Annals and Essences of Dentistry
Open Access
ISSN: 0975-8798, 0976-156X
ISSN: 0975-8798, 0976-156X
Case Report - (2022)Volume 14, Issue 5
Surgery to remove third molar teeth is one of the most common surgeries in the field of oral surgery. Subcutaneous emphysema is an uncommon clinical complication caused by high-pressure injection of air into loose connective tissue beneath the skin layer, mainly as a result of the use of a high-speed handpiece that fragments the tooth during surgery. Subcutaneous emphysema is observed mainly in the third and fifth decades of life and at the surgical site of mandibular wisdom tooth extraction. Emphysema can spread to deep spaces such as infratemporal, trigomandibular, mestric, lateral or back pharyngeal or mediastinum. In this article, subcutaneous emphysema caused during third molar extraction using an Air-driven handpiece in a 28-year-old woman is presented and investigated. Also, how to manage the patient is described and issues related to the diagnosis and prevention of surgical complications are discussed. Trismus was created with maximum mouth opening of about 30 mm, and no signs of dysphagia or shortness of breath were reported. The patient was prescribed four million units of penicillin (every four hours), metronidazole 500 mg (once every eight hours which was dissolved in 100 cc of normal saline solution and injected slowly intravenously) and mouthwash (every eight hours with chlorhexidine 02.2 percent) was hospitalized. The patient in question was hospitalized for 36 hours under antibiotic regimen and then followed up until the fifth day and until the complete resolution of the swelling and the maximum opening of the mouth up to 50 mm and the absence of crepitation. No other local, systemic or infectious complications occurred.
Subcutaneous emphysema; Molar; Mandible; Infratemporal
Surgical removal of third molar teeth is one of the most common surgical procedures in the field of oral surgery [1], but despite the skill and experience of the surgeon, complications may occur [2]. Subcutaneous emphysema is an uncommon clinical complication caused by high-pressure injection of air into loose connective tissue under the skin layer, mainly as a result of the use of a high-speed hand piece that fragments the tooth during surgery [3]. When air enters the subcutaneous layer, it can remain localized at the surgical site or spread along the loose connective tissue plane. Its common symptoms are trismus, dysphagia, swelling, cryptos and sensitivity to touch while touching the area, edema, erythema, pain and possible airway obstruction. Swelling can begin immediately after surgery or with a slight delay after about four hours [4].
The patient was a 28-year-old woman who was referred to Kashani Hospital in Isfahan by a private dentist for surgery on the right third molar of the mandible, which was lying in the mandible, in a horizontal position and near the mandibular canal. The patient who complained of swelling and pain on the right side of his face admitted that the swelling occurred almost immediately during surgery. There was no specific and relevant case in the medical records and systemic conditions of the patient, and routine tests before surgery, including coagulation tests, were within normal limits.
Clinical examination revealed crepitation and sensitivity to touch on the right side of the face, the right carotid triangle that extended to the right clavicle. Trismus was created with the maximum opening of the mouth at about 30 mm in Figures 1-3 and no signs of dysphagia and shortness of breath were reported. The patient had no history of systemic diseases. Also, there was no history of allergic reaction to food, medicine or any severe seasonal sensitivity in the patient's history. The patient's blood pressure was 125/65, heart rate was 73 and body temperature was 33.7°C. The percentage of arterial oxygen saturation was reported as 94%.
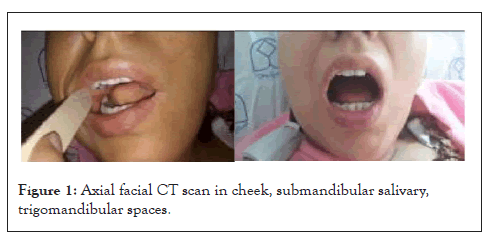
Figure 1: Axial facial CT scan in cheek, submandibular salivary, trigomandibular spaces.
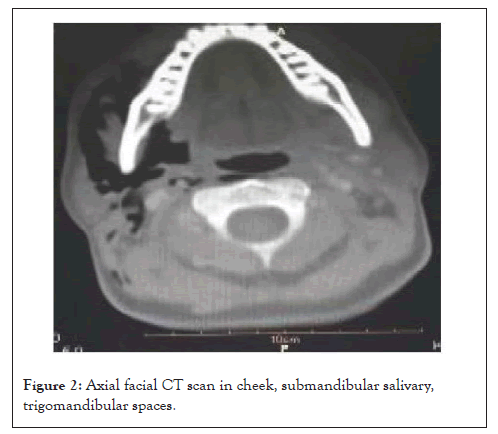
Figure 2: Axial facial CT scan in cheek, submandibular salivary, trigomandibular spaces.
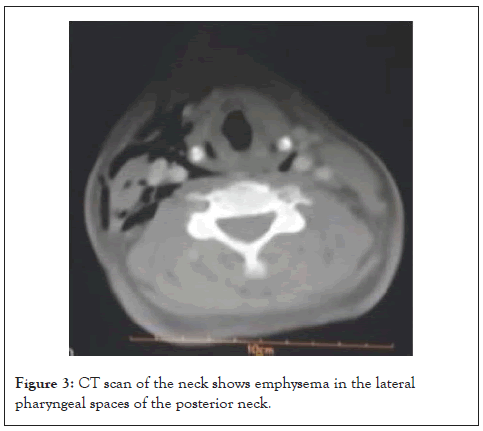
Figure 3: CT scan of the neck shows emphysema in the lateral pharyngeal spaces of the posterior neck.
The patient was prescribed four million units of penicillin (every four hours), metronidazole 500 mg (every eight hours dissolved in 100 cc of normal saline solution and injected slowly intravenously) and mouthwash (every eight hours with chlorhexidine 0.2 percent) was hospitalized.
Then, CTscan with head and neck and chest contrast was performed. In the CT performed, emphysema had penetrated to the right subcutaneous, lower eyelid, buccal, submandibular salivary gland space, back neck space around the carotid sheath, chest wall and mediastinum (Figures 4 and 5). The patient was observed for 36 hours in the hospital without any respiratory distress or pain, and following the reduction of swelling, the maximum opening of the mouth was possible more than 30 mm.
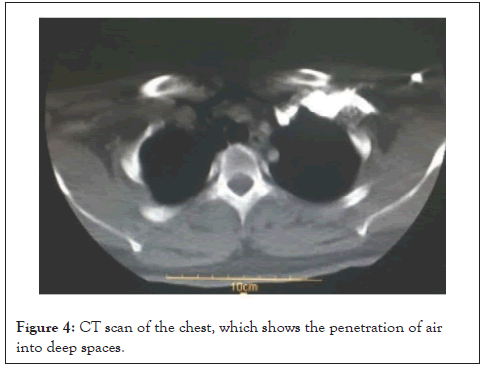
Figure 4: CT scan of the chest, which shows the penetration of air into deep spaces.
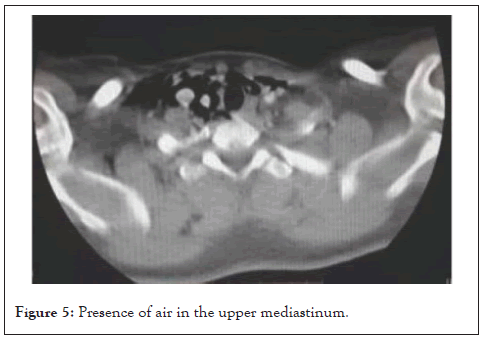
Figure 5: Presence of air in the upper mediastinum.
Subcutaneous emphysema and pneumomediastinum are complications not limited to dental procedures and may be caused by trauma, soft tissue infection, iatrogenic injury following neck surgeries such as tracheostomy and chest tube placement [5,6]. In order to implement a correct treatment, it is important to differentiate the diagnosis from complications that also involve soft tissue swelling, such as hematoma, allergic reaction, or angioedema [7]. A complete history of the current illness and a thorough clinical examination are essential for a correct diagnosis [8]. This clinical examination is based on crepitation on palpation, sudden onset of swelling associated with tenderness without erythema, fever, or lymphadenopathy [9].
Subcutaneous emphysema is observed mainly in the third and fifth decades of life and at the surgical site of mandibular wisdom tooth extraction. Emphysema can spread to deep spaces such as infratemporal, trigomandibular, mestric, lateral or back pharyngeal or mediastinum [6]. Differential diagnoses in this case can include allergic reaction to drugs, hematoma, angioedema, and infection [4,9,10].
Subcutaneous emphysema is a rare complication in the oral and dental field, but if it occurs, it is mainly associated with mandibular molar teeth surgery by air-driven handpieces [11,12]. A review of research articles in which 32 cases of subcutaneous emphysema were investigated showed that half of the cases were related to the use of Air-driven handpieces [12].
Large flaps, especially during third molar surgery, can increase the risk of emphysema, air may infiltrate into the pterygomaxillary region and into the lateral pharyngeal space from the retromolar molar region and extend into the mediastinum by discecting the visceral space. It is also possible that the air penetrates into the cervical plates and expands to the mediastinum, causing more fatal consequences [13]. The presence of pain in both chest and back areas can suggest the presence of mediastinal emphysema. Chest X-ray is necessary to confirm this diagnosis [14]. Crepitation is a pathognomic sign that can help distinguish emphysema from angioedema [8].
Subcutaneous emphysema is resolved in most cases without any need for intervention and the required attention is limited to symptom control [15]. Airway patency should be considered; however, the treatment of emphysema depends on the type of spaces involved. The connection between the deep space of the head and neck can result in the expansion of large amounts of air in deeper spaces [3]. The retrolaryngeal space, also called the danger space, has the potential to transmit air to the dorsal mediastinum. Involvement of the lateral and retrolaryngeal spaces may block the airway; therefore, careful monitoring of them is necessary. It has also been reported in some cases that the orbital space is pressurized by air, followed by damage to the optic nerve [4].
In oral dental treatments, depending on its origin, emphysema can transfer microorganisms from microflora or necrotic pulp to soft tissue and increase the risk of secondary infection. Infection is usually not seen in a subcutaneous emphysema, but cases have been reported where this condition has occurred. Prophylactic antibiotic treatment is recommended, because the injection of non-sterile air and water can cause serious complications for the patient's health. The described patient was treated with a drug regimen including antibiotics [5,9,12].
In most cases, subcutaneous emphysema starts after 3 to 5 days, and is completely managed after 7 to 10 days [12]. It is important to advise patients to avoid increasing the pressure inside the mouth, for example through strong fanning or playing wind instruments; because these processes can cause more air to enter [16]. The patient was hospitalized for 36 hours and then was observed until the fifth day and until the complete resolution of symptoms and signs.
Due to the feeling of pain in emphysema sufferers, supportive analgesic treatments are considered. Corticosteroids such as prednisolone or dexamethasone are prescribed to reduce the inflammation and swelling following emphysema, and keeping the patient's airway open helps [4].
Surgery is not the only risky intervention for the development of subcutaneous emphysema, and cases of its occurrence during restorative operations, veneer preparation, and denervation have been mentioned [12]. There are also reports based on the development of emphysema following oral laser surgery procedures [15]. Air can enter the soft tissue through several routes, but most commonly it passes through the dentoalveolar membrane or the root canal. Emphysema with secondary infection following the use of compressed air during pulp therapy has been reported [5].
Emphysema can be prevented by following standard surgical guidelines. The increase in the height of the periosteal mucosal flap should be minimal and should not extend to the lingual alveolus of the mandibular third molar. Muscular connections should be preserved as much as possible. Slow and careful pushing aside as well as limited expansion of periosteal mucosal flaps can prevent air penetration into deep butts. Also, the duration of use of highspeed air-driven handpieces should not be longer than necessary, or even they should be replaced with a contra-angle multiplier (1:5) handpiece, which does not use high-speed air flow for movement. However, immediate diagnosis Emphysema is very important to avoid serious complications such as mediastinitis.
This article is not sponsored.
According to the authors, this article has no conflict of interest.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Bargahi E (2022) Subcutaneous Emphysema Development Following Molar Surgery. Ann Essence Dent. 14:234.
Received: 03-Oct-2022, Manuscript No. AEDJ-22-19643; Editor assigned: 05-Oct-2022, Pre QC No. AEDJ-22-19643 (PQ); Reviewed: 19-Oct-2022, QC No. AEDJ-22-19643; Revised: 26-Oct-2022, Manuscript No. AEDJ-22-19643 (R); Published: 04-Nov-2022 , DOI: 10.35248/0976-156X.22.14.234
Copyright: © 2022 Bargahi E. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.