
Advances in Pediatric Research
Open Access
ISSN: 2385-4529

ISSN: 2385-4529
Research Article - (2024)Volume 11, Issue 1
Background: Epilepsy stands as a persistent and significant neurological disorder, ranking among the primary contributors to disability in Ethiopia.
Objective: To evaluate the risk factors for epilepsy among children undergoing follow-up at Yekatit 12 Hospital Medical college, Addis Ababa, Ethiopia.
Methods: An unmatched case-control study design was implemented to investigate epilepsy risk factors among patients attending the neurology clinic at Yekatit 12 Hospital Medical college, a teaching hospital in Addis Ababa, Ethiopia. The study included 87 cases selected from individuals with epilepsy and 174 controls chosen from non- epileptic patients attending the general pediatrics clinic at the same hospital during the same timeframe. Data on the identified risk factors were gathered through personal interviews using a structured questionnaire and by reviewing medical records. Subsequently, the collected data were coded, checked for accuracy and entered into Epi-Info-7. The information was then exported to SPSS version 26 for analysis. Bivariate and multivariate logistic regression analyses were conducted and both crude and adjusted odds ratios with 95% confidence intervals were calculated. A significance level of p<0.05 was employed to indicate statistical significance.
Results: Of the cases, 58 (66.7%) and among the controls, 95 (57.9%) had a mean age of 5.8 ± 4.0 and 5.8 ± 3.6 years, respectively. The probability of experiencing epilepsy was higher in children with a family history of epilepsy (AOR: 5.69, 95% CI (2.051, 15.84)), an APGAR score<6 (AOR: 7.51, 95% CI (1.55, 36.26)), a history of CNS infection (AOR: 14.26, 95% CI (3.28, 62.08)) and current neurological impairment (AOR: 8.07, 95% CI (1.10, 59.07)).
Conclusion: This study identified an increased likelihood of epilepsy in individuals with a family history of the condition, an APGAR score<6, a history of CNS infection and current neurological impairment.
Epilepsy; Head injury; Seizures; Child health; Y12HMC; Infection
AOR: Adjusted Odd Ratio; APGAR: Appearance, Pulse, Grimace, Activity and Respiration; CI: Confidence Interval; COR: Crude Odds Ratio; OR: Odd Ratio; SPSS: Statistical Package for Social Science Software; SSA: Sub-Saharan Africa; Y12HMC: Yekatit 12 Hospital Medical College; CNS: Central Nervous System; SVD: Spontaneous Vaginal Delivery
Epilepsy is a neurological disorder defined by the occurrence of two or more unprovoked seizures unrelated to acute metabolic disorders. It may result in loss of consciousness, disruptions in movement and disturbances in sensation (including vision, hearing and taste), autonomic function, mood and mental processes [1]. Epilepsy stands as the most prevalent neurological disorder globally, affecting 50 million individuals, with roughly 80% residing in resource-limited developing countries. The highest incidence of epilepsy occurs during childhood [2].
The overall lifetime occurrence of epilepsy is 3%, with over half of the cases initiating in childhood. The annual prevalence is estimated at 0.5-1.0% [3]. Worldwide, epilepsy impacts over 50 million individuals and around 85% of those affected reside in developing countries, including Ethiopia [4].
The elevated incidence of epilepsy in developing countries is attributed to a higher risk of acute and chronic brain infections, along with pre and post-natal obstetric complications that may result in brain damage [5]. While there is published data on the incidence of epilepsy in sub-Saharan Africa, the comprehensive information indicates a notably higher annual incidence in less developed countries at 81.7 per 100,000 compared to 45.0 per 100,000 in more developed countries [6]. The prevalence of epilepsy stood at 5.2 per 1000 individuals at risk, with rates of 5.8 for males and 4.6 for females. The peak age-specific prevalence was observed in the 10-19 years’ age group [7].
The impact of epilepsy in children extends across social, emotional and overall family functioning. Particularly in Africa, epilepsy remains stigmatized, largely due to traditional beliefs associating it with spirituality [8].
While there is compelling evidence indicating specific etiological factors for epilepsy, the cause remains unknown in approximately 70% of cases. Risk factors for epilepsy vary between childhood and later stages of life and encompass conditions linked to an elevated occurrence of epilepsy. These factors include head injury, perinatal insults, Central Nervous System (CNS) infections and febrile convulsions [9].
Advancements in comprehending this debilitating disease have been made through data derived from the aetiology, epidemiology and historical aspects of epilepsy. However, investigations from various countries indicate that the causes of epilepsy remain incompletely understood [10]. For example, in pediatric research, approximately 60-70% of children diagnosed with epilepsy are identified to have either idiopathic or cryptogenic epilepsy [11]. However, the study area lacks adequate research on the scope of the problem and its underlying factors, hindering the formulation of informed policies. Therefore, precise identification of the risk factors for epilepsy could potentially empower us to formulate strategies for its prevention.
The research was conducted at Yekatit 12 Hospital Medical college, a teaching hospital located in Addis Ababa, Ethiopia. The study spanned from March 2023 to August 2023 and employed an unmatched case-control design. The cases included children diagnosed with epilepsy, while the controls encompassed children without epilepsy, all receiving care at the Medical College Hospital. Informed consent was obtained from the guardians of the participating children. The study focused on children aged 3 months to 14 years clinically diagnosed with epilepsy, characterized by the occurrence of two or more unprovoked seizures consecutively within the preceding period. Exclusions comprised children with only febrile seizures and those with significant comorbidities, such as notable mental sub-normality or systemic diseases. Controls were children aged 3 months to 14 years without epilepsy attending the same hospital.
Structured questionnaires were administered to parents or guardians of the children, adapting the questionnaire through a comprehensive review of existing literature and similar previous studies. Following a pre-test and subsequent adjustments, clinical information for the children was retrieved from their medical records. Each respondent underwent an individual interview, where they were seated and given a detailed overview of the study's objectives, the assurance of confidentiality and clear explanations of key terms.
After conducting data completeness checks, the information was entered into Epi-info version 7 and subsequently exported to Statistical Package for Social Science Software (SPSS) version 26 for further data cleaning and analysis. Continuous variables were summarized using mean and standard deviation, while categorical variables were expressed as relative frequencies or proportions. To investigate the association between independent variables and the dependent variable, binary logistic regression analysis was utilized.
During the bivariate analysis, independent variables with a p-value of <0.2 were considered for inclusion in the multivariable analysis model. Ultimately, independent variables with a p-value <0.05 were considered statistically significant.
Socio-demographic characteristics of the participants
In this study, a total of 251 participants were included, consisting of 87 previously diagnosed epilepsy patients (cases) and 164 controls, yielding a response rate of 96.2%. Among the cases, 58 (66.7%) had a mean age of 5.8 ± 4.0 years, while in the control group, 95 (57.9%) had a mean age of 5.8 ± 3.6 years. The majority of both cases (88.5%) and controls (82.3%) were born to mothers under the age of 35. In terms of maternal education, 15 (17.2%) of the cases and 21 (12.8%) of the controls had no formal education. Notably, 28.7% of cases had a family history of epilepsy compared to 6.7% among the controls (refer to Table 1).
| Variables | Cases (n=87) | Controls (n=164) | ||
|---|---|---|---|---|
| Frequency (n) | Percent (%) | Frequency (n) | Percent (%) | |
| Age in years | ||||
| <6 years | 47 | 54 | 90 | 54.9 |
| 6 years and above | 40 | 46 | 74 | 45.1 |
| Maternal age at the time of delivery | ||||
| <35 years | 77 | 88.5 | 135 | 82.3 |
| 35 years and above | 10 | 11.5 | 29 | 17.7 |
| Mother’ educational status | ||||
| No formal education | 15 | 17.2 | 21 | 12.8 |
| Primary education | 26 | 29.9 | 52 | 31.7 |
| Secondary education | 25 | 28.7 | 46 | 28 |
| College/university | 21 | 24.1 | 45 | 27.4 |
| Family history of epilepsy | ||||
| Yes | 25 | 28.7 | 11 | 6.7 |
| No | 62 | 71.3 | 152 | 92.7 |
Table 1: Socio-demographic characteristics among cases and controls in among children on follow-up at Yekatit 12 Hospital Medical college, Addis Ababa, Ethiopia, 2023.
Maternal factors
Regarding maternal factors, a considerable 17.9% of cases had a history of hypertension, whereas only 9.9% among the controls had a maternal history of hypertension. Additionally, a small percentage, 3.8% of cases and 1.3% of controls, reported a maternal history of gestational diabetes. However, maternal infection during pregnancy was notably higher among cases, with 20.9%, compared to 3.1% among controls. History of drug intake during pregnancy was reported by 10.3% of mothers with epileptic children, while a smaller proportion (5.5%) of mothers without epileptic children had a history of drug intake. Furthermore, a substantial 18.4% of mothers with epileptic children had a history of spontaneous abortion, whereas 13.6% of mothers without epileptic children reported a similar history (refer to Table 2).
| Variable | Cases | Controls | ||
|---|---|---|---|---|
| Frequency (n=87) | Percent (%) | Frequency (n=164) | Percent (%) | |
| Maternal hypertension history | ||||
| Yes | 15 | 17.9 | 15 | 9.9 |
| No | 69 | 82.1 | 136 | 90.1 |
| Maternal gestational diabetes history | ||||
| Yes | 3 | 3.8 | 2 | 1.3 |
| No | 76 | 96.2 | 150 | 98.7 |
| Maternal infection | ||||
| Yes | 18 | 20.9 | 5 | 3.1 |
| No | 68 | 79.1 | 155 | 96.9 |
| Maternal history of drug intake | ||||
| Yes | 9 | 10.3 | 9 | 5.5 |
| No | 78 | 89.7 | 154 | 94.5 |
| Maternal history of spontaneous abortion | ||||
| Yes | 16 | 18.4 | 22 | 13.6 |
| No | 71 | 81.6 | 140 | 86.4 |
Table 2: Proportion of maternal factors for epilepsy between cases and controls among children on follow-up at Yekatit 12 Hospital Medical college, Addis Ababa, Ethiopia, 2023.
Perinatal factors
A notable proportion (10.3%) of children diagnosed with the disease and 6.1% among the control group were delivered at home. Concerning the mode of delivery, 70.1% of children with the disease and 75.0% of controls underwent Spontaneous Vaginal Delivery (SVD). Among these deliveries, nearly onethird of children with epilepsy and 26 (15.9%) of controls experienced prolonged labor. Moreover, 11 (12.6%) of children with epilepsy and 15 (9.1%) of controls were uncertain about whether they had prolonged labor during birth. During the delivery process, almost a quarter of children with epilepsy and 10 (6.2%) of controls either had an Appearance, Pulse, Grimace, Activity and Respiration (APGAR) score<6 or did not cry (refer to Table 3).
| Variables | Cases | Controls | ||
|---|---|---|---|---|
| Frequency (n=87) | Percent (%) | Frequency (n=164) | Percent (%) | |
| Place of delivery | ||||
| Home | 9 | 10.3 | 10 | 6.1 |
| Health facility | 78 | 89.7 | 154 | 93.9 |
| Mode of delivery | ||||
| Cesarean section | 26 | 29.9 | 41 | 25 |
| SVD | 61 | 70.1 | 123 | 75 |
| Prolonged labor | ||||
| Yes | 26 | 34.2 | 26 | 17.4 |
| No | 50 | 65.8 | 123 | 82.6 |
| APGAR<6/didn’t cry | ||||
| Yes | 28 | 32.9 | 10 | 6.2 |
| No | 57 | 67.1 | 150 | 93.8 |
| Pre or post term delivery | ||||
| Yes | 9 | 11.5 | 11 | 7.4 |
| No | 69 | 88.5 | 138 | 92.6 |
Note: SVD: Spontaneous Vaginal Delivery; APGAR: Appearance, Pulse, Grimace, Activity and Respiration.
Table 3: Proportion of perinatal risk factors for epilepsy among cases and controls among children on follow-up at Yekatit 12 Hospital Medical college, Addis Ababa, Ethiopia, 2023.
Postnatal factors
The data suggests a notable disparity in the prevalence of febrile convulsions and neurologic impairment between children with epileptic disease and the control group. Additionally, the incidences of head injury, CNS infection and CNS malformation appear to be more pronounced among those diagnosed with epilepsy.
Among the entire pool of study participants, 13 (14.9%) of children diagnosed with epileptic disease and 9 (5.5%) of the control group had a history of febrile convulsions. Similarly, 24 (27.6%) of children with epileptic disease and 4 (2.4%) of the controls exhibited neurologic impairment. The occurrences of head injury, CNS infection and CNS malformation were 1 (1.1%), 19 (21.8%) and 11 (12.6%) among cases, respectively (refer to Figure 1).
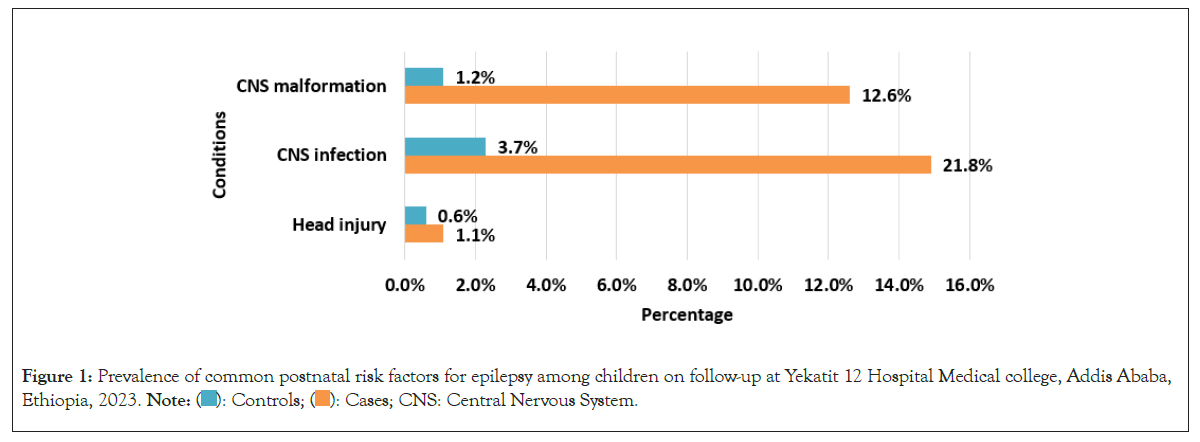
Figure 1: Prevalence of common postnatal risk factors for epilepsy among children on follow-up at Yekatit 12 Hospital Medical college, Addis Ababa,
Ethiopia, 2023. 
Factors associated with epilepsy
Both bivariate and multivariable logistic regression analyses were employed to ascertain the factors linked with epilepsy. During the bivariate analysis, factors such as the age of the child, maternal age at the time of delivery, family history of epilepsy, maternal history of hypertension, maternal infection, maternal history of drug intake, APGAR score<6 or absence of crying, prolonged labor, febrile convulsions, CNS infection and existing neurological impairment displayed a p-value of less than 0.25, prompting their inclusion in the subsequent multivariable analysis. This process aimed to identify and confirm factors independently associated with epilepsy in the studied population.
Following the adjustment for potential confounding variables through multivariate logistic regression analysis, four variables-family history of epilepsy, APGAR score<6 or absence of crying during birth, history of CNS infection and current neurologic impairment-emerged as independent factors associated with epileptic disease, exhibiting a statistically significant p-value of less than 0.05. This indicates that even after accounting for other variables, these four factors retained their individual significance in influencing the occurrence of epileptic disease in the studied population.
In the analysis incorporating multiple variables, it was revealed that the likelihood of being diagnosed with epilepsy was notably elevated among certain groups of children. Specifically, those with a family history of epilepsy (AOR: 5.69, 95% CI: 2.05, 15.84), those who scored an APGAR<6 or did not cry during birth (AOR: 7.51, 95% CI: 1.55, 36.26), individuals with a history of CNS infection (AOR: 14.26, 95% CI: 3.28, 6.08) and those currently experiencing neurological impairment (AOR: 8.07, 95% CI: 1.10, 9.07) demonstrated statistically significant associations with epilepsy in the study setting (Table 4).
| Variables | Epilepsy | COR (95% CI) | AOR (95% CI) | p-value | |
|---|---|---|---|---|---|
| Cases (%) | Controls (%) | ||||
| Maternal age at the time of delivery | |||||
| <35 years | 77 (88.5) | 135 (82.3) | 1.65 (0.76, 3.58) | 1.75 (0.56, 5.47) | 0.33 |
| 35 years and above | 10 (11.5) | 29 (17.7) | 1 | 1 | - |
| Family history of Epilepsy | |||||
| Yes | 25 (28.7) | 11 (6.7) | 5.57 (2.58, 12.01) | 5.69 (2.05, 15.84) | 0.001 |
| No | 62 (71.3) | 152(93.3) | 1 | 1 | - |
| Maternal hypertension history | |||||
| Yes | 15 (17.9) | 15 (9.9) | 1.97 (0.91, 4.26) | 1.09 (0.29, 4.05) | 0.9 |
| No | 69 (82.1) | 136 (90.1) | 1 | 1 | - |
| Maternal infection | |||||
| Yes | 18 (20.9) | 5 (3.1) | 8.21 (2.93, 23.01) | 3.86 (0.78, 19.22) | 0.099 |
| No | 68 (79.1) | 155 (96.9) | 1 | 1 | -- |
| Maternal history of drug intake | |||||
| Yes | 9 (10.3) | 9 (5.5) | 1.97 (0.75, 5.17) | 0.21 (0.03, 1.60) | 0.133 |
| No | 78 (89.7) | 154 (94.5) | 1 | 1 | - |
| APGAR<6/didn’t cry at birth | |||||
| Yes | 28 (32.9) | 10 (6.3) | 7.37 (3.36, 16.13) | 7.51 (1.55, 36.26) | 0.012 |
| No | 57 (67.1) | 150 (93.8) | 1 | 1 | - |
| Prolonged labor | |||||
| Yes | 26 (34.2) | 26 (17.4) | 2.46 (1.30, 4.64) | 0.87 (0.30, 2.55) | 0.8 |
| No | 50 (65.8) | 133 (82.6) | 1 | 1 | - |
| Febrile convulsions | |||||
| Yes | 13 (14.9) | 9 (5.5) | 3.03 (1.24, 7.40) | 2.49 (0.72, 8.63) | 0.151 |
| No | 74 (85.1) | 155 (94.5) | 1 | 1 | - |
| CNS infection | |||||
| Yes | 19 (22.1) | 6 (3.7) | 7.45 (2.47, 19.53) | 14.26 (3.28, 6.08) | 0.001 |
| No | 67 (77.9) | 158 (96.3) | 1 | 1 | - |
| Neurological impairment | |||||
| Yes | 24 (27.6) | 4 (2.4) | 15.24 (5.08, 45.68) | 8.07 (1.10, 9.07) | 0.040 |
| No | 63 (72.4) | 160 (97.6) | 1 | 1 | - |
Note: AOR: Adjusted Odds Ratio; COR: Crude Odds Ratio; 1: Reference category; CNS: Central Nervous System; P: Probability; CI: Confidence Interval; APGAR: Appearance, Pulse, Grimace, Activity and Respiration.
Table 4: Variables linked to epilepsy in children undergoing follow-up at Yekatit 12 Hospital Medical college in Addis Ababa, Ethiopia, in the year 2023.
In the bivariate analysis of this study, various factors exhibited a noteworthy association with epilepsy. However, upon conducting multivariate logistic regression analysis, only a family history of epilepsy, an APGAR score<6 or absence of crying during birth, a history of CNS infection and current neurologic impairment demonstrated statistically significant associations with epilepsy. This suggests that, when considering multiple factors simultaneously, these specific variables retained their significance in relation to the occurrence of epilepsy.
In the findings of this research, a strong relationship was identified between epilepsy and a familial history of the condition (AOR: 5.69, 95% CI (2.05, 15.84)). This discovery aligns with results from previous studies conducted in Kenya, Tanzania and India. The consistency of these findings across diverse geographical locations supports the notion that a family history of epilepsy may be a significant factor influencing the occurrence of the condition [12-14].
The findings indicated a noteworthy connection between individuals with an APGAR score<6 or those who did not cry during birth (AOR: 7.51, 95% CI (1.55, 36.26)) and the likelihood of developing epilepsy. This observation is consistent with comparable outcomes identified in research conducted in Sub-Saharan African (SSA) countries, such as Kenya and Tanzania. This underscores the consistency of the association across diverse populations in the SSA region and India [12- 15].
Within this study, children with a prior history of central nervous system infection exhibited a 14-fold higher likelihood of experiencing epilepsy compared to those without such a history. These findings are consistent with a communitybased study conducted in Tanzania, reinforcing the association between CNS infections and the increased risk of epilepsy in children and a study done in Turkey [15,16]. In contrast, a study conducted in Jordan revealed that although there were more patients with a history of central nervous system infection compared to controls, this difference did not reach statistical significance. This suggests that, unlike the findings in the current study, the association between a history of CNS infection and the occurrence of epilepsy was not statistically significant in the Jordanian study [17].
Lastly, there was a strong likelihood of an association between current neurologic impairment and epilepsy, with individuals experiencing an 8-fold increase in the odds (AOR: 8.07, 95% CI (1.10, 9.07)). Similar findings have been reported in other studies involving children from Tanzania, reinforcing the connection between present neurologic impairment and the heightened risk of epilepsy [15]. It is probable that this relationship is not causative but rather stems from a shared aetiology influencing both epilepsy and cognitive impairment. Support for this hypothesis is evident in studies indicating that cognitive impairment occurred before the onset of seizures. This suggests a common underlying factor contributing to both conditions rather than one directly causing the other [18].
It is crucial to recognize the limitations inherent in this study. While it contributes to the limited body of research on predictors of epilepsy, it is important to note certain drawbacks, including its retrospective design and the relatively smaller sample size. These limitations imply that the findings should be interpreted with caution and future studies with larger sample sizes and prospective designs may provide a more comprehensive understanding of the predictors of epilepsy.
In summary, this study emphasizes an increased susceptibility to epilepsy within the population under analysis. Specifically, it identifies certain factors such as a family history of epilepsy, a low Apgar score (<6) or lack of crying at birth, prior history of Central Nervous System (CNS) infection and pre-existing neurological impairment as statistically significant association with epilepsy among patients receiving care at Yekatit 12 Hospital Medical College in Addis Ababa, Ethiopia. These findings underline the importance of recognizing and addressing these risk factors in clinical settings to enhance the management and potentially prevent the onset of epilepsy in affected individuals. Further research and targeted interventions may contribute to alleviating the burden of epilepsy within this population and enhancing overall patient outcomes.
This study adhered to the principles outlined in the Helsinki Declaration concerning research involving human subjects. The Institutional Review Board of Yekatit 12 Hospital Medical college granted ethical clearance (Ref. No: Y12HMC/289/01/23). Prior to participation, participants were briefed on the study's objectives and informed consent was obtained individually. For participants below the age of 18, consent was acquired from their parents or guardians, along with obtaining assent from the participants themselves. Rigorous training was provided to data collection facilitators to ensure the confidentiality of participant information. Additionally, participants were informed of their rights, including the option to decline participation or withdraw from the study at any point.
Not applicable.
The authors declare that they have no conflict of interest.
The authors state that no funding was involved.
MT (pediatrician, academic and research vice provost at the Yekatit 12 Hospital Medical college, Addis Ababa, Ethiopia) contributed to the conception of the idea, proposal design, development and revisions; conducted data collection and analysis; interpreted the results and participated in reviewing and editing the manuscript. TM (pediatrician at the Mizan Tepi University Hospital, Tepi, Ethiopia) was involved in proposal design, amendments, data analysis, interpretation of results and took the lead in drafting the initial manuscript. TM also played a role in reviewing and editing the manuscript for intellectual content. All authors have read and given approval for the final version of the manuscript to be published.
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Alemu MT, Nigusie TM (2024) Risk Factors for Epilepsy in Pediatric Patients Undergoing Follow-Up at Yekatit 12 Hospital Medical College, Addis Ababa, Ethiopia: A Case-Control Study. Adv Pediatr Res. 11:075.
Received: 12-Feb-2024, Manuscript No. LDAPR-24-29568; Editor assigned: 14-Feb-2024, Pre QC No. LDAPR-24-29568 (PQ); Reviewed: 28-Feb-2024, QC No. LDAPR-24-29568; Revised: 06-Mar-2024, Manuscript No. LDAPR-24-29568 (R); Published: 13-Mar-2024 , DOI: 10.35248/2385-4529.24.11.075
Copyright: © 2024 Alemu MT, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.