
Advances in Pediatric Research
Open Access
ISSN: 2385-4529

ISSN: 2385-4529
Research Article - (2024)Volume 11, Issue 3
Background: Urological anomalies are the most common associated anomalies in patients with anorectal. Most publications state an incidence of between 30% and 50%, with the frequency of relation increasing proportionally with the complexity of anorectal malformations. Therefore, to enable early diagnosis and management of these abnormalities, a high index of suspicion is needed. In addition, long-term follow-up of patients with anorectal malformations and surveillance of their kidney function and urinary tract anatomy is of great importance to prevent damage to the urinary system.
Objectives: To identify and classify the urological anomalies associated with anorectal malformation patients admitted to Pediatric Surgery Department in Alexandria University Children’s Hospital from June 2021 to June 2023 and to correlate urological anomalies with the level of anorectal malformation.
Patients and methods: This study involved collection of data of all patients diagnosed with anorectal malformations between June 2021 and June 2023 who attended at Alexandria Pediatric Surgery Department of Alexandria University Children’s Hospital. Patients who were diagnosed with anorectal malformations and underwent urological screening. The following data were extracted from the patient’s files who met the inclusion criteria: Neonatal presentation, age at presentation, weight, sex and findings of genital examination.
Results: In 66 patients with ARM, 19 (28.7%) patients had Low Anorectal Anomaly (LARA) and High Anorectal Anomaly (HARA) were found in 47 (71.2%) patients. The incidence of ARM was higher in male patients than in female patients regardless the level of ARM. The most common genital anomaly among male patients was bifid scrotum, which was found in 3 out of 15 with genital anomaly, followed by hypospadias. In female patients, isolated cloaca anomaly was the most frequent genital anomaly.
Conclusion: Screening of associated urological anomalies is vital to prevent renal damage and reduce morbidity and mortality in patients with anorectal malformations.
Anorectal malformations; Hydronephrosis; Cloaca; Urogenital; Hypospadias; Vesicoureteral reflux
Anorectal Malformations (ARM) are one of the most common congenital anomalies that are encountered in pediatric surgical practices [1]. The global incidence of anorectal malformation is approximately 1 in every 4,000 to 5,000 live births, with slight male predominance. Approximately 50% of children with ARM have related abnormalities. The total incidence of related abnormalities was found to be 78% in a study to assess the prevalence of ARM according to the Krickenbeck anatomical classification. These associated anomalies involve vertebral, gastrointestinal, cardiovascular, trachea-esophageal, genitourinary and skeletal anomalies i.e., one or more components of Vertebral defects, Anal atresia, Cardiac defects, Tracheo-esophageal fistula, Renal anomalies, And Limb abnormalities (VACTERL) association [2-6].
Urological anomalies are the most common associated anomalies in patients with ARM. Most publications state an incidence of between 30% and 50%, with the frequency of relation increasing proportionally with the complexity of ARM. Therefore, to enable early diagnosis and management of these abnormalities, a high index of suspicion is needed. In addition, long-term follow-up of patients with ARM and surveillance of their kidney function and urinary tract anatomy is of great importance to prevent damage to the urinary system [7].
Urological anomalies are defined as birth defects involving the urological (i.e., kidney, ureter and urinary bladder) and genital system (i.e., penis, urethral and scrotum in males and vagina, cervix or uterus in females). These urological anomalies associated with ARM include hydronephrosis, Vesicoureteral Reflux (VUR), solitary kidney, ectopic kidney or pelvic kidney, horseshoe kidney, Pelvic-Ureteric Junction Obstruction (PUJO), Lower Urinary Tract Dysfunction (LUTD), hypospadias, Undescended Testis (UDT), ambiguous genitalia, hypoplastic uterus, vaginal atresia and bifida scrotum [5,8,9].
The most frequent congenital urological problem linked to ARMs is absent kidney, which can either be a fully absent kidney or rather a remnant kidney that is non-functionally multicystic or dysplastic. Prenatal ultrasonography can identify this aberration when it shows a hypertrophied single kidney as an adaptive response. Postnatal screening with ultrasound and Magnetic Resonance Imaging of Urinary Tract (MRU), together with renal radionuclide scintigraphy with a Dimercaptosuccinic Acid (DMSA) can confirm the presence of this anomaly. Renal function of this kidney should be monitored regularly and those with concurrent VUR should be managed adequately according to its grade [7,10].
Hydronephrosis (unilateral or bilateral) or hydronephrosis along with megaureter are not uncommon in patient with ARM. This anomaly can be either due to obstructive or non-obstructive etiologies. When a patient has hydronephrosis with megaureter, this can be due to severe VUR or due to Uretervesical Junction Obstruction (UVJO) cause by extrinsic compression in patients with cloacal type. This study aimed to identify and classify the urological anomalies associated with anorectal malformation patients admitted to Pediatric Surgery department in Alexandria University Children’s Hospital from June 2021 to June 2023 and to correlate urological anomalies with the level of anorectal malformation [11].
This study was a retrospective observational study conducted at Alexandria University Children’s Hospital in the Pediatric Surgery Department.
Patients
This study involved collection of data of all patients diagnosed with anorectal malformations between June 2021 and June 2023 who attended at Alexandria Pediatric Surgery Department of Alexandria University Children’s Hospital. Including the patients who were diagnosed with anorectal malformations and underwent urological screening. The following data were extracted from the patient’s files who met the inclusion criteria: Neonatal presentation, age at presentation, weight, sex and findings of genital examination.
Type of anorectal malformations which were classified based on the 1984 Wingspread classification for statistical analysis as a LARA which included rectoperineal fistula, imperforate anus without fistula (low) when the rectal pouch found at less than 1 cm from perianal skin or below the coccyx on the cross-table lateral radiographic film and HARA which included anomalies such as recto-bladder neck fistula, rectourethral (prostatic or bulbar) fistula, rectovestibular fistula, persistent cloaca with common channel less than or more than 3 cm, imperforate anus without fistula (high) when rectal pouch found more than 1 cm from perianal skin or above the coccyx on the radiographic film. Renal and bladder ultrasonography at neonatal period was done in all patients. Other urological investigations Voiding Cystourethrogram (VCUG), Magnetic Resonance Urography (MRU), Diethylenetriamine Pentaacetate (DTPA) renal scan or Dimercapto-Succinic Acid (DMSA) renal scan, urodynamics, sacral radiography and spinal cord ultrasonography or magnetic resonance imaging done accordingly when patients had abnormal findings of renal bladder ultrasonography. Also, pelvic ultrasound and magnetic resonance imaging was done in patients with cloacal malformation to detect vaginal and uterus anomalies. Also genital examination performed in all patients either male or female searching for hypospadias, maldescended testicles, urogenital sinus or cloacal anomalies.
A total of 66 patients with ARM data were analyzed for the study, 42 (63.6%) were males and 24 (36.4%) were females. The patients were diagnosed during neonatal period with mean age of 1.48 ± 0.73 days. Their median weight at presentation in the neonatal period was 2.80 (2.50-3.0) kg.
In 66 patients with ARM, 19 (28.7%) patients had LARA and HARA were found in 47 (71.2%) patients. The incidence of ARM was higher in male patients than in female patients regardless the level of ARM and this was statistically significant with p value <0.024 when comparing LARA with HARA according to sex as shown in Table 1.
| Sex | Total (n=66) | LARA (n=19) | HARA (n=47) | χ² | p | |||
|---|---|---|---|---|---|---|---|---|
| No. | % | No. | % | No. | % | |||
| Male | 42 | 63.6 | 16 | 84.2 | 26 | 55.3 | 4.881* | 0.024* |
| Female | 24 | 36.4 | 3 | 15.8 | 21 | 44.7 | ||
Note: Low Anorectal Anomaly; HARA: High Anorectal Anomaly; χ²: Chi-square.
Table 1: Comparison between LARA and HARA according to sex.
The most common anomaly among male patients with ARM was imperforate anus without fistula with incidence of 13 (31.0%), while rectovestibular fistula was the most frequent anomaly identified among female patients with incidence of 14 (58.3%), as shown in Table 2.
| Type of Anorectal Malformations (ARM) | Total (n=66) | Sex | ||||
|---|---|---|---|---|---|---|
| Males (n=42) | Females (n=24) | |||||
| No. | % | No. | % | No. | % | |
| Rectoperineal fistula | 9 | 13.6 | 6 | 14.3 | 3 | 12.5 |
| Low imperforate anus without fistula | 10 | 15.2 | 10 | 23.8 | 0 | 0 |
| Rectourethral fistula | 8 | 12.1 | 8 | 19 | 0 | 0 |
| Rectobladder neck fistula | 5 | 7.6 | 5 | 11.9 | 0 | 0 |
| Rectovestibular fistula | 14 | 21.2 | 0 | 0 | 14 | 58.3 |
| High imperforate anus without fistula | 14 | 21.2 | 13 | 31 | 1 | 4.2 |
| Cloaca | 6 | 9.1 | 0 | 0 | 6 | 25 |
Table 2: Distribution of type of Anorectal Malformations (ARM) according to sex.
Based on the genital examination findings, 51 (77.3%) patients had normal findings and 15 (22.7%) patients had abnormal findings as shown in Table 3. The most common genital anomaly among male patients was bifid scrotum, which was found in 3 out of 15 with genital anomaly, followed by hypospadias. In female patients, isolated cloaca anomaly was the most frequent genital anomaly. Other genital anomalies are as shown in Table 4.
| Genital examination findings | Total (n=66) | Sex | ||||
|---|---|---|---|---|---|---|
| Males (n=42) | Females (n=24) | |||||
| No. | % | No. | % | No. | % | |
| Normal | 51 | 77.3 | 33 | 78.6 | 18 | 75 |
| Abnormal | 15 | 22.7 | 9 | 21.4 | 6 | 25 |
Table 3: Genital examination findings according to sex.
| Sex | Genital anomalies | Number | % |
|---|---|---|---|
| Male | Bifid scrotum | 3 | 4.54 |
| Distal hypospadias | 2 | 3.03 | |
| Proximal hypospadias with bifid scrotum | 2 | 3.03 | |
| Undescended testis | 2 | 3.03 | |
| Female | Isolated cloaca | 3 | 4.54 |
| Hydrocolpos+bicornuate uterus | 2 | 3.03 | |
| Uterus+vaginal atresia | 1 | 1.51 | |
| Total | 15 | 22.7 |
Table 4: Associated genital anomalies in 15 of 66 (22.7%) patients with Anorectal Malformations (ARM).
Renal ultrasound assessment was performed in all patients during the neonatal period, while 59 (89.4%) normal and 7 (10.6%) as shown in Table 5. VCUG was done in patients who had abnormal renal ultrasound findings and VUR was detected in 2 out of 7 of those patients. Absent kidney, multicystic kidney and VUR were the most common urological anomalies as shown in Table 6.
| Renal US findings | Total (n=66) | Sex | ||||
|---|---|---|---|---|---|---|
| Males (n=42) | Females (n=24) | |||||
| No. | % | No. | % | No. | % | |
| Normal | 59 | 89.4 | 39 | 92.9 | 20 | 83.3 |
| Abnormal | 7 | 10.6 | 3 | 7.1 | 4 | 16.7 |
Note: US: Ultra Sound.
Table 5: Renal ultrasound findings according to sex.
| Urological anomalies | Number | % |
|---|---|---|
| Absent kidney | 2 | 3.03 |
| Multicystic kidney+hydronephrosis | 1 | 1.51 |
| Multicystic kidney+megaureter+ectopic ureter | 1 | 1.51 |
| Vesicoureteral reflux | 1 | 1.51 |
| Vesicoureteral reflux+duplicating ureter | 1 | 1.51 |
| Horseshoe kidney | 1 | 1.51 |
| Total | 7 | 10.60% |
Table 6: Associated urological anomalies in 7 of 66 (10.6%) patients with Anorectal Malformations (ARM).
In some patients (n=5) more than one anomaly was associated, in male patients, 2 patients had unilateral absent kidney associated with distal penile hypospadias and undescended testis in each. Among female patients with cloaca malformation, 1 patient had left moderate hydronephrosis with right multicystic kidney, 1 patient had left multicystic kidney with left megaureter and right ectopic ureter and another had bilateral VUR with duplicating left ureter.
The overall incidence of urogenital anomalies was 22 out of 66 (33.3%) ARM patients where by 12 (18%) and 10 (15%) were males and females respectively. Among male patients, 1 had urological anomaly, 9 had genital anomalies and 2 had urogenital anomalies, while female patients 4 had urological anomalies, 3 had genital anomalies and other 3 had urogenital anomalies as shown in Figure 1 and Table 7.
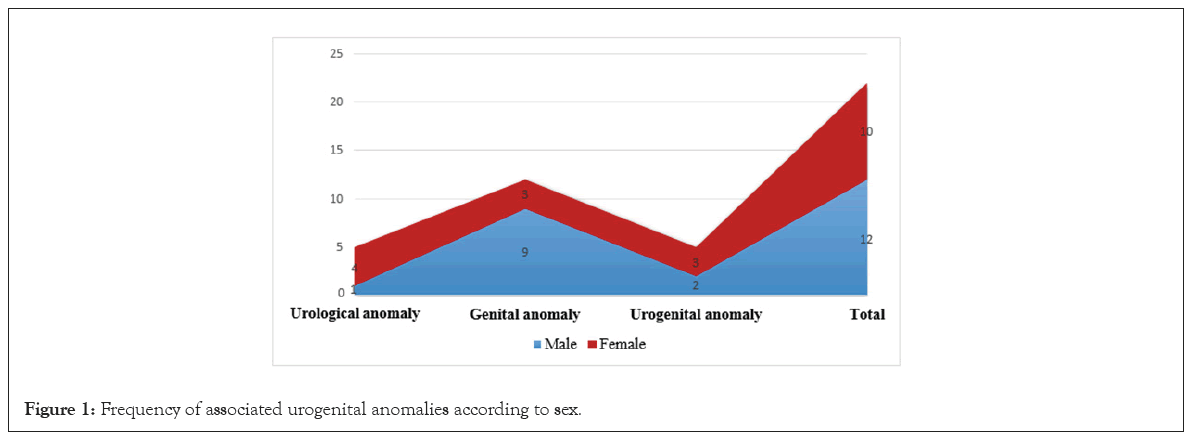
Figure 1: Frequency of associated urogenital anomalies according to sex.
| Sex | Urological anomaly | Genital anomaly | Urogenital anomaly | Total |
|---|---|---|---|---|
| Male 42(63.6%) | 1 (1.5%) | 9 (13.6%) | 2 (3.03%) | 12 (18.1%) |
| Female 24(36.4%) | 4 (6.06%) | 3 (4.55%) | 3 (4.55%) | 10 (15.0%) |
| Total 66 | 5 (7.58%) | 12 (18.1%) | 5 (7.58%) | 22 (33.3%) |
Table 7: Frequency of associated urogenital anomalies in 66 patients with Anorectal Malformations (ARM) according to sex.
Among 47 patients with HARA, 7 patients had urological anomalies and 13 patients had genital anomalies while only 2 patients with genital anomalies were found with LARA as shown in Table 8. Urological and genital anomalies are more frequently seen in HARA than LARA patients as shown in Table 9.
| Type of ARM | Number | Urological anomaly | Genital anomaly |
|---|---|---|---|
| HARA | 47 (71.2%) | 7 (14.9%) | 13 (27.7%) |
| LARA | 19 (28.8%) | 0 (0.00%) | 2 (10.5%) |
| Total | 66 | 7 (10.6%) | 15 (22.7%) |
Note: Low Anorectal Anomaly; HARA: High Anorectal Anomaly; ARM: Anorectal Malformations.
Table 8: Frequency of associated urogenital anomalies in 66 patients with anorectal malformations according to the level of deformity.
| Urological anomalies | Total (n=66) | LARA (n=19) | HARA (n=47) | |||
|---|---|---|---|---|---|---|
| No. | % | No. | % | No. | % | |
| Absent kidney | 2 | 3 | 0 | 0 | 2 | 4.3 |
| Horseshoe kidney | 1 | 1.5 | 0 | 0 | 1 | 2.1 |
| Multicystic kidney | 2 | 3 | 0 | 0 | 2 | 4.3 |
| Hydronephrosis | 1 | 1.5 | 0 | 0 | 1 | 2.1 |
| Megaureter | 1 | 1.5 | 0 | 0 | 1 | 2.1 |
| Ectopic ureter | 1 | 1.5 | 0 | 0 | 1 | 2.1 |
| Duplicating ureter | 1 | 1.5 | 0 | 0 | 1 | 2.1 |
| Vesicoureteral reflux | 2 | 3 | 0 | 0 | 2 | 4.3 |
| Bifida scrotum | 5 | 7.6 | 1 | 5.3 | 4 | 8.5 |
| Hypospadias | 6 | 9.1 | 1 | 5.3 | 5 | 10.6 |
| Undescended testis | 2 | 3 | 0 | 0 | 2 | 4.3 |
| Hydrocolpos | 2 | 3 | 0 | 0 | 2 | 4.3 |
| Uterus anomaly | 3 | 4.5 | 0 | 0 | 3 | 6.4 |
| Vaginal anomaly | 1 | 1.5 | 0 | 0 | 1 | 2.1 |
Note: LARA: Low Anorectal Anomaly; HARA: High Anorectal Anomaly.
Table 9: Distribution of urological anomalies in each group.
Anorectal malformations are among the most common surgical neonatal anomalies seen in children. Frequently, patients with ARM are associated with anomalies of other systems of the body, commonly the genitourinary system with an incidence ranging between 25% and 50%. Urological anomalies are the cause of significant morbidity and mortality in ARM patients rather than ARM itself. The present study aimed at identifying and classifying the associated urological anomalies with ARM patients who underwent screening of the genitourinary system.
This study’s population involved a total of 66 patients with ARM, whereby 63.6% of them were male and 36.4% were female, all diagnosed during the neonatal period. Similar to previous studies that reported that ARM is slightly more common among male than female patients with ARM. Moreover, in the present study low and high anorectal anomalies occurred merely frequently in male patients, this could be due to higher prevalence compared to female patients [2,12].
Furthermore, this study showed that more patients had high anorectal anomalies whereby high imperforate anus without fistula was the most prevalent with an incidence of 31.0% among males with ARM, while recto-vestibular fistula anomaly was the most common in female patients with an incidence of 58.3%.
In a study done by Cassina et al., on 428 patients with ARM, the rectovestibular fistula was the most common ARM with 60.3% of incidence among females whereas rectoperineal fistula and rectourethral fistula were common in males with incidence of 40.7% and 38.3% respectively [13]. Similar results were found in other studies reported that rectovestibular fistula and rectoperineal fistula as the most frequent anomalies in female and male patients respectively. In our study, imperforate anus without fistula was the commonest anomaly among male patients in comparison to the studies reported previously, this is due to failure of localization of the fistula on high pressure distal colostogram that was done before definitive repair of ARM [14,15].
In the current study, the overall incidence of urogenital anomalies was 33.3% of all patients with ARM. Comparable results have been published in various articles reporting a high incidence of urogenital abnormalities in ARM patients. A recent study done by Fuchs et al. reported that urological abnormalities were diagnosed in 45% of females and 55% of male patients with ARM. A study done in the Netherlands reported a 57% incidence of genitourinary anomalies in patients with ARM. In both studies the overall incidence of urological anomalies is higher in comparison to our study, this could be attributed by smaller study population and short duration of the present study [16,17].
Of 66 patients, 22.7% patients had abnormal findings on genital examination, whereby hypospadias with or without another genital anomaly was the most frequent genital anomaly with 6 (9.1%) incidence. A slightly higher incidence of hypospadias was reported in a recent study conducted in Italy whereby the incidence was 10% among male patients with ARM. Another study that was conducted on 408 male ARM patients reported even higher incidence of hypospadias of 21% and at least one associated urological defect. This association was also encountered in our study where 2 male patients had absent kidney with hypospadias and undescended testis in each. In our study, bifid scrotum was among the genital anomalies identified with an incidence of 5 (7.6%) among ARM patients. A study that included 909 male patients with ARM reported that bifid scrotum was found in 102 patients, which was higher in comparison to our study which could be due to lager study population. In the current study we found that 7.14% (3 of 42) of male patients had bifid scrotum associated with recto-bladder neck fistula which is a lower incidence when comparing to another study where 26.1% (29 of 111) male patients had recto-bladder neck fistula with associated bifid scrotum [18-20].
The present study reports the incidence of undescended testis of 3.0% among all patient with ARM. In one study conducted in Iran, reported a wide spectrum of urogenital anomalies, whereas undescended testis and hypospadias were the most frequent genital abnormalities detected with an incidence of 37.5% of those with genital anomalies [21].
Moreover, in our study the incidence of Mullerian Duct Anomalies (MDA) associated with ARM in specific cloacal anomalies, were hydrocolpos at 3.0%, uterus anomalies (bicornuate uterus and uterus agenesis) at 4.5% and vaginal agenesis at 3.0%. These anomalies occurred concurrently with urological anomalies such as hydronephrosis, multicystic kidney, and vesicoureteral reflux, ectopic and duplex ureters. A similar relation between cloacal malformations, MDA and urological anomalies has been reported in previous studies. In one large series of 490 cases, found that the incidence of hydrocolpos in patients with cloaca was at 30%, while the incidence of both uterus and vaginal anomalies was at 40%. These anomalies had associated urological anomalies similar to the findings of the present study [22].
In our study, all the patients underwent urological assessment which involved genital examination and renal ultrasound during the neonatal period. In 7 (10.6%) out of 66 patients had abnormal renal ultrasound findings, of whom VCUG was done and 2 patients were diagnosed with bilateral VUR. A study conducted by Ahn et al., that constituted 427 cases of ARM, similar urological screening methodology was done except a renal scan. This study reported that 22% (93 of 247) had a urological assessment that involved renal ultrasound done in 25% (112/427), VCUG in 8% (34/427) and a renal scan in 1% (4/427) [23].
In another study, urological evaluation involved renal ultrasound and VCUG were done in all patients with ARM, whereby VUR was detected in 10 patients who had normal renal ultrasound, which was similar to another study in which VUR was detected in 16 patients where 10 had normal renal ultrasound at birth. In contrast to the present study where VCUG was done only in patients with abnormal renal ultrasound findings, thus lower incidence of patients with VUR [24].
In the present study, VCUG was performed in all patients with abnormal renal ultrasound findings. Absent kidney and VUR were the most common urological anomalies, each with an incidence of 3.0% of all patients with ARM. Other urological anomalies identified in our study were horseshoe kidney, hydronephrosis, multicystic kidney and ureteral anomalies with incidence of 1.5% of all patients. Most of these anomalies occurred concurrently with genital anomalies. Similar urological abnormalities have been identified in previous studies. In a study conducted over 5 years, showed that 25 (64%) patients had urogenital abnormalities, whereby hydronephrosis was 62.5%, VUR 37.5%, unilateral renal agenesis 31.2% and horseshoe kidney 6.2% as the most frequent anomalies. Another study reported that 17 (32%) patients had solitary kidneys out of 53 patients with genitourinary anomalies, while 41 (31%) out of 190 ARM patients had VUR [25,26].
In our study, urogenital anomalies were highly associated with high anorectal anomaly is the risk of associated urological anomalies increases directly with the complexity of ARM. Among 22 patients with urogenital anomalies, 20 patients had associated high anorectal anomalies. Among male patients, urogenital anomalies were found in 3 of 5 with recto-bladder neck fistula, 3 of 15 with high imperforate anus without fistula and 2 of 8 with rectourethral fistula. Among female patients, 4 of 6 with cloacal malformation had urological anomalies.
This finding is paramount and should raise the suspicion of associated urogenital anomalies in all patients with high or complex ARM. Similar results have been reported in one study, where the incidence of urologic abnormalities increased with the severity of the ARM subtype (p<0.0001), with males having bladder neck fistulas and females having cloacal malformations being the most common. In both males and females, as ARM complexity increased, the rate of hydronephrosis and VUR also increased. Also, in other studies reported a high incidence of urological anomalies in patients with complex ARM, more commonly in cloacal malformation and rectourethral fistula in females and males respectively [27].
Moreover, another study reported 45 (42.5%) cases of associated urological defects in 101 patients with ARM, whereby these anomalies were significant in a high variety of ARM when compared to its counterpart [28]. Similar to another report, among 20 patients with urological abnormalities out of 72 ARM patients, 16 patients had a high anorectal anomaly, a significant association [29].
Lastly, a study was conducted to determine risk factors of associated urological anomalies, and found that the presence of high ARM subtype, the presence of genital defect and cloacal malformations in female were significant determinants [30]. Adequate screening and a high index of suspicion of any associated urological anomalies in patients with ARM, especially with high anomaly type is essential to preserve renal structure and function.
Screening of associated urological anomalies is vital to prevent renal damage and reduce morbidity and mortality in patients with anorectal malformations. The most frequent related anomalies in anorectal patients are urological malformations. According to the majority of papers, the incidence ranges from 30% to 50%, and the prevalence of such relations increases in direct proportion to the intricacy of anorectal malformations. Therefore, a high index of suspicion is required to facilitate the early diagnosis and therapy of these anomalies. In order to avoid harm to the urinary system, it is also crucial to monitor kidney function and urinary tract morphology in individuals with anorectal abnormalities over the long term.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Ahmed O, Marco P, Ahmed K, Mohamed A (2024). Screening of Urological Anomalies Associated with Anorectal Malformations in Children: Single-Center Experience in Two Years. Adv Pediatr Res. 11:085.
Received: 16-Aug-2024, Manuscript No. LDAPR-24-34061 ; Editor assigned: 19-Aug-2024, Pre QC No. LDAPR-24-34061 (PQ); Reviewed: 02-Sep-2024, QC No. LDAPR-24-34061 ; Revised: 09-Sep-2024, Manuscript No. LDAPR-24-34061 (R); Published: 17-Sep-2024 , DOI: 10.35248/2385-4529.24.11.085
Copyright: © 2024 Ahmed O, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.