
Advances in Pediatric Research
Open Access
ISSN: 2385-4529

ISSN: 2385-4529
Research Article - (2021)Volume 8, Issue 1
Introduction: Despite World health organization universal recommendation of Preventive Therapy, only 56% of pediatrics on ART receiving this intervention. The aim of this study was to determine the magnitude of Preventive Therapy and challenges in its effective implementation among HIV exposed children in Ilu Ababor zone public hospitals.
Materials: A facility based retrospective cohort study was used among 300 children’s’ reviewing records by standard structured questionnaires and interviewing their primary caregivers. Data were cleared and entered into Epi-info version 3.1 and exported into SPSS version 24 for further analysis and a binary logistic regression was used to investigate factors associated with uptake of Preventive Therapy. Variables with p-value <0.2 in bivariable analysis were entered into the multivariable analysis. Odds ratio with 95% confidence interval was estimated to show the strength of association and the p-value <0.05 was used to declare as statistical significance in the multivariable analysis.
Results: Out of 300 (293) records were reviewed with a response rate of 97.6%. Almost all of the respondents were female 279 (93%) also about half (48%) of the respondents were orthodox in religion and a few (3.4%) of them have had primary education. More than half the exposed infants’ age was b/n 13-18 months. Moreover, about 65.5% of guardians were well awared about preventive treatment.
The strongest independent predictors of poor adherence to Preventive Therapy are not able to read [OR=0.153 (0.027-0.863) P< 0.330], long procedure in getting the drug (OR=9.913[2.825, 34.731], p=<0.000), Shortage of drug availability [OR=9.91 (2.829-34.73), P< 0.000], missed dose greater than three doses [OR=2.69 (1.17-6.26), p=<0.022], Persistent diarrhoea [OR=4.324 (1.067-17.530), p=0.040] were associated with Preventive Therapy among HIV exposed children.
Conclusion: Preventive Therapy in study area was found to be relatively high and long procedure, shortage of preventive drug and persistent diarrhea were found to be significant predictors of Preventive Therapy, Hence, to avert this, accessing drugs, treating persistent diarrhea and decreasing waiting time were plays unfold role to increases uptake of Preventive Therapy.
Preventive Therapy adherence; Uptake; HIV Exposed Child
According to UNICEF estimate and projection in 2016 nearly 740, 251 populations were positive for HIV among these 143,201were children and there were 4,800 new HIV infections among children less than 15 years [1]. Moreover, in 2015, around 1.1 million people died from HIV-related causes diseases and there were 2.6 million children living with HIV around the world, 90% of who live in sub- Saharan Africa [2,3]. In addition, Daily 1000 newly HIV infected children of majority in sub-Saharan Africa [4]. Beside this without access to cotrimoxazole and isoniazid prophylaxis, Antiretroviral Therapy (ART) and supportive care, about a third of all HIVinfected infants die by 1 year of age and about half of all HIVinfected infants die by age 2 years [5]. To prevent opportunistic infections during the early years of life, especially when the serostatus of the child is not yet confirmed, the use of antibiotic prophylaxis is commended especially the use of cotrimoxazole prophylaxis for exposed children and adolescent living with HIV to prevent OI, complications and avoid simultaneous intermittent preventive treatment is maintained, and it also equally benefits with respect to mortality, low birth weight and placental malaria. In Africa, Cotrimoxazole and isoniazid prophylaxis reduces mortality by 25% - 46% among children living with HIV/AIDS [6]. Despite of this importance, it also has its limitations in resource-limited settings, with potential for increased bacterial resistance due to inappropriate use of the cotrimoxazole [7]. In Ethiopia, out of an estimated 135,000 children who are in need of Preventive Therapy; Only56 % are currently receiving this intervention.
Studies pointed out that there are challenges related to Uptake of Preventive Therapy like educational level of mothers, low economic status of caregiver, adherence to ART supply chain& management like issues of stock-out imposing charge for the medication, low coverage of CTX and counselling, lost to follow up, missing dose inadequate training for health care workers and distance from the health facility [8].
In Ethiopia, up to 52% and 75% of HIV exposed children die before the age of two and five years respectively in the absence of any intervention. This is due to gap on the current Preventive Therapy up take implementation and the current guidelines for Preventive Therapy use among exposed children. Therefore, the aim of this study was to determine up take and challenges facing in effective implementation of Preventive Therapy in children born from HIV infected mother in governmental hospitals in Ilubabor zone of Oromia regional state, Ethiopia.
Study area
The study was conducted among governmental hospitals in Ilubabor zone. One of Oromia regional state zone which is located 600 km away from the capital city, Addis Ababa, Ethiopia. It is bordered on the south by south nation nationality and peoples, southwest Gambella Regional state, on the west by Kellem Wollega zone, on the north by west wollega zone, on the northwest by Buno Bedele Zone. There are two public hospitals (Mettu karl referral hospital and Darimu hospital) which are delivering PMTCT service.
Study design
The facility based a retrospective cohort study that involve review of the records of children from PMTCT register books of at for past 2 years, and Interviewing health care workers and their parents/ guardian of all children at follow up clinic in two public hospital of Ilubabor zone from March1-30,2018G.C.
Source and study population
All children born from HIV infected mother and enrolled at PMTCT follow up clinic and All HIV exposed children from six week to five years of age those enrolled at PMTCT follow up clinic in zone governmental public hospital over the last two years were used as source and study population respectively.
Sample size determination and sampling procedure
The sample size was determined by using formula to estimate the single population proportion as follows from retrospective study done in Addis Ababa 56% of infants adhered to cotrimoxazole with 95% CI and 5% marginal error (7).
The after proportionally allocation of sample size to the public hospitals, simple random sampling technique was used to select each sampling unit(ART registration book) for each hospitals.
Data collection tool
Data were collected by using structured questionnaire to gather information of infants from the PMTCT register books. The data were collected through the review of the PMTCT register books and interview of parents, guardians /care giver, and health care workers.
Data Collection Procedure and Quality Control methods
Structured questionnaire was prepared in English after reviewing literatures of similar study. The final modified English questionnaire was translated to Afan oromo which is dominant local language. One supervisor and three data collectors were female diploma and BSc holders in health respectively who have experience on it. The supervisors were trained for two days on components of data collection which are data collection procedure, accuracy and completeness of the data. After the training, pretest was carried out on the 5% of the sample was done in similar population that was in other health facility, to ensure the quality and validity of the data.
Operational definition and study variables
Uptake of Preventive Therapy is providing /supplying cotrimoxazole and Isoniazid prophylaxis in line to the national guideline or infant having Preventive Therapy start at six week of age. If responded ‘Yes’ coded as ‘1’ whereas ‘No’ coded as ‘0’ as the child didn’t on Preventive Therapy.
Challenge in implementation of Preventive Therapy: The factors that hinder implementation of Preventive Therapy.
Preventive treatment Adherence is number of missed dose.
Data Analysis
Collected data were entered into and cleared using Epi-data software version 3.1 and then exported to SPSS version 24 for further statistical analysis. A binary logistic regression was used to investigate factors associated with uptake of PT. Variables with p-value < 0.2 in bivariable analysis were entered into the multivariable analysis. Odds ratio with 95% confidence interval was estimated to show the strength of association and the p-value <0.05 was used to declare the statistical significance in the multivariable analysis.
Socio-demographic characteristics of participants
A total of 300 (293) were reviewed which were drawn from Mettu Karl referral and Darimu Hospitals. Most 279 (93%) of the respondents were female and 203 (66.9%) of them were married. 230 (76%) of the respondents were aged between 24-30 years of age and 148 (48%) were orthodox Christians. Regarding education level only 102 (3.4%) of respondents had primary school education and 80% of them reported an average monthly household income of less than 3000 Ethiopian birr. The results indicated that the majority 287 (95%) of the respondents were non-employed. Some form of non-employed engaged in private business about 99 (32.4%). 77(25.6%) of the respondents reported being casual laborers performing various jobs with the least being unemployed representing 33 (11%) and 12 (4%) governmental employed and 6 (2%) professional employed NGO.
Review of the records indicated that all children who were registered in the PMTCT register books and born from confirmed HIV-infected mothers in which more than half 158 (54%) of them were in the 13-18 month age group, 31% (90), 11% (32), 12% (35) between 6-12, 19-24, 25-28 months respectively (Figure 1).
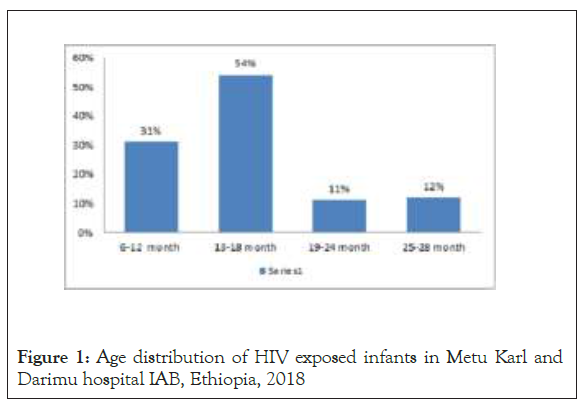
Figure 1: Age distribution of HIV exposed infants in Metu Karl and Darimu hospital IAB, Ethiopia, 2018
Awareness of guardians/care takers on preventive prophylaxis
Regarding the awareness of caretakers towards prophylactic treatment 191 (65.5%) of the care taker have awareness while 75(25.6%) of the respondents were not aware. The majority of participant 88.8% indicated that they had indeed suffered from one or more opportunistic infections.
Hospitalization and health facility related factors
The results indicate that nearly half of HIV exposed infants 44.1% had been hospitalized within the last one month and the cause of admission to hospital, diarrhea (18.4%), pneumonia (43.2%) while 9.6% reported having been admitted for various other reasons. 80.5% of the respondents has received regular supply of PT and 19.5% of respondents reported being unable to acquire the drug when they needed it.
The most common problem encountered in accessing Preventive therapy and other related care at the health facility was frequent drug out of stock (33.8%), followed by long hospital procedures (31.4%), Unfriendly hospital staff and long distance to the health facility (8.5%). Others like provision of social support 60.8% of respondents were reported not received any form of social support from the hospital while 115(39.2%) had received hospital based social support during their course of treatment. The reported social support consisted of counseling on positive living and nutritional advice.
Health care workers related factors
A total of 94 health care workers were interviewed and majority (99.2% )of the respondents got counseling during treatment in which the patients informed about their drug instructions, benefits of adherence and related issues on preventive therapy. More than half (66.7%) of the health care workers reported to have experienced unavailability of co-trimoxazole and isoniazid pediatric formulations in the health facilities. One-third (28.6%) of the health care workers reported that scarcity of the drug as the main reason for poor adherence and (19.0%) reported a lack of funds to purchase the drug in the hospitals has strong association with poor adherence. In the absence of co-trimoxazole syrup, approximately one-quarter (23.8%) of health care workers gave instructions to parents and guardians to prepare co-trimoxazole suspension using crushed tablets at home. Some health care workers (17.5%) were able to assist parents and guardians by making co-trimoxazole suspension using co-trimoxazole crushed tablets and (19.8%) requested parents and guardians to come back to the health facilities the next day with anticipation that the drug will be available during that time.
Independent predictors of preventive therapy uptake
The results from multiple logistic regressions analysis demonstrate the variables that statistically significant to preventive therapy uptake among HIV exposed children were long distance from home [AOR: 9.91(2.829-34.73);p=0.000], having persistent diarrhea [AOR: 4.32(1.06-17.53) p= 0.040], perceived to be cured from HIV/AIDS [AOR : 0.33 (0.128-0.850) 0.023] predictors of preventive therapy uptake.
Factors associated with preventive therapy uptake and challenges in its implementation were being Long distance from home nine times more challenged to uptake PT to counter parts [(2.829, 34.73); p=0.000],having persistent diarrhea four times more likely to uptake preventive therapy than their counterparts [(1.06, 17.53); p=0.040], perceived to be Cured from HIVAIDS is 67% more likely to uptake preventive therapy than to alleviate disease [(0.128- 0.850); p=0.023] and being missing dose is more than two times more likely to Uptake preventive therapy than regular users [(1.17- 6.26); P=0.022].
This study was conducted to assess the uptake and challenges preventive therapy and factors associated by using validated tools.
This finding of quantitative study in which two health facilities involved indicated, patient self-report and document review indicated that uptake in the month prior to the interview was good (82.6%) while the rest had poor uptake. This proportion of good uptake was higher than that of retrospective study in Addis Ababa 56%. This is possibly due to that almost all, [99.5% and 98.2%] of the respondents of this study had appropriate information of Preventive Therapy and approach towards Preventive Therapy use respectively.
In addition to this, 99.2% of the respondents got counseling during treatment in which the patients informed about their drug instructions, benefits of adherence and related issues on Preventive Therapy. But the above stated factors are not significant predictors of good uptakePreventive Therapy in the final multivariable analysis which may be due to confounding factors in the final model and the probable reason may be; there could be difference in the study population as well as different methods used. Long procedure in getting the drug, scarcity of the drug, number of missed dose, related medical problems and admission to hospital, and presence of opportunistic infection were statistically significant predictors of Preventive Therapy uptake in multivariable logistic regression analysis.
Multiple variable regressions was employed to assess whether there was any association between the various socio-demographic variables like age, level of education, occupation and Preventive Therapy up take. There was no significant association between socio-demographics factors and preventive Therapy uptake. But, Unable to read is associated with Uptake of Preventive Therapy but not significant with the study done in Tanzania (p=0.428) and was align with the study done in South Africa may be due to socio economic status.
The availability and affordability of Preventive Therapy and treatment services for opportunistic infections was variously noted as a major factor promoting its utilization is similar with study done in Tanzania. Most importantly, the fact that the drug was offered free of charge during HIV related care and management promoted a wider acceptability among care givers. However, occasional drug stock-outs compounded by long procedure (8.5%) for health services within the hospital were noted as the major barriers to Preventive Therapy uptake the utilization of HIV related care at the hospital which was higher than study done in Kenya (1.6%) this variation may be due to socio economic status or confounding effect. In addition, some of the respondents reported shortage of the drug (33.8%) to get to the facility only to be met by drug stock-outs at the hospital and this was a big contributor to poor adherence more higher than the study done Kenya and Tanzania 6.8%and 0.6% respectively may be due to economic status of the country and confounding effect of other variables.
Regarding counseling on awareness of opportunistic infections suffered as a result of HIV related diseases like diarrhea 18.4% [p=0.040, AOR 4.324 (1.067-17.530)] i.e. those individuals who got counselling was about 4.32 times more likely uptake to their counter parts, but it was lower than the study done in Kenya 28.9. This may be due to confounding effect of other variable. The main reason for admission to hospital (15%) were care takers awareness on use of PT about 25.6% do not know what to treat. it was higher than the study done in Tanzania (13.1%) [8].
The finding of this study indicated the number of missed dose was 60% which was higher than the study done in Tanzania (33%) that resulted in suffered from one or more an opportunistic infection. When asked about the cause of admission to hospital within the last one month, 43.9% of the respondents reported URTI as the cause of admission with 18.4% reporting diarrheal related diseases. The remaining 9.6% had been hospitalized from others. This can be attributed to the fact that poor adherence to Preventive Therapy is usually associated with increased rates of diarrhea, and hospitalization due to missed dose.
ART: Antiretroviral Therapy; CPT: Cotrimoxazole Preventive Therapy; CD4: Cluster of Differentiation; CDC: Communicable Disease Control, HIV: Human Immune Virus; HEI: HIV Exposed Infants; IPT: Isoniazid Preventive Therapy; OI: Opportunistic Infection; PCR/DNA: Polymerase Chain Reaction; PMTCT: Prevention to Mother to Child Transmission; PJP: Pneumocystis Jiroveri Pneumonia; PT: Preventive Therapy; RLS: Resource Limited Setting, WHO: World Health Organization
Authors would like to thank mothers for their willingness to participate in the study. The authors’ appreciation will also go to the Mettu University for provision of financial support as well as to Illu Aba Bor zone Health office for their positive cooperation during data collection.
Conceived and designed by TF, and TF. DN performed data analysis and interpreting of findings. TF prepares manuscript. Both authors read and approved the final manuscript.
No funding was obtained for this study.
The Authors declare that they have no competing interests.
Ethical clearance was obtained from the Institutional Review Board of Mettu University. An official permission letter was secured from the Illu Aba Bor Zone health office. All mothers were informed about the purpose of the study, and interview was held only with those who agreed to give verbal consent to participate. The right of a participant to withdraw from the study at any time, without any precondition was disclosed unequivocally. Moreover, the confidentiality of information was guaranteed by all data collectors and investigators by using code numbers rather than personal identifiers and by keeping the questionnaire locked.
Citation: Nigatu D, Fekede T (2021) Preventive Treatment Adherence and Challenges In Its Effective Implementation Among HIV Exposed Children In The Public Hospitals In Ilubabor Zone: Retrospective Follow-Up Study. Adv Pediatr Res 8:36.
Received: 02-Feb-2021 Accepted: 17-Mar-2021 Published: 24-Feb-2021 , DOI: 10.35248/2385-4529.21.8.36
Copyright: © 2021 Nigatu, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.