementation of systematic ethics work, which are the same as those described for the implementation of palliative care in nursing homes (Figure 2 modified from [49]). These include: 1) education and qualification of the whole staff; 2) to receive an assignment and support from the management; and 3) a change in the organization’s culture. These key factors must be taken care of to ensure a smooth process and sustainable success.
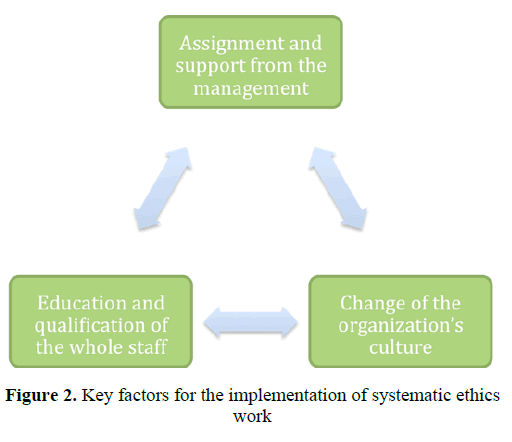
Figure 2: Key factors for the implementation of systematic ethics work
Suggestions for the implementation of systematic ethics work in nursing homes, and methods to handle the described challenges and obstacles that arise during the course of the implementation process are to:
• Receive an assignment and support from the management (e.g., resources, time)
• Use a combination of a top-down and bottom-up model
• Define tasks and the structure of systematic ethics work:
ο Usual tasks are education, case review, and development of guidelines
ο A combination of education and case review might be reasonable in the initial phase
• Raise awareness about ethics: education for all, including all personnel, patients, relatives and other interested parties from the community
• Provide information about ethics and the local structures to staff, patients and relatives:
ο Is an ethics consultant or ethics committee available?
ο Who can be contacted?
ο Information folder?
• Include residents and their next of kin
• To ask questions has to be acceptable within the organization
ο Ethics can be viewed as the question about what is best for those involved and affected
• Conduct research as part of the implementation process
Many ethical problems occur in nursing homes, where there is a lack of systematic work in the field of ethics. Ethics peer groups, ethics consultation, or ethics committees could help to solve many ethical dilemmas in this setting. A broader inclusion of the residents’ and relatives’ perspectives, and open discussions about “everyday ethical issues” (e.g. the use of restraints) as well as “big ethical issues” (e.g. decision-making in end-of-life care) are needed. The implementation should be individualized to meet different needs, as well as geographical and cultural conditions. A three-step approach to ethical decisionmaking in nursing homes has been proposed, and suggestions for the implementation process are given. As there is currently no gold standard for systematic ethics work in nursing homes, research should be an integral part of its implementation.
Citation: Bollig G, Rosland JH, Heller A (2016) How to implement systematic ethics work in nursing homes? Advances in Medical Ethics 3:1.
Received: 02-Apr-2015 Accepted: 29-Nov-2015 Published: 01-Jan-2016 , DOI: 10.35248/2385-5495.2016.3.1
Copyright: © 2016 Bollig et al.
Competing interests: The authors have declared that no competing interests exist.
Sources of funding : GB´s PhD-project on ethical challenges and decision-making in nursing homes has been financially supported by the Norwegian Extra Foundation for Health and Rehabilitation through EXTRA funds (grant no. 2008/2/0208).