
Advances in Pediatric Research
Open Access
ISSN: 2385-4529

ISSN: 2385-4529
Research - (2024)Volume 11, Issue 3
Nigeria is the largest country in Africa in terms of its population and economy, and has innovative policies, strategies and investments to improve child survival and development. Despite these efforts, approximately 12 million Nigerian children aged under 5 years are stunted and 3 million are suffering from wasting. In response to this child malnutrition crisis, United Nations International Children's Emergency Fund (UNICEF) partnered with the government of Nigeria and public-private partners to develop and implement the Nigeria-UNICEF country programme of cooperation (2018-2022), with nutrition as part of the child survival component.
The impact assessment within the pilot states has been performed using the primary data collected across seven states using an holistic questionnaire (51) developed for this purpose covering a sample of 5,600 households. We also supplement the analysis with findings from our nationwide historical impact evaluation using secondary data. Key objectives of the evaluation were to determine the programme’s merit based on expected results and impact; and the effectiveness of multisectoral interventions for addressing child malnutrition.
Quantitative findings of the multi variate statistical analysis of the HH primary data collection reveals that the pilot multi sectors community based nutrition programme implemented in selected states, has contributed to decrease the prevalence of stunting in children under five years. There are many factors that may simultaneously contribute to this finding, such as caregiver attitudes and knowledge, WASH and housing conditions and broader socioeconomic empowerment. Committee for Programme and Coordination (CPC) programme activities improved children’s anthropometric measurements by reducing stunting and underweight cases. The CPC programme impact evaluation yielded a statistically significant 3 percentage-point reduction in both stunting (z<-2) and severe stunting (z<-3) and a 3 percentage-point reduction in underweight children (z<-2). These impacts translate to small, standardized impacts of 0.06 (likelihood of stunting) to 0.07 (likelihood of underweight) standard deviation impact. However, we did not find any impacts on the overall length-for-height z-score or for the overall weight-for-height z-score. This contrast suggests that the CPC Programme was most effective at improving anthropometric outcomes for the most stunted and underweight children.
But we can conclude that the programme impacts were concentrated amongst children who otherwise would have been stunted since better nourished children-that is, those with z-scores greater than (-2)-did not see a corresponding boost. We did not find any impacts on child wasting or body mass index. We also saw that only 4% of the children in the treatment group received treatment for undernutrition, even though stunting prevalence exceeded 30% and underweight prevalence exceeded 20%.
However, the prevalence of wasting has increased during the period due to the negative impact of Coronavirus Disease of 2019 (COVID-19) on household food insecurity, poverty and increased inflation, as well as physical insecurity in the north of the country. Delivering a multisectoral programme to support nutrition proved challenging and many stakeholders have concerns about the government’s capacity to sustain the progress that has been achieved.
Nutrition; Child malnutrition; Nigeria; United Nations International Children's Emergency Fund (UNICEF); Maternal and child nutrition
AIR: American Institutes for Research; ANC: Antenatal Care; CMAM: Community-based Management of Acute Malnutrition; CPC: Country Programme of Cooperation; DID: Difference in Difference; EBF: Exclusive Breastfeeding; FGD: Focus Group Discussion; IMAM: Integrated Management of Acute Malnutrition; IYCF: Infant and Young Child Feeding; KII: Key Informant Interview; LGAs: Local Government Areas; MAM: Moderate Acute Malnutrition; MICS: Multiple Indicator Cluster Survey; MNCHW: Maternal, New-born and Child Health Weeks; MUAC: Mid-Upper Arm Circumference; NDHS: Nigeria Demographic and Health Survey; NGO: Non-Governmental Organization; NMPFAN: National Multisectoral Plan of Action for Food and Nutrition; OECD DAC: Organisation for Economic Co-operation and Development’s Development Assistance Committee; PHC: Primary Health Care; RUTF: Ready-to-use Therapeutic Food; SAM: Severe Acute Malnutrition; SDG: Sustainable Development Goal; WASH: Water, Sanitation and Hygiene
Nigeria has the largest population and economy in Africa, yet its health and nutrition indicators lag behind many others [1]. Despite economic growth, under-five mortality remains high. Nigeria accounts globally for about 10% of all deaths of children aged under 5 years. The country has the highest number of undernourished children in Africa and the second largest in the world after India. A total of 12 million Nigerian children aged under 5 years are stunted and 3 million are suffering from wasting. Rural areas, especially in the north, face challenges in healthcare access and nutrition outcomes. An estimated 9.3 million people, including 5.7 million children, are affected by conflicts in states in the North East, North West and North Central (Benue State) regions. Stunting prevalence among children aged under 5 years is 33% at the national level, but there are wide regional disparities with the highest levels of stunting in the North West (48%) and the North East (35%). Family livelihoods and child nutrition are highly affected in Nigeria by the negative impact of physical insecurity and the COVID-19 pandemic that resulted in huge food insecurity, inflation of food prices, household poverty, reduction of purchasing power and multiple child deprivations [2-12].
Recent improvements in undernutrition determinants in Nigeria have not resulted in considerable reductions in undernutrition: Wasting prevalence halved between 2008 and 2018 and stunting declined by 9.4%, but maternal undernutrition did not improve [13]. Similarly, while there were improvements in Exclusive Breastfeeding (EBF), Vaccinations, Antenatal Care (ANC) and other health services, some elements such as food security and child illnesses deteriorated. The country also has high levels of micronutrient deficiencies, primarily vitamin A, iodine, iron, folic acid and zinc, but coverage rates of micronutrient supplementation and fortification remain generally low, despite their cost effectiveness. An estimated 30% of Nigerian children and 20% of pregnant women are vitamin A deficient, while 76% of children and 67% of pregnant women are anemic. Only 34% of Nigerian children are exclusively breastfed and just 12% consume the recommended minimum acceptable diet [13,14].
Nigeria's healthcare structure operates at three levels, with the Federal Ministry of Health and the Federal Ministry of Finance playing key roles in policy and coordination [15]. However, challenges persist, including a poorly functioning public health system, high healthcare costs and low health facility delivery. The primary healthcare system faces operational hurdles and access to health services remains low and inequitable: Nine out of every ten women in urban areas received ANC from a skilled provider, while only six out of every ten women received ANC from a skilled provider in rural areas [2-4,16-20].
To combat malnutrition, the government has implemented various measures, including the creation of the National Council on Nutrition and the development of strategic plans [21]. However, policy implementation remains a challenge due to factors such as poor governance, lack of coordination and capacity constraints at the state and local levels. Effective programming, encompassing both nutrition-specific and nutrition-sensitive interventions, is important to improve nutrition outcomes. Nigeria needs interventions targeting dietary diversity, nutrient supplementation, healthy breastfeeding and improvements in the healthcare system [22-25].
In response to these needs, UNICEF partnered with the government and other agencies to develop the Country Programme of Cooperation (CPC) 2018-2022 [20]. The CPC focuses on child survival and development, with a significant budget allocated to nutrition interventions. It supports strengthening health and community systems, integrating nutrition into primary health care and addressing immediate and underlying causes of malnutrition. The programme’s main strategic outcome was to increase the access of vulnerable children, adolescent mothers and women to quality services and information for preventing and treating malnutrition. The Nutrition CPC worked across three inter-related areas to achieve this: (i) policies and planning; (ii) service delivery and community outreach; and (iii) humanitarian relief. The CPC targets caregivers, pregnant and lactating women and adolescents in poor, rural regions, particularly in northern Nigeria. UNICEF and the government have focused on interventions such as Community-based Management Of Acute Malnutrition (CMAM), Infant and Young Child Feeding (IYCF) interventions, micronutrient supplementation and multisectoral integrated packages in their goal to reduce stunting, wasting and child mortality.
This evaluation employed a mixed-methods approach to assess the government-UNICEF nutrition component (2018-2022), encompassing both nationwide programmes and a pilot of multisectoral integrated interventions in seven states (Bayles, Borno, Enugu, Jigawa, Niger, Oyo and Sokoto) is seen in Figure 1. A comprehensive approach combining secondary data analysis and primary quantitative evaluation was adopted to provide a robust assessment of the CPC nutrition component's impact and effectiveness, informing future programming and policy decisions. The secondary data analysis leveraged existing data sources, including the Nigeria Demographic and Health Survey (NDHS) reports and UNICEF's Multiple Indicator Cluster Surveys (MICS), to analyze trends and impacts on key anthropometric outcomes at the national level. In addition, a primary quantitative evaluation was conducted at the community level to specifically assess the effectiveness of the multisectoral integrated interventions pilot in seven selected states. The programme combined multiple interventions, such as agriculture, child protection, livelihoods, social protection (cash transfer) and Water, Sanitation and Hygiene (WASH).
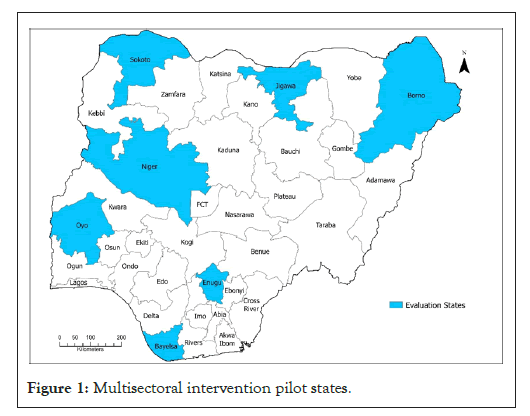
Figure 1: Multisectoral intervention pilot states.
Sampling strategy
A two-stage sampling was adopted so that LGAs were first selected as the main sampling unit and wards/communities selected as the secondary sampling units. Since treatment was purposively assigned to LGAs by stakeholders, comparison LGAs were matched to treatment LGAs as previously described. At the second stage, we randomly selected communities/wards. Within each community/ward, the required number of households were selected based on the number of eligible households i.e., households with at least one child aged under 5 years.
Power calculation and sample size determination
The sample size included 800 households per state-400 households in treated areas and 400 households in comparison areas. In total, there were 36 LGAs (noting that for Jigawa, the treated and comparison wards were from the same LGAs but were treated as separate geographic units). Based on a conservative assumption of one eligible child per household, we measured height and weight of 5,600 children, taking three measurements of each to minimise measurement error. Power calculations showed that, by using this strategy, there was an 80% chance of detecting an effect of 0.26 standard deviations improvement in height-for-age z-scores when we assumed an intraclass correlation of 0.09 for households clustered at the LGA level, based on undernutrition outcomes in MICS data.
Selection of households and respondents
Households were selected using a simple random approach. A household listing at the community level where such existed, was used to identify households with at least one child aged under five and randomly selected the required number of households. However, in cases where the household listings did not exist, field staff conducted a listing exercise in collaboration with the community leader and eligible households were randomly selected from the listing. A household was defined as a person or group of persons, related or unrelated, living together in the same dwelling unit. This included monogamous and polygamous households headed by either males or females.
The quasi-experimental design approach compared differences in outcome and impact indicators at end line across the programme participants and non-participants, using Coarsened Exact Matching (CEM) and multivariate regression analysis. A cluster-robust standard errors was used to account for clustering of households within LGAs. In addition to ordinary least squares regression analysis, we calculated the normalised difference in time-invariant outcomes to examine balance. We controlled for any variables unaffected by the intervention that have a normalised difference of more than 0.25.
Data management
Impact evaluation was estimated with a quasi-experimental design using a generalized Difference-in-Differences (DID) approach. This approach compares changes in outcomes for children residing in programme states (treatment group) to those in non-programme states (comparison group). The DID design leverages two key features to mitigate bias in impact estimation.
• Pre and post-treatment measures: By utilizing data collected before and after programme implementation, we control for time-invariant household or individual characteristics that may influence outcomes, such as proximity to markets or health facilities, agricultural activity, pre-existing medical conditions and unobserved nutritional practices. This allows researchers to isolate the programme's impact from these confounding factors.
• Comparison group as counterfactual: T he change in outcomes observed in the comparison group serves as a counterfactual to account for general trends in the population that are unrelated to the programme. This helps to ensure that any observed changes in the treatment group are truly attributable to UNICEF interventions.
Treatment and comparison states
States were classified based on the timing of UNICEF programme implementation. Treatment states were those receiving current UNICEF support through various programmes (e.g., vitamin A supplementation, CMAM, IYCF). Comparison states were those that had received some form of UNICEF support in the past but might not be currently receiving it. This quasi-experimental DID approach, coupled with careful selection of treatment and comparison states, strengthens the internal validity of the evaluation, allowing us to draw more confident conclusions about the impact of the UNICEF nutrition programmes on a national scale.
Difference-in-Difference (DID) analysis: To assess the impact of nationwide UNICEF nutrition programmes, we employed a Difference-in-Difference (DID) analysis. This approach compares changes over time in child outcomes and impact indicators between programme states (treatment group) and non-programme states (comparison group). We graphically depicted average outcomes over time at both national and state levels for descriptive purposes.
In addition to the DID analysis, descriptive statistics and trend analyses were conducted, including mean, median, standard deviation and minimum and maximum values by state. Data were further disaggregated by child gender, urbanicity, socioeconomic status, mother's education, crisis locations and wealth status to examine potential disparities in programme impact across subgroups. We also provided descriptive evidence on the health system's capacity to finance nutrition programmes at regional levels and its responsiveness to children's nutritional needs.
DID regression specification: The DID analysis controlled for general trends in child malnutrition and state-specific characteristics. The regression specification used to estimate the intent-to-treat effect of the programme on key nutrition outcomes was shown in Figure 2.
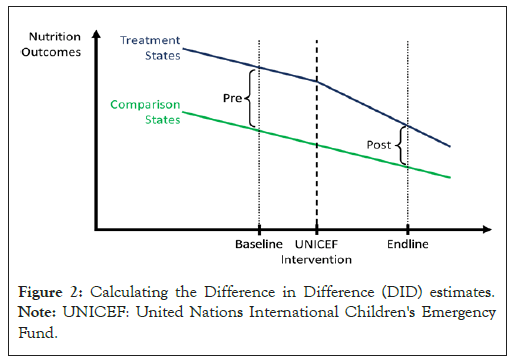
Figure 2: Calculating the Difference in Difference (DID) estimates. Note: UNICEF: United Nations International Children's Emergency Fund.
Where, yhct: Outcome of interest for child c in household h at time t; Treathc: Indicator variable (1 if child is in a UNICEF programme state, 0 otherwise); Postt: Indicator for observations taken from the end line period (t=end line); Chct: Set of child-level variables; Hht: Set of household-level variables; εhct: Unexplained model error; The key parameter of interest was α1, representing the programme's impact.
Limitations of the nationwide impact evaluation approach
The DID approach assumes no systematic, unobserved, time-varying differences between treatment and comparison states. If such differences exist (e.g., comparison states independently investing in malnutrition reduction), the programme's impact might be underestimated. While the large, representative sample of states should minimize average trend differences, pre-existing differing trends in programme states could bias the results. Additionally, past UNICEF support in comparison states might lead to downward bias in impact estimates. Thus, findings should be interpreted cautiously.
CPC programme impact evaluation in 7 pilot states
Data analysis: Researchers, we conducted a quantitative analysis of primary data collected to evaluate the impact of the multi-sector integrated interventions pilot on anthropometric characteristics for children. A cross-sectional, Coarsened Exact Matching (CEM) design was used to address potential differences between beneficiary and comparison areas. CEM improves match quality by approximating a blocked randomized controlled trial, enabling the study of nutrition outcomes within two groups that should have been similar without the intervention. This controls for observable differences due to background characteristics that would not change over time.
CEM approach and regression: CEM identifies similar pairs between beneficiaries and non-beneficiaries based on observable, time-invariant characteristics. Since beneficiary areas were selected due to higher malnutrition rates, CEM restricted the comparison sample to more food-insecure households for impact estimation.
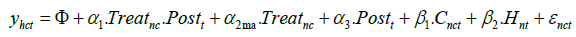
We used the cluster-robust cross-sectional regression to estimate the impact:
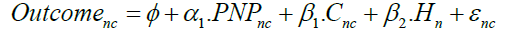
Where, Outcomehc: Outcome of interest for child c in household h; PNPhc: Indicator variable (1 if child is integrated package intervention eligible, 0 otherwise); Chc: Set of child-level variables; Hh: Set of household-level variables; εhc: Unexplained model error.
Standard errors were clustered at the LGA level to account for correlation of community-level conditions and implementation.
Treatment and comparison groups
The treatment group consisted of LGAs and wards in seven states where specific interventions were implemented. The comparison group comprised LGAs in those states that did not receive related UNICEF support but were matched to the treatment group based on observable characteristics.
Key indicators
Key indicators for the CPC programme impact evaluation included IYCF practices and anthropometric measures (stunting, wasting and underweight). The household survey contained additional domains included in the results seen in Table 1.
| Classification | Indicator | Age group |
|---|---|---|
| Anthropometrics | Percentage of children who are stunted | 0-59 months |
| Percentage of children who are underweight | ||
| Percentage of children who are wasted | ||
| Percentage of children who are severely wasted | ||
| Dietary diversification | Percentage of infants who are fed exclusively with breast milk | 0-5 months |
| Percentage of children provided with a minimum acceptable diet | 6-23 months | |
| Percentage of children who received a minimum number of food groups | ||
| Micronutrient supplementation | Number of children who received (a) vitamin A supplements in Semester 1; (b) vitamin A supplements in Semester 2 | 6-59 months |
| Percentage of children who received (a) deworming medication in Semester 1; (b) deworming medication in Semester 2 | ||
| Severe acute malnutrition | Percentage of children with SAM who (a) were admitted for treatment and recovered or (b) did not recover (death rate) | 6-59 months |
Table 1: Key indicators for the impact evaluation.
Limitations to the CPC programme impact evaluation analysis approach
A CEM design has three major limitations: Dealing with unobservable differences; dealing with time-invariant characteristics and eliminating observations that fall outside the common support. First, it was not possible to rule out unobservable differences that followed from the purposive selection of integrated package intervention states. The CEM approach relies on specifying all outcomes that would predict whether a household would receive this nutrition programming. Even with a well-executed design, there may be unobserved characteristics that create groups that were different before the programme had any impact. We mitigated this problem by carefully designing all data collection instruments to capture outcomes that predicted whether a household participated in the nutrition programme.
Second, matching households based on time-invariant outcomes (outcomes that do not change over time, for example, parents’ education or distance to a nutrition centre) is more difficult than matching on outcomes captured before the intervention, because pre-intervention outcomes would most directly capture household variation. Data collected before the intervention do not depend on treatment since the intervention would not yet have affected those values. However, an outcome collected after the intervention may have been affected by treatment and would introduce a bias if used in the matching process. Thus, nutrition outcomes collected after the intervention cannot be used in the matching process and data is limited to time-invariant outcomes.
Ethical consideration
The evaluation adhered to the standards of independent, impartial and credible research, free from conflicts of interest. The contractors AIR and Hanovia followed the United Nations Evaluation Group’s (UNEG) code of conduct, which requires adherence to the four ethical principles of integrity, accountability, respect and beneficence. The ‘do no harm’ principle was applied to ensure protection of children. Ethical approval was obtained from the AIR institutional review board and the National Health Research and Ethics Committee of Nigeria-(NHREC). Informed consent was sought from respondents and data security protocols were followed.
Overall performance evaluation of the effectiveness of nutrition programme
The evaluation shows mixed results for the CPC programme's impact on child nutrition in Nigeria as shown in Table 2. There is positive progress in exclusive breastfeeding, which increased from 25% to 38%; and deworming coverage which reached 35%. Other areas require improvement despite some level of progress recorded. Stunting declined from 37% but remains high at 30%, which is short of the desired target. Similarly, the prevalence of underweight has decreased from 20% but remains above the 15% target, with a 2022 result of 23%. The most concerning finding is the increase in wasting prevalence from 7% to 14%, significantly exceeding the 5% target. This alarming rise indicates a growing number of children suffering from acute malnutrition, which requires urgent attention to prevent further deterioration and mortality.
| Impact and outcome indicators | Indicator values | Evaluative judgement by the evaluation team | ||
|---|---|---|---|---|
| Starting value (2016 baseline) | 2022 target | 2022 results | ||
| 1) Impact (government commitment 2018–2022) | ||||
| 1.1 Prevalence of stunting (%) | 37% | 20% | 33.30% | Not achieved |
| 1.2 Prevalence of underweight (%) | 20% | 15% | 25.30% | Not achieved |
| 1.3 Prevalence of wasting (%) | 7% | 5% | 11.60% | Not achieved |
| 2) Outcomes (UNICEF 2018-2022) | ||||
| 2.1 Percentage of infants aged 0-5 months who were exclusively fed with breast milk | 25% | 57% | 34% | Partially achieved |
| 2.2 Number of children aged 6-59 months who received: (i) vitamin A supplements in Semester 1; and (ii) vitamin A supplements in Semester 2-key results for children (KR4C) indicator | 9,250,000 | 32 million | 23 million | Partially achieved |
| 2.3 Percentage of children aged 6-59 months with SAM who were admitted for treatment and recover | 88% recovery) (706,395 admitted) | 96% (363,344) | 93% (748,000) | Fully achieved |
| 2.4 Percentage of children aged 12-59 months who received: (i) deworming medication in Semester 1; and (ii) deworming medication in Semester 2 | 25% | 46% | 35% | Partially achieved |
| 2.5 Percentage of children aged 6-23 months provided with minimum acceptable diet | 25% | 21% | 11% | Not achieved |
| 3) Outputs (UNICEF 2018-2022) | ||||
| 3.1 Existence of a functional multisectoral committee for nutrition | Yes | Yes | Yes | Fully achieved |
| 3.2 Percentage of health facilities that provided treatment services for the management of SAM | 5% | 16% | 11% | Partially achieved |
| 3.3 Number of primary caregivers of children aged 0-23 months who received IYCF counselling | 618,050 | 1,373,186 | 1,253,080 | Partially achieved |
| 3.4 Existence of an emergency preparedness plan for nutrition | No | Yes | Yes | Fully achieved |
Note: SAM:Severe Acute Malnutrition; IYCF: Infant and Young Child Feeding; UNICEF: United Nations International Children's Emergency Fund.
Table 2: Nutrition Country Programme of Cooperation (CPC) results framework/indicator status.
The percentage of infants aged 0-5 months that were exclusively breastfed increased from 25% to 38%, showing positive progress but still far from the 57% target. This suggests that efforts to promote optimal breastfeeding practices need to be intensified. The recovery rate for children with Severe Acute Malnutrition (SAM) admitted for treatment was 45%, significantly below the 96% target. This points to potential gaps in the quality and effectiveness of SAM treatment services. The percentage of children aged 6-23 months receiving a minimum acceptable diet slightly decreased from 12% to 11%, indicating a need to improve dietary diversity and meal frequency among young children. These findings emphasize the need for targeted interventions and stronger programme implementation to address persistent challenges, particularly in reducing stunting, underweight, wasting and improving SAM treatment.
The CPC programme impact evaluation yielded a statistically significant 3 percentage-point reduction in both stunting (z<-2) and severe stunting (z<-3) and a 3 percentage-point reduction in underweight children (z<-2) is seen in Table 3. These impacts translate to small, standardized impacts of 0.06 (likelihood of stunting) to 0.07 (likelihood of underweight) standard deviation impact. However, we did not find any impacts on the overall length-for-height z-score or for the overall weight-for-height z-score. This contrast suggests that the CPC Programme was most effective at improving anthropometric outcomes for the most stunted and underweight children. But we can conclude that the programme impacts were concentrated amongst children who otherwise would have been stunted, since better nourished children-that is, those with z-scores greater than -2 did not see a corresponding boost. We did not find any impacts on children’s wasting or body mass index.
| Outcome | Impact | Treatment mean | Treatment N | Comparison mean | Comparison N |
|---|---|---|---|---|---|
| Length/height-for-age Z-score | -0.18 | -1.02 | 2,779 | -0.86 | 2,894 |
| Stunting (z<-2) | -0.03** | 0.3 | 2,779 | 0.34 | 2,894 |
| Severe stunting (z<-3) | -0.03*** | 0.14 | 2,779 | 0.18 | 2,894 |
| Weight-for-age Z-score | -0.13 | -0.92 | 2,779 | -0.81 | 2,894 |
| Underweight (z<-2) | -0.03** | 0.23 | 2,779 | 0.26 | 2,894 |
| Severe underweight (z<-3) | -0.01 | 0.08 | 2,779 | 0.09 | 2,894 |
| Weight-for-length/height Z-score | -0.05 | -0.6 | 2758 | -0.55 | 2,882 |
| Wasting (z<-2) | 0 | 0.14 | 2758 | 0.15 | 2,882 |
| Severe wasting (z<-3) | 0 | 0.05 | 2758 | 0.05 | 2,882 |
| BMI-for-age Z-score | 0.05 | -0.3 | 2779 | -0.34 | 2,894 |
| Ever treated for malnourishment | 0.01 | 0.04 | 2798 | 0.03 | 2,904 |
Note: BMI: Body Mass Index; (*): 10% significance; (**): 5% significance; (***): 1% significance
Table 3: Impact results on anthropometrics.
We also saw that only 4% of the children in the treatment group received treatment for malnourishment, even though stunting prevalence exceeded 30% and underweight prevalence exceeded 20% is seen in Table 3.
To place our findings from this research within the context of the larger changes in anthropometric measures of child nutrition, we considered the nationwide changes based on historical Demographic Health Survey (DHS), MICS and recent National Food Consumption and Micronutrient Survey (NFCMS) data. Figure 3, shows the historical trends for stunting, wasting and underweight, respectively and at both standard levels and severe levels. Each graph shows a steady, downward trend for the severely undernourished. Severe stunting falls from 23% to 17%; severe wasting falls from 9% to 1%; severe underweight falls from 12% to 10%. Time trends for standard measures of stunting, wasting and underweight were slightly less clear. Stunting fell by only about half of a percentage point; wasting decreased by about 7 percentage points and underweight increased by about 6 percentage points.
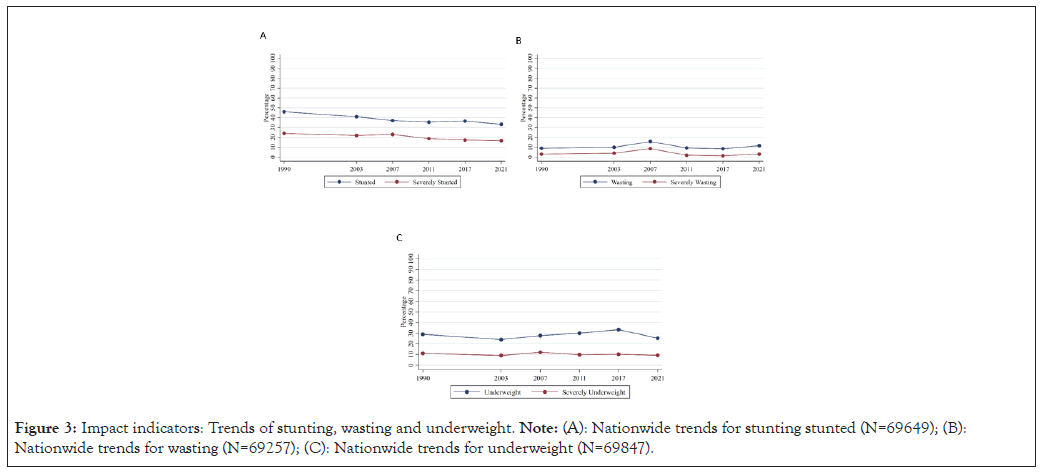
Figure 3: Impact indicators: Trends of stunting, wasting and underweight. Note: (A): Nationwide trends for stunting stunted (N=69649); (B): Nationwide trends for wasting (N=69257); (C): Nationwide trends for underweight (N=69847).
Regression analysis for the nationwide impact evaluation of nutrition programming tested whether any of the nationwide changes could be directly attributed to the programme but did not detect any statistically significant impacts. There is only one significant result suggesting an increase in malnutrition; however, this level of statistical significance is in line with the number of spurious cases to be expected due to random chance. One possible reason of non-effect is that UNICEF did not determine implementation locations in a vacuum. Rather, UNICEF implemented and supported nutrition programming in states where nutritional outcomes were susceptible to deteriorating over time.
Results show clear decreases for severe levels of undernutrition (z<-3) but mixed results for the lower standards for total undernutrition (z<-2), therefore it appears likely that the most undernourished Nigerian children moved from severe levels of undernourishment to less severe levels of undernourishment. The levels of undernutrition are similar but slightly lower in the sample used for the CPC programme evaluation, which validates the CPC programme’s goal of targeting areas with nutritional deficiencies. Findings shows that stunting, underweight and wasting in UNICEF’s present operating states are consistently higher than in the other states. Measures of undernutrition in UNICEF’s present states remain consistent, so the possibility remains that UNICEF’s support has prevented deteriorating conditions for children’s anthropometrics and state-level results of Anthropometrics as detailed in (Figure 4).
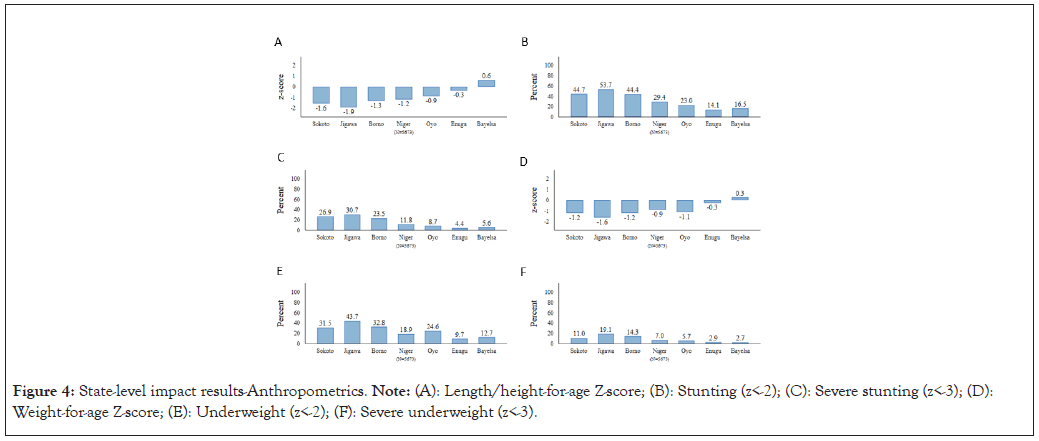
Figure 4: State-level impact results-Anthropometrics. Note: (A): Length/height-for-age Z-score; (B): Stunting (z<-2); (C): Severe stunting (z<-3); (D): Weight-for-age Z-score; (E): Underweight (z<-2); (F): Severe underweight (z<-3).
Impact of community-based, multisectoral integrated interventions in 7 pilot states
Table 4, shows the impacts on stunting and wasting. In the case of stunting, the overall -3 percentage point impact is driven primarily by the impacts measured in the Niger state, which shows an 11 percentage point decrease and Sokoto state, which shows a 17 percentage point decrease. By contrast, none of the other states have shown a statistically significant impact at even the 10% level. For stunting, we see that the overall statistically insignificant impact of the CPC programme evaluation holds for each of the seven states. Indeed, none of the states show a significant impact of the CPC programme on the likelihood that children are wasted. The states with the statistically significant reductions of stunting were two of the states with higher rates among the comparison group.
| States | Treatment stunting | Comparison stunting | Impact | Treatment wasting | Comparison wasting | Impact |
|---|---|---|---|---|---|---|
| Borno | 43% | 46% | -1 pp | 14% | 19% | -3 pp |
| Jigawa | 53% | 54% | 2 pp | 22% | 18% | 4 pp |
| Niger | 25% | 34% | -11 pp*** | 13% | 13% | -3 pp |
| Sokoto | 36% | 53% | -17 pp*** | 15% | 17% | 0 pp |
| Bayelsa | 18% | 15% | 2 pp | 11% | 12% | 4 pp |
| Oyo | 12% | 16% | -3 pp | 9% | 8% | 0 pp |
| Overall | 30% | 34% | -3 pp** | 14% | 15% | 0 pp |
Note: (*): 10% significance; (**): 5% significance; (***): 1% significance.
Table 4: State-level comparison of key impacts.
Equity at national level: UNICEF’s current nutrition programming in Nigeria takes place in the states that have historically had the worst undernutrition. Table 5, shows the prevalence of stunting, underweight and wasting in the states where UNICEF presently operates based on MICS data. Further, within UNICEF and non-UNICEF states, we see that the poorest quintile of households has a higher prevalence of undernutrition. UNICEF’s present focus on the states with the largest share of children facing undernutrition is an appropriate approach to promoting equitable nutrition outcomes in Nigeria.
| State | Stunting | Underweight | Wasting | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2007 | 2011 | 2017 | 2021 | 2007 | 2011 | 2017 | 2021 | 2007 | 2011 | 2017 | 2021 | |
| Poorest quintile UNICEF’s present states (19) | 50% | 53% | 59% | - | 38% | 45% | 53% | - | 21% | 13% | 11% | - |
| Poorest quintile other comparison states (18) | 35% | 43% | 44% | - | 24% | 34% | 34% | - | 13% | 9% | 7% | - |
| Richest quintile UNICEF’s present states (19) | 30% | 17% | 15% | - | 24% | 19% | 21% | - | 15% | 9% | 10% | - |
| Richest quintile Other comparison states (18) | 20% | 11% | 12% | - | 15% | 12% | 15% | - | 13% | 6% | 7% | - |
| National average | 37% | 35% | 37% | 33% | 28% | 30% | 33% | 25% | 16% | 10% | 8% | 12% |
Note: UNICEF: United Nations International Children's Emergency Fund.
Table 5: Prevalence of undernutrition in UNICEF focus states.
Equity within the integrated multisectoral interventions: Table 6, provides findings related to the nutrition’s programming in addressing inequality in childhood nutritional status when analysing the disparity for the top sextile, bottom sextile and the middle two-thirds of wealth. We do not find any indication that the CPC programme was any more likely to reduce wasting among children from wealthier and poorer households. For each of the three groups and impact on wasting is statistically insignificant as shown in Table 6.
| States | Treatment stunting | Comparison stunting | Impact | Treatment wasting | Comparison wasting | Impact |
|---|---|---|---|---|---|---|
| Self-assessed poorest sextile | 38% | 39% | 2 pp | 16% | 18% | -2 pp |
| Self-assessed middle-income sextile | 30% | 34% | -3 pp** | 15% | 14% | 2 pp |
| Self-assessed wealthiest sextile | 22% | 29% | -5 pp | 12% | 15% | -4 pp |
| Overall | 30% | 34% | -3 pp** | 14% | 15% | 0 pp |
Note: (*): 10% significance; (**): 5% significance; (***): 1% significance.
Table 6: State-level comparison of key impacts.
By contrast, we see that the overall impact of a negative 3 percentage points on stunting is driven primarily by the middle two-thirds of the wealth distribution, which also has a negative 3 percentage point impact. Children from the top and bottom sextiles both have results that are statistically insignificant. These findings suggest that the CPC programme equitably served children with different levels of wealth given the consistent results for children from the wealthiest and poorest families.
Evidence generated from this research confirms that the nutrition programme was a valuable quality important investment in addressing the high burden of child malnutrition in Nigeria. The programme’s focus on CMAM, IYCF initiatives, micronutrient supplementation and multisectoral packages tackled the four main factors from NDHS 2018 found to be driving malnutrition in Nigeria: Inadequate access to nutrition and health services; sub-optimal caring practices; a poor environment for young children and women during pregnancy and insufficient and poor-quality food [26].
CMAM programmes have proven effective in helping admitted children to recover from SAM and promoting prevention through community outreach and MAM management. Results of a 2012 CMAM evaluation in Ethiopia funded by UNICEF showed improved access and coverage as the number of SAM children treated annually increased from 18,000 in 2002 to 230,000 in 2012-more than 12-fold in a decade. Similarly, multisectoral collaboration between health and nutrition sectors enabled successful scaling up of vitamin A supplementation. Integrated routine and COVID-19 vaccines, vitamin A and birth registration campaigns were conducted in 33 states reaching 35 million children in 2022 in semester one [27-30].
The nutrition CPC was less effective in reaching its stunting and wasting targets, which is unsurprising given the low awareness (30%) and low coverage (20%) of the programme’s key activities. This aligns with other research showing nutrition intervention coverage in Nigeria to be low compared to the magnitude of need. Despite scale-up and improvements in the MNCHW package (from 2008-2019), coverage of most interventions was below 50% in the target population, too low to be effective. Intra-sectoral and multisectoral coordination were also potentially inadequate; Adeyemi et al., showed that 12% of children had received all three selected health sector interventions and 6% had received six selected multisectoral interventions for stunting reduction in Nigeria between 2008-2019 . Achieving and sustaining high coverage of effective multisectoral interventions remain the critical limiting factors for reducing malnutrition [31-34].
Nigeria is one of the 15 countries most severely affected by the current global food and nutrition crisis, in which only one in three children with severe wasting receive treatment [35]. Food and nutrition security in Nigeria were also impacted during the 2008-2010 global economic crisis, with food price increases affecting nearly every agricultural product in Nigeria without a corresponding increase in the disposable income of families and population groups (especially vulnerable groups). Programmes such as the nutrition CPC must address the determinants and drivers of undernutrition to have an impact on the more life-threatening forms of child wasting. This includes joint intervention packages for both wasting and stunting that overcome the humanitarian-development divide and aim to secure substantial, sustainable and predictable funding [36-39].
Analysis of Nigeria’s DHS data confirms the importance of addressing the socioeconomic inequalities and social norms and families practices that determine child stunting and wasting, especially wealth, maternal education and access to sanitation. A study of four Sahel and Horn of Africa countries with similar stubborn high levels of stunting and wasting (Burkina Faso, Ethiopia, Niger and Senegal) confirmed that negative social norms and cultural beliefs cause inadequate child feeding, nutrition and health care practices that facilitate disease and malnutrition [25].
UNICEF’s CPC programming provided necessary and impactful support that directly benefitted new-borns and young children. Undernutrition remains a persistent problem in Nigeria and represents a key focus of national and global nutrition goals. By supporting some of the solutions for undernutrition, the CPC programme improved the likelihood and frequency of infants receiving breastmilk and a more diverse diet. These successes carry over to physical measurements of children, reducing cases of stunted and underweight children.
The nutrition CPC achieved targets across a number of expected results, providing vital support that directly benefited new-born and young children aged 0-59 months during the first 1,000 days of life. At national level this included reaching 35 million children with vitamin A supplementation and over 2.5 million (80%) of children suffering from SAM were treated in UNICEF-supported states. By supporting IYCF services, the programme improved the likelihood and frequency of infants receiving breastmilk (extending duration by 0.33 months per child) and a more diverse diet.
The programme has not achieved its goal of a significant reduction in child malnutrition, with nutrition outcomes still languishing at low levels. Furthermore, delivering a multisectoral programme to support nutrition has proved challenging and many stakeholders have concerns about the government’s capacity to sustain progress that has been made.
Undernutrition (stunting, wasting and underweight) remains high in Nigeria and requires continued (and increased) investment. An evaluation of the country’s likelihood for achieving its SDG targets for child mortality and stunting reduction found that Nigeria was off-track. The main drivers were the very low level of public health financing (4% of Gross Domestic Product (GDP), the lowest in Africa), limited access, poor quality and weak local governance of PHCs, huge household out-of-pocket payment for health services and poverty. Numerous other factors such as COVID-19, increased food prices, insecurity and climate change aggravated household poverty and child vulnerabilities to malnutrition during the programme time period (2018-2022).
Key lessons learned are that nutrition programming that does not also address these underlying drivers of malnutrition like food insecurity and poverty may handicap the ability of stakeholders (government-federal and state, donors and communities) to accelerate improvements in reducing child malnutrition in Nigeria.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Ndamobissi R, Kutondo EE, Hodge AJ, Hajeebhoy N, Mitchell M, Ring H, et al. (2024). Impact and Equity of Five Years Multisectoral Investment to Improve Child Nutritional Status in Nigeria. Adv Pediatr Res. 11:084.
Received: 09-Aug-2024, Manuscript No. LDAPR-24-33733; Editor assigned: 12-Aug-2024, Pre QC No. LDAPR-24-33733 (PQ); Reviewed: 26-Aug-2024, QC No. LDAPR-24-33733; Revised: 02-Sep-2024, Manuscript No. LDAPR-24-33733 (R); Published: 10-Sep-2024 , DOI: 10.35248/2385-4529.24.11.084
Copyright: © 2024 Ndamobissi R, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.