
Advances in Pediatric Research
Open Access
ISSN: 2385-4529

ISSN: 2385-4529
Research Article - (2023)Volume 10, Issue 2
Background: Low birth weight is one of the critical issues in Ethiopia that causes many babies’ short- term and long-term health consequences. In Ethiopia, low birth weight is increasing; however, limited evidences of multilevel factors associated with low birth weight in the study setting, Ethiopia.
Objectives: The objective of this study was to assess individual and area level factors of Low Birth Weight in Ethiopia: from Ethiopia Demographic and Health Survey 2016.
Methods: The data were extracted from the 2016 Ethiopia Demographic and Health Survey. For analysis a sample of 2110 birth weights within five years preceding the survey were included. The analysis was carried out using STATA software version 14. A two level mixed effects logistic regression analysis was used to estimate both the fixed effects of the individual and contextual factors and the random effects of the between cluster difference. Adjusted Odds Ratio with 95% Confidence Interval to express measures of association and Intra Class Correlation to express measures of variation were used.
Results: A total of 2110 children nested within 445 clusters were included in the analysis. Among them, 13% were with low birth weight. The ICC implied 11.7% of the variance in low birth weight was attributable to Area level unobservable factors. At individual level; multiple birth (AOR=2.74; 95%CI: 1.450-5.184), preterm birth (AOR=4.83; 95%CI: 2.644-8.830), anemic mothers (AOR=1.49; 95% CI: 1.069-2.092), six and above birth order (AOR=0.42; 95%CI: 0.242-0.752), mothers with primary educational level (AOR=0.61; 95%CI: 0.418-0.896) and secondary/higher educational level (AOR=0.39; 95%CI: 0.252-0.612) as well as region from Area level were significantly associated with low birth weight.
Conclusion: The results of this study showed that multiple births, anemic mothers, birth order, not-educated mothers and preterm gestational age at birth were significant factors of low birth weight. Hence, switching off/on the significant factors accordingly could reduce the risk of having low birth weight child.
Community level; Ethiopian demographic and health survey; Individual level; Low birth weight; Multilevel analysis
Low Birth Weight (LBW), which is defined by the World Health Organization (WHO) as birth weight less than 2500 grams, is associated with a higher risk of neonatal and infant mortality and morbidity and a greater risk for adverse health outcomes, cognitive development and school performance problems than those born with normal weight. The subcategories of low birth weight are: Very Low Birth Weight (VLBW) which is <1500 gram, Extremely Low Birth Weight (ELBW) which is <1000 gram [1-3].
Low birth weight caused due to either preterm (before 37 weeks of gestational age) or Intra-Uterine Growth Retardation (IUGR) and poor health care during pregnancy. The IUGR is often as a result of maternal nutrition either before conception or during pregnancy as well as fetal problem [4].
Low birth weight has public health importance including increased neonatal mortality and morbidity, physical and psychomotor development delay. Besides infant LBW are more likely to develop significant disabilities and there are long term health implication of future chronic disease [4]. LBW due to restricted fetal growth affect the person throughout life and is associated with poor growth in childhood and a higher incidence of adult disease, such as type 2 diabetes, hypertension and cardiovascular disease. An additional risk for girls is having smaller babies when they become mothers [5].
Based on Literatures, the factors associated with premature delivery and low birth weight includes: socio economic status, maternal education and occupational, residence, maternal anthropometric status such as: maternal stature, Mid Upper Arm Circumference (MUAC) and multiple pregnancies [6,7].
Triggering LBW, previous history of preterm/LBW/IUGR, maternal age, birth interval, inadequate weight gain in pregnancy, infectious and improper nutrition are other predictors of LBW. From the maternal factors, stress, smoking and use of alcohol, pollution, violence and genetic factor are some of the determinant factors of LBW [8].
In 2012, the world health assembly resolution endorsed a comprehensive implementation plan on maternal, infant and young child nutrition, which specified six global nutrition targets for 2025. The third target of this policy briefly covers 30 percent reduction of LBW. The goal is to achieve a 30% reduction of the number of infant born with a weight lower than 2500 gram by the year 2025. This would translate in to 3.9 percent relative reduction per year between 2012 and 2025 [9].
Statement of the problem
About 20 million infants world-wide accounting for 15.5 percent of all births are born LBW, 95.6 percent of them in developing countries. In developing countries 16.5 percent of infants are born LBW, 13 percent in sub Saharan Africa. LBW is a major public health problem in under-resourced settings [10]. There are 15 million Preterm Birth (PTB) annually and more than 1 million of infants born preterm die due to early complications. The rate of PTB is increasing, particularly in sub-Saharan Africa and South Asia where over 60 percent of global PTBs occur [11].
Babies born low birth weight are 37 percent more likely to die during infancy compared to those of normal weight if other factors are held constant. Therefore LBW is strongly negatively associated with infant survival [12]. In a study conducted in East Africa, preterm babies and babies with LBW were found to account for 52 percent of newborn deaths in East Africa [13].
Being born with LBW is generally recognized as a disadvantage for the infant, family and country. Preterm birth is a direct cause of 28 percent of the 4 million neonatal deaths that occur globally every year. Direct or indirect, LBW may contribute to 60 percent to 80 percent of all neonatal death. LBW infant are at higher risk of early growth retardation, infection, developmental delay and death during infancy and childhood [14]. Studies have shown that infants weighing less than 2500 gram were approximately 20 times more likely to die than heavier babies [5].
Based on the united nation report in Ethiopia the prevalence pattern of LBW in 2000 GC was 15 percent but in 2005 GC report was 20.5 percent [15]. The pattern of LBW in Ethiopia was increased from 11 percent to 13 percent in 2011 and 2016 respectively. Based on a different researches done in Ethiopia was reported the prevalence of LBW in Addis Ababa 11 percent and in Jima 22.5 percent and Gondar percent and the prevalence of LBW in Tigray was 9.9 percent [3,15,16].
In Ethiopia, using a single level analysis, there are a lot of studies done on LBW, however; the multilevel factors associated with LBW, are not well addressed. For data with a hierarchical nature, using single level logistic regression can bias the parameter estimation. Multilevel models allow one to account for the clustering of subjects within clusters of higher-level units when estimating the effect of subject and cluster characteristics on subject outcomes and gives us appropriate parameter estimation for nested data.
Limited evidences are available regarding predictors of LBW in Ethiopia at nationally representative sample. So this study has taken a step further from the routine Ethiopian Demographic Health Survey (EDHS) report by further analysis of Demographic Health Survey (DHS) data using advanced analysis model to assess multilevel factors of LBW using a multilevel logistic regression model and provides context specific information to program planners and policy makers.
Objectives
General objective: To assess the individual and Area level factors of low birth weight in Ethiopia evidence from EDHS 2016.
Specific objectives: To identify the individual level factors associated with low birth weight in Ethiopia EDHS 2016. To identify the Area level factors associated with low birth weight in Ethiopia EDHS 2016.
Study area and period
Ethiopia is situated in the Horn of Africa with 9 Regional States and two city administrations. The capital city of Ethiopia is Addis Ababa. Study was conducted in all nine geographical regions and two administrative cities of Ethiopia which are included by EDHS 2016 [3]. Study period of this study is from May to December of 2018.
The current health policy of Ethiopia gives much more emphasis on prevention and the health promotion components of health care that should be able to resolve most of the health problems of the population [17].
Data source
The child dataset used for this analysis was the 2016 EDHS. It is the latest and the nationally large scale dataset of demographic and health survey that was conducted by the Central Statistical Agency (CSA) from January 18, 2016 to June 27, 2016 with nationally representative sample from 9 regions and two administrative cities. The total study participant to this study was 2110 infants whose weights were recalled. Details of sampling design and selection of sample are available in the Ethiopia Demographic and Health Survey 2016 EDHS reports (Table 1a) [3].
| Characteristics | Frequency weighed | % | Normal BW | LBW | LBW % |
|---|---|---|---|---|---|
| Religion | |||||
| Orthodox | 1006 | 47.7 | 871 | 135 | 13 |
| Protestant | 469 | 22.2 | 423 | 45 | 10 |
| Muslim | 620 | 29.4 | 522 | 98 | 16 |
| Others | 15 | 0.7 | 15 | 0 | 0 |
| Age of mother (in year) | |||||
| 15-24years | 536 | 25.4 | 470 | 66 | 12 |
| 25-34 years | 1208 | 57.2 | 1037 | 171 | 14 |
| 35 and above years | 366 | 17.4 | 325 | 41 | 11.2 |
| Member of at household | |||||
| 1-5 | 1299 | 61.6 | 1119 | 180 | 14 |
| 6 and above | 811 | 38.4 | 712 | 99 | 12 |
| Sex of child | |||||
| Male | 1077 | 51.1 | 960 | 117 | 11 |
| Female | 1033 | 48.9 | 871 | 161 | 16 |
| Sex of HH head | |||||
| Male | 1681 | 79.7 | 1476 | 205 | 12 |
| Female | 429 | 20.3 | 356 | 73 | 17 |
| Maternal age at 1st birth | |||||
| Less than 18 years | 557 | 26.4 | 479 | 79 | 14 |
| 18 and above years | 1553 | 73.6 | 1353 | 200 | 13 |
| Continued- Gestational age at birth | |||||
| Term | 2047 | 97 | 1797 | 250 | 12 |
| Preterm | 63 | 3 | 34 | 29 | 46 |
| Child is single or twin | |||||
| Single birth | 2045 | 96.9 | 1792 | 252 | 12 |
| Multiple birth | 65 | 3.1 | 39 | 26 | 40 |
| Marital status | |||||
| Not married | 20 | 1 | 17 | 2 | 15 |
| Married | 2090 | 99 | 1814 | 276 | 13 |
| Birth order | |||||
| 1-3 | 1535 | 72.7 | 1342 | 193 | 13 |
| 4-5 | 318 | 15.1 | 252 | 66 | 21 |
| 6 and above | 257 | 12.2 | 237 | 20 | 8 |
| Smokes cigarettes | |||||
| No | 2102 | 99.6 | 1824 | 277 | 13 |
| Yes | 8 | 0.4 | 7 | 1 | 13 |
| Anemia level | |||||
| Anemic | 399 | 19.9 | 333 | 66 | 17 |
| Not anemic | 1603 | 80.1 | 1397 | 207 | 13 |
| Mothers educational level | |||||
| No education | 609 | 28.9 | 498 | 111 | 18 |
| Primary | 803 | 38 | 714 | 88 | 11 |
| Secondary/higher | 698 | 33.1 | 619 | 79 | 11.3 |
| Maternal occupation | |||||
| Not Employed | 1253 | 59.4 | 1073 | 179 | 14 |
| Employed | 857 | 40.6 | 758 | 99 | 11 |
| Husband education level | |||||
| No education | 414 | 20.9 | 339 | 75 | 18 |
| Primary | 690 | 34.8 | 585 | 107 | 15 |
| Secondary/higher | 878 | 44.3 | 791 | 89 | 10 |
| Husband occupation | |||||
| Not employed | 904 | 45.6 | 747 | 157 | 17 |
| Employed | 1078 | 54.4 | 986 | 110 | 10 |
| Nutritional status | |||||
| Underweight | 289 | 14.2 | 233 | 56 | 19 |
| Normal | 1361 | 66.7 | 1176 | 185 | 14 |
| Overweight/obese | 390 | 19.1 | 355 | 35 | 9 |
| Wealth index | |||||
| Poor | 363 | 17.2 | 306 | 57 | 16 |
| Middle | 294 | 13.9 | 243 | 51 | 17 |
| Rich | 1453 | 68.9 | 1283 | 170 | 12 |
| Media exposure | |||||
| Not exposed | 713 | 33.8 | 611 | 102 | 14 |
| Exposed | 1397 | 66.2 | 1220 | 177 | 13 |
Table 1a: Low birth weight distribution by individual level characteristics, EDHS 2016, Ethiopia, 2018.
Study design
A cross sectional study design was used to identify multilevel factors associated with LBW from the 2016 EDHS data collected by the CSA.
Population
Source population: All live births in the five years born to women’s of reproductive age of 15-49 years who were residents of the nine regions and two administrative cities of Ethiopia during the survey.
Study population: All live births in the five years born to women’s of reproductive age of 15-49 years, who were residents of the selected households in the selected enumeration areas during the survey.
Sample population: All live births in the five years born to women’s of reproductive age of 15-49 years, who were residents of the selected HHs in the selected enumeration areas during the survey, Study population who fulfilled the inclusion criteria.
Eligibility criteria
Inclusion and exclusion criteria: All Birth Weighted infants in EDHS 2016 sampled areas were included in the study. All mothers who had not weighted their children and do not know their child’s weight were excluded.
Operational and standard definition: It includes,
• Normal Birth Weight (NBW): It is a weight class greater than or equal to 2500 gram.
• Low birth weight: It is a weight at birth less than 2500 gram.
• Individual level factors: A variable operating at the lowest level or individual level which included children’s, parents and household characteristics.
• Area level factors: The term Area refers to clustering of individuals within same geographic environment.
Sample size and sampling procedures
Each region was stratified into urban and rural areas yielding 21 sampling strata. Samples of Enumeration Areas (EAs) were selected independently in each stratum in two stages. In the first stage an enumeration areas 645 (202 urban areas and 443 rural areas) were selected. In the second stage of selection a 28 households per cluster were selected with an equal probability systematic selection from the newly created household listing. Overall, 18,008 households were selected of which 17,067 were occupied. Selected households were visited and interviewed. All women aged 15-49 years were eligible to be interviewed. Of all the child dataset related to birth weight, 2110 infants are eligible to this study (Table 1b and Figure 1).
| Characteristics | Frequency | % | Normal BW | LBW | % |
|---|---|---|---|---|---|
| Region | |||||
| Tigray | 294 | 13.96 | 272 | 22 | 7 |
| Afar | 9 | 0.44 | 7 | 2 | 22 |
| Amhara | 288 | 13.64 | 224 | 64 | 22 |
| Oromia | 602 | 28.53 | 523 | 79 | 13 |
| Somali | 73 | 3.44 | 65 | 8 | 11 |
| Benishangul | 36 | 1.71 | 33 | 4 | 11 |
| Southern Nation, Nationalities and People (SNNP) | 448 | 21.21 | 389 | 59 | 13 |
| Gambela | 12 | 0.57 | 11 | 1 | 8 |
| Harari | 13 | 0.63 | 12 | 1 | 8 |
| Addis Ababa | 306 | 14.49 | 271 | 35 | 11 |
| Dire Dawa | 29 | 1.36 | 26 | 3 | 10 |
| Residence | |||||
| Urban | 1026 | 48.63 | 914 | 112 | 11 |
| Rural | 1084 | 51.37 | 917 | 167 | 15 |
| Area poverty | |||||
| Low | 1424 | 67.47 | 1244 | 180 | 13 |
| High | 666 | 32.37 | 588 | 97 | 14 |
| Area education | |||||
| Low | 2001 | 94.83 | 1738 | 263 | 13 |
| High | 109 | 5.17 | 93 | 16 | 15 |
| Area media exposure | |||||
| Low | 1052 | 49.88 | 895 | 157 | 15 |
| High | 1058 | 50.12 | 937 | 121 | 11 |
Table 1b: Low birth weight distribution by Area level characteristics, EDHS 2016, Ethiopia, 2018.
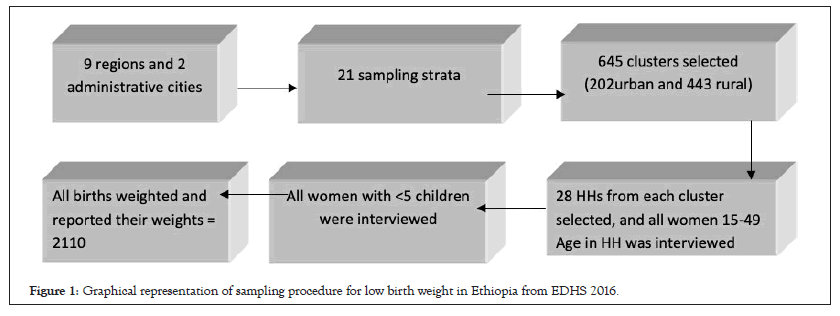
Figure 1: Graphical representation of sampling procedure for low birth weight in Ethiopia from EDHS 2016.
Data quality control
Data related to the outcome variable of low birth weight was selected and extracted from the child dataset of EDHS 2016. Further data cleaning, labeling, coding and recoding were done for all selected variables. Categorization was done for continuous and categorical variables using information from different literatures accordingly.
Study variables
Dependent variable: The outcome variable is low birth weight.
The dependent variable for the ith birth weight was represented by a random variable with two possible values coded 1 and 0. So, the response variable of the ith birth weight was measured as a dichotomous variable. (Yi=1 if low birth weight was occurred, otherwise Yi=0)
Independent variables: The explanatory variables were considered at two levels individual and area level factors.
• Individual level variable: Individual level factors considered in this study includes: Age of mother, maternal age at first birth, gestational age at birth, birth order, type of birth, sex of the child, sex of household head, marital status, mother’s educational level, husband/partner of mothers’ educational level, maternal occupation, husband/partner of mothers’ occupation, cigarette smoking, household wealth index, religion, household size, media exposure, body mass index.
• Area level variables: In addition to region, place of residence, Area media exposure, Area educational status, Area poverty status. The aggregated Area level predictor variables were constructed by aggregating individual level values at cluster level and binary categorization of the aggregated variables were done based on the distribution of the proportion values calculated for each cluster (Area).
Statistical methods of analysis
Multilevel modeling: Nature of nested data makes the uses of traditional regression methods inappropriate because of the assumption of independence among individual within the some group, assumption of equal variance across groups which an inherent in traditional regression methods are violated. Therefore, multilevel model is a type of regression analysis for multilevel data where the dependent variable is more appropriate for hierarchically structured data, such as the DHS to estimate the robust standard error. So in this study multilevel binary logistic regression analysis was employed in order to account for the hierarchical nature of the DHS data and the binary response of the outcome variable.
Descriptive analysis: Frequency and percentage were reported for categorical variables and continuous explanatory variables. In addition cross tabulation was showed the proportion of different categories of each characteristic with respect LBW.
Multilevel analysis: It includes:
• Bivariate multilevel logistic regression analysis: Bivariate MLRA was employed to explore association between dependent variable and a wide range of independent variables. Variables with p-value ≤ 0.25 entered multivariable logistic regression which controls the undesirable effects of confounding variables [18].
• Multivariable multilevel logistic regression analysis: Multilevel Logistic Regression Model was fitted to examine the individual and Area level factors that are associated with low birth weight at p-value of ≤ 0.25 during the Bivariate Multilevel Logistic Regression Analysis. Variables with p-value of less than 0.05 were considered as significant predictors. The result was presented with Adjusted Odds Ratio (AOR) and 95% Confidence Interval (CI).
Model specification
In this multilevel analysis it has set up of two level models. The level one individual variables and second level is the Area level. The analytical strategy in the case of multilevel analysis consists of four models.
First model: It is usually called the “empty” or “null model” is fitted without explanatory variables. In other words, it contained no covariates, but decomposes the total variance in to individual and Area components. The empty model is used to determine whether the overall difference between communities and individual on LBW were significant.
Y= ln [Pij/1-Pij]= boj + uoj (Equation-1)
In the above equation, Pij is probability of LBW, boj is the overall regression intercept when all predictors were adjusted to zero and uoj is the residuals at the Area level.
Second model: It is referred to as the “individual model” included individual-level characteristics. This is to allow the assessment of the association between the outcome variable and individual level characteristics. The model containing the individual level variables is used to determine whether the variation across communities could be explained by the characteristics of the individual residing within that Area or not.
Yij= βoj + β1 X1ij+...+βn Xnij+ uoj+eij (Equation-2)
In the above model, βoj is the intercept, β1 is the regression coefficient (regression slope) for the explanatory variable, X1ij is number of individual’s level factors and eij is the usual (random error term).
Third model: It contains only the Area level characteristics to allow the assessment of the impact of the Area level variables on the outcome variables.
Yij= βoj +β1Z1 + …+βnjZnj+eij + unj (Equation-3)
Each cluster has different intercept βoj, slope coefficients β1, Znj is number of Area level factors and unj random residual error terms at the cluster level.
Fourth model: It is generated which is called “final model”. This includes explanatory variables at both the individual and Area level simultaneously. The final model is used to test for the independent effect of Area contextual variables above and over the individual variables. The simultaneous inclusion of both individual and Area level predictors in the multilevel logistic regression model permits: (1) the examination of Area effects after individual level confounders have been controlled for: (2) the examination of individual level characteristics as modifiers of the Area effect (and vice versa); and (3) the simultaneous examination of within and between Area variability in outcomes, and of the extent to which between Area variation is explained by individual and Area level characteristics (Table 2).
| Characteristics | Empty individual area | (Individual and Area) Model 4 AOR (95% CI) | ||
|---|---|---|---|---|
| Model 1 | Model 2 AOR (95% CI) | Model 3 AOR (95% CI) | ||
| Child is single or twin | ||||
| Single birth | Ref | Ref | ||
| Multiple birth | 3.25(1.670-6.355) | 2.74*(1.450-5.184) | ||
| Birth order | ||||
| 1-3 | Ref | Ref | ||
| 4-5 | 0.80(0.501-1.296) | 0.87(0.570-1.326) | ||
| 6 and above | 0.40(0.205-0.801) | 0.42*(0.242-0.752) | ||
| Gestational age | ||||
| Term | Ref | Ref | ||
| Preterm | 6.69(3.361-13.35) | 4.83*(2.644-8.830) | ||
| Anemia level | ||||
| Not anemic | Ref | Ref | ||
| Anemic | 1.37(0.974-1.954) | 1.49*(1.069-2.092) | ||
| Mothers educational level | ||||
| No education | Ref | Ref | ||
| Primary | 0.61(0.396-0.941) | 0.61*(0.418-0.896) | ||
| Secondary/higher | 0.43(0.252-0.752) | 0.39*(0.252-0.612) | ||
| Region | ||||
| Tigray | Ref | Ref | ||
| Afar | 3.98*(1.509-10.499) | 3.83*(1.463-10.044) | ||
| Amhara | 3.74*(1.762-7.950) | 3.50*(1.649-7.428) | ||
| Oromiya | 2.23*(1.113-4.483) | 2.19*(1.085-4.411) | ||
| Somali | 1.93(0.957-3.891) | 1.32(0.625-2.818) | ||
| Benishangul | 1.13(0.54-6-2.371) | 1.35(0.630-2.906) | ||
| SNNPR | 1.92(0.999-3.707) | 2.39*(1.236-4.644) | ||
| Gambela | 1.79(0.890-3.602) | 1.71(0.846-3.471) | ||
| Harari | 0.74(0.340-1.629) | 0.73(0.330-1.623) | ||
| Addis Ababa | 1.96*(1.030-3.760) | 1.73(0.935-3.203) | ||
| Dire Dawa | 1.32(0.667-2.637) | 1.23(0.627-2.437) | ||
| Random effect parameters | Empty | Individual | Area | Individual and Area |
| Area level variance and (SE) | 0.434 (0.1869) | 0.3 (0.1801) | 0.247 (0.1572) | 0.155 (0.1576) |
| ICC (%) | 11.7 | 8.4 | 7 | 4.5 |
| PCV (%) | Ref | 33.6 | 44 | 64.3 |
| Model fit statistics AIC | 1469.67 | 1340.07 | 1463.08 | 1333.33 |
Note: * represents the area level of variables
Table 2: multivariable multilevel logistic regression analysis of individual and Area level factors associated of low birth weight 2016.
The formula for the final models expressed as:
Log [Pij / (1-Pij)] = boj +b1X1ij + b1Z1j+…..+ uoj+ eij
• Pij is the probability of LBW ith birth weight in the jth Area
• boj is the log odd of the intercept
• b1,b...bnj are the regression coefficient estimate the data
• X1ij,…Xnij are the covariates (independent variables) which may be defined at the individual level
• Z1j,…Znj are the covariates (Area variables) which may be defined at the Area level
• uoj are random error at the Area level
• eij are random error at the individual level
Parameter estimation method
The parameters that have to be estimated are the fixed coefficients b0, b1, etc and the random parameters s2 u0.
In the multilevel model, fixed effects (measure of association) refer to the individual and Area covariates and expressed as Adjusted Odds Ratio (AOR) and 95% confidence interval. The random effects are the measure of variation with LBW across communities. The ratio of the variance at the Area level to the total variance is referred to as the Intra-class Correlation Coefficient (ICC). The precision is measured by the Standard Error (SE) of the independent variables [19].The result of random effects (which are the measure of variation) are expressed as Variance Partition Coefficient (VPC) (which in this study is equal to ICC), and Proportional Change in Variance (PCV). As a result of the dichotomous nature of the outcome variable in the study, the VPC calculated based on the linear threshold model method which converts the individual level variance from the probability scale to the logistic scale, on which the Area level variance is expressed [20]. In the other words, by using the linear threshold model, the unobserved individual outcome variable follows a logistic distribution with individual level variance S2 e equal to p2/3=3.29. In this case, the VPC corresponds to the ICC, which is a measure of general clustering of individual outcome of interest in the communities.
The ICC is calculated as: ICC = (s²u/(s²u+ p²/3)
ICC is the proportion of Area variance out of the total variance (Area plus individual variance) s²u is the variance of the Area level, p²/3=3.29 and represent the fixed individual variance.
Area differences with LBW may be attributable to contextual influences or differences in individual composition of communities (including unobserved individual characteristics). In view of this, while adjusting for the individual characteristics in the multilevel model, same part of the compositional differences were taken in to consideration to explain some of the Area difference observed in the empty model. Thus the equation for the proportional change in Area variance is:
PCV1=(VN1-VN2)/VN1
VN1 –is the Area variance in the empty model and VN2 is the Area variance in the model including either individual level characteristics or Area level characteristics or both individual and Area level characteristics [20].
The Wald test was used to test the null hypothesis that a parameter value is zero or that a group of parameters are jointly zero. The latter case applies when testing the significance of categorical variable. Linear functions of parameters can also be tested. If the null hypothesis is true, the test statistic is distributed as approximately x² with r degrees of freedom, where r is the number of functions that are being tested [21]. Hence, the significance of freedom variation at each level will be tested with the Wald test, and p- values <0.05 were considered to be significant to reject the null hypothesis.
Model diagnostics
Multi-collinearity diagnostic evaluation was done using Variance Inflation Factor (VIF), and thus value of VIF greater than 10, gives evidence of multi-collinearity. Interaction effects were assessed between individual and Area level explanatory variables [22].
Model fit statistic
Receiver Operating Characteristics (ROC) curve was used to assess general accuracy of the model to the data set using the area under receiver operating characteristics. ROC curve is a commonly used measure for summarizing the discriminatory ability of a binary prediction model.
Relative goodness-of-fit tests were conducted using both Akaike’s Information Criteria (AIC) for each of the models and compared. In general, it might be best to use AIC together in model selection. This was done because AIC was the appropriate selection in multilevel analysis than other methods. Since multilevel data have a different sample size at different levels and compared to AIC [23].
This study used multilevel logistic regression analysis to address these two level factors. Accordingly the individual and Area level factors such as the type of birth, gestational age at birth, anemia status, birth order, mother’s educational level and region have a significant association with low birth weight. Child whose mother’s with multiple births had high odds of LBW compared to those with single birth. Study done in Nigeria also shows multiple birth children were found to be significantly positively associated with LBW [24]. Similarly, a multilevel analysis conducted in Ethiopia also showed that multiple-birth children are 1.964 times more likely to have a LBW than single births [25]. Twin gestations are commonly associated with delivery of LBW infants because sometimes leading to complications like anemia, high blood pressure and early labor [26].
Gestational age at birth was also found to be an important factor in determining low birth weight in this study. Preterm gestational ages at birth had higher odds of low birth weight compared with full term birth. Studies conducted in Tanzania, Ghana and Uganda also shows gestational age less than 37 weeks were found to be significantly positively associated with LBW [27-29]. This is also consistent with study conducted in Gondar, Ethiopia [30].
This study found that anemic mothers were positively associated with low birth weight. Similar studies conducted in northern Tanzania and Ethiopia also shows mothers who are anemic are significantly vulnerable to small birth size than those who had not anemic mothers [25,31]. Some studies have demonstrated a strong association between low hemoglobin before delivery and LBW babies. Maternal anemia is commonly considered a risk factor for LBW babies [32].
Even though having a birth order of 6 and above showed odds of low birth weight compared to lower birth order (one up to three), other study conducted in Malawi revealed that birth order of 2–3 and 4–5 are associated with lower risk of being small at birth compared to those with first birth order [33]. But another studies conducted in 2014 in Ethiopia birth order of the child appeared to have no significant effect on determining the baby’s size at birth [25]. During pregnancy, structural changes take place in the uterine spiral arteries, increasing blood flow with beneficial effects for fetal growth [34].
Maternal educational level appeared to be a very important determinant of the LBW in this study. The risk of LBW is significantly higher for children whose mothers have no education than children whose mothers have primary or secondary/higher level of education. Other studies done in Northern Tanzania, Nigeria, Kenya and Malawi implied that mothers’ education has an association with delivery of LBW. Children of higher education mothers have reduced chance of being small at birth than children of mothers with no education [24,27,33,35]. Previous single level studies done in Ethiopia showed a consistent result with this study [25,36]. Low educated mothers are more frequently malnourished, have unhealthy habits, chronic diseases and inadequate prenatal care and this in turn related with mothers delivering small birth size infants [25].
Concerning the regional disparity children born in Afar, Amhara, Oromiya and Southern nations, nationalities and people were at a higher odds of LBW than children who born in Tigray. Similarly, previous study conducted In Ethiopia showed that children whose mothers reside in Afar, Amhara and Addis Ababa were more likely to be LBW as compared to those from the reference category (Dire Dawa) [25]. The observed high odds of LBW in these regions may be attributed to differences in nutrition, socio economic status, health care services, and other cultural and life style differences among these regions.
In this study the overall percentage of low birth weight in Ethiopia remained higher. The results of this study showed that multiple births, anemic mothers, birth order, not-educated mothers and preterm gestational age at birth were significant factors of low birth weight. Also, there exist considerable differences in baby’s size at birth among regions. Hence, switching off/on the significant factors accordingly could reduce the risk of having low birth weight child.
There were no cluster level weights for conducting weighted analysis and some variables may not be collected at the date of the event.
[Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
Citation: Weldemariam KT, Gezae KE, Abebe HT, Teklu T (2023) Individual and Area Level Factors of Low Birth Weight in Ethiopia: Evidence from Ethiopian Demographic Health Survey 2016: Multilevel Modeling. Adv Pediatr Res. 10:056.
Received: 10-May-2023, Manuscript No. LDAPR-23-24015; Editor assigned: 12-May-2023, Pre QC No. LDAPR-23-24015 (PQ); Reviewed: 26-May-2023, QC No. LDAPR-23-24015; Revised: 05-Jun-2023, Manuscript No. LDAPR-23-24015 (R); Published: 12-Jun-2023 , DOI: 10.35248/2385-4529.23.10.056
Copyright: © 2023 Weldemariam KT, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.