
Advances in Pediatric Research
Open Access
ISSN: 2385-4529

ISSN: 2385-4529
Research Article - (2022)Volume 9, Issue 6
Introduction: Neonatal mortality is the death of newborn babies from the time of birth to 28 completed days of life which is the most vulnerable time for a child's survival. About one million of them passed away on their first day of life, and more than two thirds (38%) of the deaths were in sub-Saharan Africa where Ethiopia is one of the countries with the highest neonatal mortality in the world which accounts for 29 deaths per 1,000 live births.
Methods: Institutional based retrospective cross-sectional study design was conducted from November 1, 2018, up to January 30, 2019, in Debre Tabor General Hospital (DTGH). A Structured interviewer-administered pre-tested questionnaire was used to collect data. The collected data were entered into Epi data version 4.2 and then exported into SPSS window version 24. Bivariate and multivariate analysis was undertaken and information was presented by using simple frequency tables, graphs, and pie charts.
Result: The prevalence of neonatal mortality was found to be 12.3%. Gestational age group 28-32 weeks (AOR [Adjusted Odd Ratio] =9.5, 95% CI: 2.39-37.97), Gestational Age beyond 42 weeks (AOR=4.6, 95% CI: 6.3-33.8), and forceps delivery (AOR=0.18, 95% CI: 0.05-0.68) were found to be statistically significant.
Conclusion: Neonatal mortality was higher than the national with independently associated factors of prematurity and post maturity while forceps delivery as a preventive factor. Therefore, this might be essential to the hospital neonatal intensive care unit nurse to plan for managing prematurity and post maturity in better nursing care as well as providing quality ANC (Ante-Natal Care) and identifying most predisposing factors for prematurity.
Neonatal mortality; NICU (Neonatal intensive care unit); Preventive factor; Infants
Neonatal morbidity and mortality are the major global public health challenges, specifically for the first 28 days of life. Globally, each year over 4 million neonates died within 28 days of birth among 130 million births. Every minute, twenty under-five children die, leading to 8 million deaths before they reach their fifth birthday due to the conditions which could be either avoided or treated. Neonatal mortality accounts for two- thirds of deaths of infants, and nearly two-fifths of all deaths in under-five children. Many babies die nameless and unrecorded, indicating the perceived inevitability of their deaths. Most neonatal deaths (99%) occur in low and middle-income countries, where about half of the deaths occur at home. Ethiopia, one of the countries with the highest neonatal mortality in the world, is responsible for 29 deaths per 1,000 live births which was over 9 times more than that of highly developed countries, where the rate is 29 per 1,000 live births [1,2]. The health of future societies depends on the health of the children of today and their mothers. The neonatal period is considered as the highest risk period. Childhood mortality is often used as a broad indicator of social development or a specific indicator of the health conditions of a country. However, child health programs were given low attention, especially neonatal health [3-5]. Every year an estimated 4 million babies die in the first 4 weeks of life (the neonatal period). Three-quarters of neonatal death happens in the first week, the highest risk of death is on the first day of life. The highest number of neonatal death was in South Asian countries and the highest rate is generally in sub-Saharan Africa. Preventing death in newborn babies has not been a focus of child survival or safe motherhood programs. While we neglect these challenges, 450 newborn die every hour, mainly from the preventable cause which is unjustifiable in the 21 century [2]. Neonatal mortality accounts for 44% of underfive mortality in 2014. Average death during the neonatal period is 30 times higher compared to the rest of under-five children. Ten countries account for 67% of neonatal mortality globally by which Ethiopia accounts for 4% of global neonatal mortality [6]. Neonatal mortality has three main causes in low and middleincome countries. The complication of preterm, asphyxia, and neonatal infection together contribute to 85% of newborn death. In 2013, 35% of the global neonatal deaths were caused by complications of preterm birth, 24% by intrapartum related complications, and 25% by infection. The rest of the death is caused by congenital malformations [7,8]. In Ethiopia, the rate of under-five mortality (U5MR) decreased by 60% from the year 2000 to 2016 which implies from 123 to 67 per 1000 of live births. However, the neonatal mortality rate (NMR) decreased only by 40% from 49/1000 live births to 29 per 1000 live births from 2000 to 2016. Because of this, the share of neonatal mortality in under-five mortality has been increased from 29.5% to 43% [3]. Neonatal health problems are usually seen as similar to an older child's health problem. But, the causes of neonatal mortality and intervention to improve neonatal health are different from that of other under-five children. Neonatal survival is the most important indicator of improved health care during childbirth. There is a gap in integrating the need for care of neonates in the NICU, the neonatal health problems, and health programs for maternal and child health. As a result, there is still slow progress to decrease neonatal mortality in the majority part of the country by which they contribute to the national burden of neonatal mortality in Ethiopia. Even though there were some endeavors in identifying major causes of neonatal death, in Ethiopia, studies that identify the prevalence and associated factors of neonatal mortality were not applicable as they were not specific for the nurses-led hospital admitted neonates in a single hospital in intensive care unit. This study demonstrates the impact of nurse-led nursing care in neonatal intensive care unit Which provides with what neonatal health problem majorly challenge the nursing care, and come up with a base line evidence for future applied research and intervention in the hospital. Having data on the prevalence of the problem, it is crucial to take prioritized actions in the unit leaded by neonatal nurses [9,10].
Study design and period
An Institutional based cross-sectional study was conducted from November 1, 2018, to January 30, 2019, in Debre Tabor General Hospital in NICU among admitted neonates.
Study setting
Debre Tabor General Hospital is found in the South Gondar zone in the Amhara region of Ethiopia. It was officially commenced its function in 1917 and currently, it delivers the health care services for more than 2.3 million populations through medical, surgical, gynecological, pediatrics, NICU, ophthalmological wards, and 14 OPD with a total of 182 beds and 444 staffs.
Annually, nearly more than 1250 neonates were admitted to the neonatal intensive care unit with different health problems. It has 22 beds, 3 pediatricians, and 20 nurses in which 2 are neonatal nurses.
Study population
All neonates who were admitted at NICU in Debre Tabor General Hospital from November 1, 2018, up to January 30, 2019.
Sample size estimation
The sample size was calculated using single population proportion formula and by taking into the following consideration: prevalence (P) of neonatal mortality 13.29% Confidence Level (CL) 95%, the margin of error (d) 5%, and by adding 10% for non-response rate. The final sample size came up to 195. However, to make a statistical analysis of logistic binary logistic regression, a 50% proportion (p) was used to get the final sample size to be 422.
Data collection and procedure
Before data collection, both the data collectors and supervisors have trained by the principal investigator for one day. Secondary data was collected from Neonatal ICU treatment registers by using a structured questionnaire and checklist designed in the way that it could collect pieces of information about all the relevant variables. Then it was pre-tested with individuals’ equivalent to 5% of the calculated sample size among Debre tabor General hospital. Data were collected by two BSc nurses and one MSc nurse for the supervisor. The data has collected among admitted neonates on a specified period from NICU. A simple random sampling method was used to select neonates admitted in NICU from medical records. This was done by sampling frame 1up to N [1; 1000] admitted neonates in NICU, then choose 422 samples were chosen every 2 intervals of medical record systematically, so it was taken the sample from a patient chart and register which have full information.
Data quality control
Data quality was assured by proper designing of the questionnaire in Amharic the local language to prevent misinterpretation, apply pre-test on 5% of the sample in Debre Tabor General Hospital. The data have also coded, entered, cleaned, and made close supervision during data collection by the principal investigator.
Data analysis
Then data have coded, entered, and cleaned using Epi-data version 4.2 software and finally exported into SPSS version 24 for analysis. Bivariate analysis, crude odds ratio with 95% CI, was used to see the association between each Independent variable and the outcome variable by using binary logistic regression. Independent Variables with a p-value of ≤ 0.05 were included in the multivariable analysis to control Confounding factors. Adjusted odds ratios with 95% CI were estimated to identify the prevalence and associated factors of neonatal mortality using multivariable logistic regression analysis. The level of statistical significance was declared at p-value ≤ 0.05.
Sociodemographic characteristics
From the total of 928 selected neonatal charts during study periods, 422 neonatal charts were reviewed. The majority of maternal age group were 20-34 and the least were age group 20 and below which accounts 284 (67.3%) and 16 (3.7%) respectively. The majority 392 (92.90%) were born from married parents while 219 (51.8%) were from rural family while 203 (48.2%) from urban; and 172 (40.5%) born from mothers with no formal education and 41 (9.7%) were from mothers with completed primary educational level. Majority of neonates were from housewife mothers and the least were from others occupation which accounts 223 (52.8%) and 80 (19 %) respectively (Table 1).
| Characteristics | Frequency | Percentage (%) | |
|---|---|---|---|
| Age of mothers | <20 years | 16 | 3.7 |
| 20-34 years | 284 | 67.3 | |
| >=35 years | 122 | 28.9 | |
| Marital status | Married | 392 | 92.90% |
| Not married | 28 | 6.63% | |
| Others | 2 | 0.47 | |
| Residence | Rural | 219 | 51.8% |
| Urban | 203 | 48.2% | |
| Educational status | No formal education | 172 | 40.5% |
| Can read and write | 91 | 21.6% | |
| Primary school | 41 | 9.7% | |
| Secondary school | 56 | 13.3% | |
| College and above | 63 | 14.9% | |
| Occupation | House wife | 223 | 52.8% |
| Employers | 119 | 28.2% | |
| Others | 80 | 19.0% | |
Table 1: Maternal sociodemographic characteristics of prevalence and associated factors of neonatal mortality among admitted neonates in NICU, Debre Tabor Hospital, 2019.
Prevalence of neonatal mortality
The prevalence of neonatal mortality was found to be 12.30%.
Neonatal characteristics
Out of 422 neonates, female, male and ambiguous genitalia were 214 (50.7 %), 207 (49%) and 1(0.3%) respectively. The majority of neonates were admitted at age less than or equal to 7 days 409 (96.92%) and the least 13 (3.08%) were 8 days or beyond.
Most neonates were died at early neonatal age and late neonatal age which accounts 45 (87%) and 7(13) respectively. Sepsis 203 (48.2%), asphyxia 95 (22.56%) and others 71 (16.92%) were the leading cause of neonatal admission from first to third respectively whereas the majority 209 (53.85%) were low birth weight and the least were very low birth weight which accounts 10 (2.56 %). The majority neonates were born from mothers whose membrane rupture from 1 to 12 hours 395 (93.58%) and those with 12 to 24 hours duration were 26 (6.15%).
Pregnancy and obstetric characteristics
The majority maternal factors were duration of labor lasts from one to twelve hours 218 (56.41%), and the least were above twenty four hours 19 (5.13%). Regarding labor delivery, the majority was through SVD (Spontaneous Vaginal Delivery) and least were forceps which accounts 296 (70.26%) and 33 (7.69%) respectively.
The majority were delivered at health institution 389 (92.28 %) and the majority of presentation were cephalic which accounts 315 (81.03%). Majority neonates were term (37-42 weeks) 232 (54.80%) and the least were both post term (≥42 weeks) and unknown gestational age which accounts 13 (3.10%). The majority 385 (91.28%) had ANC follow up visit whereas 37(8.72%) did not have ANC follow up in which majority 192 (45.64%) had four ANC visit (Table 2).
| Variables | Frequency (n=422) | Percent (%) |
|---|---|---|
| Cause of admission | ||
| Asphyxia | 95 | 22.56 |
| Sepsis | 203 | 48.2 |
| Jaundice | 20 | 4.62 |
| Pneumonia | 20 | 4.62 |
| Birth trauma | 13 | 3.08 |
| Others | 71 | 16.92 |
| Duration of labor(DOL) | N=385 | Percent |
| 1-12 hours | 218 | 56.41 |
| 12-24 hours | 148 | 38.46 |
| Above 24 hours | 19 | 5.13 |
| Mode of delivery | N=422 | Percent (%) |
| SVD | 296 | 70.26 |
| Forceps | 33 | 7.69 |
| Vacuum | 39 | 9.23 |
| C/S | 54 | 12.82 |
| Presentation at labor | N=389 | Percent (%) |
| Cephalic | 315 | 81.03 |
| Breach | 66 | 16.92 |
| Others | 8 | 2.06 |
| Gestational age at birth | N=389 | Percent (%) |
| 28-32 weeks | 45 | 10.8 |
| 32-36 weeks | 119 | 28.2 |
| 37-42 weeks | 232 | 54.8 |
| Above 42 weeks | 13 | 3.1 |
| Unknown | 13 | 3.1 |
| Birth weight | N=386 | Percent (%) |
| VLBW | 10 | 2.56 |
| LBW | 209 | 53.85 |
| NBW | 167 | 43.59 |
| ANC visit during pregnancy | N= 422 | Percent (%) |
| Yes | 385 | 91.28 |
| No | 37 | 8.72 |
| Duration of rupture of membrane (ROM) | N=389 | Percent (%) |
| ≤ 12 hours | 365 | 93.84 |
| >12 hours | 24 | 6.16 |
Table 2: Maternal and neonatal characteristics for prevalence and associated factors of neonatal mortality among admitted neonates in NICU, Debre Tabor General Hospital, 2019.
Maternal health problems during pregnancy
The majority, 303 (71.9%) women did not have health problem during pregnancy while the rest 119 (28.2%) had different health problem at the latest pregnancy.
Types of health problem during pregnancy
Among 119 women who had health problem, 86 (72.27%) were with hypertensive disorders during pregnancy and those with others disorders were 2 (1.68%) (Figure 1).
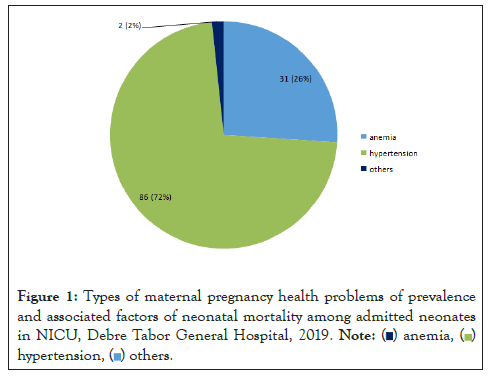
Figure 1: Types of maternal pregnancy health problems of prevalence
and associated factors of neonatal mortality among admitted neonates
in NICU, Debre Tabor General Hospital, 2019.
Factors associated with neonatal mortality
Binary and multiple logistic regressions have been used to identify associated factors. There were no marked variation by mode of delivery, presentation of labor, maternal health problems during pregnancy and maternal educational level even though it appeared associated factors of neonatal mortality by bivariate analysis.
Neonatal gestational age group (28-32 weeks) and beyond 42 weeks were risk factors for neonatal mortality while forceps delivery was protective factor for neonatal mortality.
Neonates with (28-32 weeks) age group were 9.5 times more likely to death than (37-42 weeks) age group. And those with gestational age group >42 weeks were 4.6 times more likely to death than gestational age group (37-42 weeks). Those neonates who delivered by forceps were 18% less likely to die than SVD (Table 3).
| Variables | Outcome of admission | 95% confidence interval | ||
|---|---|---|---|---|
| Mode of delivery | Discharged | Died | COR | AOR |
| SVD | 388 (92%) | 34 (8%) | 1 | 1 |
| Forceps | 366 (86.7%) | 56 (13.3%) | 1.76 (0.35-8.82) | 0.18(0.05-0.68)* |
| Vacuum | 304 (72.2%) | 118 (27.8%) | 4.40(1.32-14.64) | 0.44(0.07-2.82) |
| C/S | 321 (76%) | 101 (24%) | 3.61(1.19-10.92) | 1.49 (0.41-7.86) |
| Presentation at labora | ||||
| Cephalic | 352(90.5%) | 37(9.5%) | 1 | 1 |
| Breach | 295(75.8%) | 94(24.2%) | 3.05(1.17-7.94) | 0.15(0.0-4.61) |
| Gestational age at birth | ||||
| 28-32 wks | 276(71.4%) | 96(24.8%) | 3.88(1.23-12.24) | 9.5(2.39-37.97)* |
| 32-36 wks | 350(90.2%) | 38(9.8%) | 1.05(0.36-3.06) | 2.0(0.60-6.7) |
| Above 42 wks | 259(66.7%) | 128(33.3%) | 4.85(0.78-29.87) | 4.6(6.3-33.8) |
| 37-42 wks | 353(90.7%) | 35(9.3%) | 1 | 1 |
| Problem during pregnancya | ||||
| Yes | 338(80.8%) | 84(20%) | 2.44(1.02-5.84) | 2.41(0.72-7.92) |
| No | 380(90.7%) | 38(9.3%) | 1 | 1 |
| Educational status of mothersa | ||||
| No formal education | 375(88.9%) | 42(10.1%) | 0.43(1.3-1.37) | 0.17(0.07-1.55) |
| Can read and write | 338(81%) | 80(19%) | 0.90(0.27-2.94) | 0.99(0.19-5.0) |
| Primary school | 397(94.7%) | 21(5.3%) | 0.21(0.23-1.93) | 0.58(0.03-8.62) |
| Secondary school | 405(96.2%) | 16(3.8%) | 0.15(0.01-1.37) | 0.16(0.01-2.27) |
| Above secondary | 333(79.3%) | 87(20.7%) | 1 | 1 |
Note: avariables significant at p <0.2 in bi variable analysis, *significant withp ≤ 0.001, 1= reference.
Table 3: The factors for prevalence and associated factors among admitted neonates in NICU, Debre Tabor General Hospital (n=422), 2019.
In this study, the prevalence of neonatal mortality was 12.3%. The prevalence was higher than the national neonatal mortality with is 29 per 1000 live births [1]. The study conducted at Jimma specialized hospital and Felege Hiwot Referral Hospital Ethiopia showed that neonatal mortality was 35.4% which was nearly three times higher than prevalence in Debre Tabor Hospital and 13.29% which was comparable to this study respectively. And this study finding was higher than study conducted in Dire Dawa Ethiopia which was 11.44%. The study conducted in Pakistan showed that the neonatal mortality were 27% which was higher than this study [11-17].
This variation might be due to different socioeconomic status of the mother and level of differences among hospitals in which the studies conducted.
The previous studies showed that mode of delivery, educational status of secondary school, marital status, house hold wealth, male sex and ANC visit, preterm gestational age and early neonatal age were associated factors for neonatal mortality [17,18]. Similarly, in this study, forceps delivery and gestational age group (28-32 weeks) had significant association for neonatal mortality. In addition, gestational age group beyond 42 weeks was associated factors.
The neonate who were delivered through forceps were 18% less likely to die than those who delivered by spontaneous vaginal delivery. But, the study in Sudan showed that neonates delivered in C/S (Cesarean Section) were more likely to die than spontaneous vaginal delivery [11]. This might be due to timely management of labor which in turn decreases labor complications. Gestational age at delivery was significantly associated with neonatal mortality. The newborns who were preterm (28-32) weeks were 9.5 times more likely to die than who were delivered at term (37-42) weeks which was 4 times higher than the study conducted at Bahir Dar Felege Hiwot Referral Hospital [17]. This might be due to different in hospital care level like ANC, institutional delivery and quality of maternal health service [19].
The prevalence of neonatal mortality was higher compared to the national figure while Factors associated with neonatal mortality were prematurity (28-32 weeks) of gestational age, post term (>42 weeks) of gestational age and forceps delivery which is preventive. Therefore, this might be essential to the hospital neonatal intensive care unit nurses to plan for managing prematurity and post maturity in better nursing care as well as providing quality ANC (Ante-Natal Care) and identifying most predisposing factors for prematurity. And, the way forwarded to the hospital management team, using this study as an input would be providing client based individualized ANC care to decrease prematurity, enhanced pre term care at NICU and studies on causes of prematurity as it was the leading factor for neonatal mortality in this study.
The neonatal chart was secondary data, hence some missing information on individual folders.
The authors acknowledge the Debre Tabor University, College of health sciences, Department of neonatal nursing and pediatrics child health nursing, the data collectors, the supervisors for their inevitable support and encouragement in carrying out his research.
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of this article.
SD: the corresponding authors, has prepared the proposal, and writing up the manuscript, BM: has prepared data collection tools, analyzed the data. TM: has interpreted the result and monitored data collection procedures. KA: edited the final manuscript.
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
Citation: Demis S, Munye T, Munye B, Agmas K (2022 Prevalence of Neonatal Mortality and its Associated Factors among Neonates Admitted in Neonatal Intensive Care Unit in Debre Tabor General Hospital, Northcentral, Ethiopia. Adv Pediatr Res. 9:047.
Received: 23-Nov-2022, Manuscript No. LDAPR-22-20395; Editor assigned: 25-Nov-2022, Pre QC No. LDAPR-22-20395 (PQ); Reviewed: 12-Dec-2022, QC No. LDAPR-22-20395; Revised: 20-Dec-2022, Manuscript No. LDAPR-22-20395 (R); Published: 28-Dec-2022 , DOI: 10.35248/2385- 4529.22.9.047
Copyright: © 2022 Demis S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.