
Advances in Pediatric Research
Open Access
ISSN: 2385-4529

ISSN: 2385-4529
Research Article - (2023)Volume 10, Issue 4
Background: Globally, it has been known that around 15.5% of infants were below the normal level of weight at their birth and 95% of these infants lived in developing countries.
Objectives: The study aimed to model time to normal weight from low weight among low weight infants delivered at Jimma University Medical Center (JUMC).
Methods: The retrospective data from all the admitted follow up of Low Birth Weight (LBW) infants, from September 1,2020 to March 30,2022 in JUMC is used in this study. By assessing the overall goodness of fitted models, log- logistic accelerated failure time model which can fit the data well and had smallest akaike information criterion value was selected as the appropriate fit model.
Results: Out of 325 LBW infants 286 (88%) were recovered from LBW and 39 (12%) censored. The most important predictors of time to normal weight at 0.05 level of significance were place of residence [ φ =0.877 (95% CI: 0.808- 0.952)], multiple birth [ φ =1.459 (95% CI: 1.316-1.617)], gender [ φ =0.870 (95% CI: 0.809-0.936)], history of abortion [ φ =1.296 (95% CI: 1.165-1.441)], preterm birth [ φ =1.172 (95% CI: 1.070-1.285)], maternal age 20-34 [ φ =0.813 (95% CI: 0.727-0.909)] and maternal age >34 [ φ =0.798 (95% CI: 0.694-0.917)], ANC follow up [ φ =0.816 (95% CI: 0.755-0.883)] and weight at birth 1000-1500 gm [ φ =0.773 (95% CI: 0.658-0.910)] and weight at birth 1500-2500 gm [ φ =0.700 (95% CI: 0.602-0.815)].
Conclusion: Log-logistic AFT model fits the data well in analyzing time to normal weight among LBW infants data. The duration of time to normal weight of LBW infants significantly affected by the infants’ place of residence, birth status, history of abortion of mothers, gender, preterm, maternal age, number of ANC visits and weight at birth. Therefore, special emphasis should be given for infants who are female, rural place of residence, multiple birth, prematurely birth, infants born from teenage mothers, mother have an abortion, mother have not regular ANC follow up and infants who had <1000 gm birth weight to improve the duration of LBW. The estimated median duration of LBW was 10 days.
Low birth weight; Infant; Survival model; Normal weight
AFT: Acceleration Failure Time; AIC: Akiake Information Criteria; ANC: Antenatal Care; BMI: Body Mass Index; CI: Confident Interval; JUMC: Jimma University Medical Centre; LBW: Low Birth Weight; MLE: Maximum Likelihood Estimation; MUAC: Mid Upper Arm Circumference; NBW: Normal Birth Weight; NDHS: Nigeria Demographic Health Survey; PAF: Population Attribute Fraction; PH: Proportional Hazard; PL: Partial Likelihood; WHO: World Health Organization
Low Birth Weight (LBW) is defined as weight of child at birth less than 2500 g measured within 24 hours of birth (WHO). Level of low birth weight is categorized in to three based on weight. Low birth weight is defined as less than 2500 grams, very low birth weight is less than 1500 g and extremely low birth weight is less than 1000 g [1]. This practical cut-off for international comparison is based on epidemiological observations that infants weighing less than 2,500 grams are approximately 20 times more likely to die than heavier babies [2]. More common in developing than developed countries, a birth weight below 2,500 grams contributes to a range of poor health outcomes [3]. Normal weight at term delivery is 2,500-4,000 g.
Preterm birth (younger than 37 weeks of gestation), smaller gestational age (a slow prenatal growth rate) and a combination of preterm birth and smaller gestational age are the common cause of low birth weight. Risk factors in the mother may contribute to low birth weight. Those factors are young ages, multiple pregnancies, previous LBW infants, poor nutrition, heart disease or hypertension, untreated coeliac disease, drug addiction, alcohol abuse and insufficient prenatal care. In addition, pre-labor rupture of membranes and environmental risk factors such as smoking, lead exposure and other types of air pollutions are also the cause of low birth weight [4-7]. In general, the risk of neonatal mortality for very LBW infants is 25 to 30 times greater than for infants with a birth weight exceeding 2500 g [8].
The incidence of LBW is estimated to be 16% worldwide, 9% in the least developed and developing countries and 7% in the developed countries. Globally, more than 20 million infants are born with LBW. The largest number of LBW babies is concentrated in two regions of the developing world which are Asia and Africa. Seventy-two percent of LBW infants in developing countries are born in Asia, specifically, in South Asia that accounts for half of the LBW and 22% are born in Africa. The prevalence of LBW in sub-Saharan Africa ranges between 13% and 15%, with little variation across the region as a whole. In East Africa the prevalence of LBW is 13.5% and in Ethiopia between 2006 and 2010, United Nations Children's Fund (UNICEF) estimated the prevalence of LBW to be 8% [3].
LBW is one of the critical issues in Ethiopia that causes many babies short-term and long term health consequences and tend to have higher mortality and morbidity. Ethiopia Demographic and Health Survey (EDHS) Ethiopia/2005 report shows that the percentage of LBW babies has increased in the past five years from 8 percent in 2000 to 14 percent in 2005. LBW is a reasonable well-defined problem caused by factors that are potentially modifiable and the costs of preventing them are well within rich, even in poor countries like Ethiopia. Furthermore, the study conducted in Jimma University Medical Center (JUMC) indicated that the prevalence of low birth weight was 7.8%, with regard to factor associated with birth weight, antenatal care follows up, parity, gestational age, sex of new born and maternal age during the last pregnancy had significant association with LBW [8]. The study conducted at Butajira general hospital, Southwest Ethiopia, showed that the magnitude of low birth weight among study participants was 12.5% and factors such as maternal medical complication during pregnancy, maternal MUAC less than 23 cm and birth interval less than 24 months were significantly associated with low birth [9]. Some of the studies conducted so far used logistic framework. However, for time-to-event data, survival analysis method is more powerful than the logistic framework as it takes censoring into consideration. Most importantly, the absence of studies conducted to model time to normal weight from low birth weight by using survival analysis on the basis of determining most significant factors affecting the length of life time of LBW of infants under follow-up especially in the study area motivated this study. Therefore, to fill this gap and all the stated above, this study will identify a risk factor that brings low birth weight at Jimma University Medical center.
The study area, design and target population
The study is conducted at JUMC. Jimma University Medical center is one of the oldest public hospitals in Ethiopia. The hospital is located in Jimma city and, Jimma is the largest city in South-western of Oromia region at a distance of 355.2 Km from Addis Ababa, the capital city of Ethiopia. This time the hospital provides services for more than 20 million patients with 800 bedded. The study is a retrospective cohort type because, it investigates time to normal weight of low birth weight infants, since September 1, 2020 to March 30,2022. The study population included selected infants with low birth weight, that have been followed time between September 1, 2020 to March 30,2022 would be included.
Inclusive and exclusive criteria
All infants who born with low weight (<2,500 g) during the study period would be included in the study. While, infants who born with more than or equal to 2,500 g during the study period would be excluded.
Variables in the study
To response variable in this study is the time to normal weight of LBW infants from infants starts to follow-up for treatment. The entry of the survival data would be considered from the day that the infants follow up for treatment. The event is occurred when the infant develops normal weight. Among the infants there are children that are transferred to other hospital, dropped treatment, died, does not develop normal weight at March 30, 2022 (at the end of study time). This means that the type of the survival data is random right censored.
Residence, multiple birth, history of abortion, gender, preterm, birth status, gravidity, parity, maternal age, number of ANC visits, birth weight were all considered independent variables in this study.
Statistical models
Survival model is statistical model used for analysis of data which have survival time, censored observation and explanatory variables whose effect on the waiting time we wish to assess or control. Survival time is the waiting time until the occurrence of a well-defined event.
The Kaplan-Meier is also known as the product-limit method and in the presence of censored cases, it is used for estimating timeto- normal weight in our context. It is a descriptive procedure for examining the distribution of time-to-event variables.
The log-rank test, first proposed by Breslow, allows for comparison of the survival curves for two or more groups [10]. It gives information on the significance of the difference in the survival of two groups of participants. You can think of it as a one-way Analysis of Variance (ANOVA) for survival analysis.
Checking proportional hazard assumption
It is obvious to check PH assumptions before conducting further survival analysis. Here the assumption of PH was checked by the GLOBAL Schoenfeld test. The null hypothesis of the PH assumption holds rejected for small p-values [11].
Accelerated failure time model
A parametric survival model is one in which survival time is assumed to follow a known distribution. Under parametric survival models, these study was considered with exponential, Weibull, log normal and log-logistic regression models. The Accelerated Failure Time model (AFT) is one of parametric survival models that can be used as an alternative to PH model, especially to overcome the statistical problems due to the violation of PH assumption [12]. The parametric accelerated failure time models can be represented in the form
where βt = ( β1, βp ) is a vector of regression coefficients and n∈N and  Xis accelerated factor ( φ ) which accelerates the survival
function with covariate X =0 [13].
Xis accelerated factor ( φ ) which accelerates the survival
function with covariate X =0 [13].
Comparison of models
This study makes a comparison between survival models. This is directly possible for parametric models. This study use Akaike Information Criterion (AIC) for model comparison among all parametric models. Additionally, in existence of nested models, likelihood ratio test is applying to select the best model. AIC is an estimator of out-of-sample prediction error and thereby relative quality of statistical models for given set of data. Given a collection of models for the data, AIC estimates the quality of each model, relative to other models and it estimates relative amount of information lost by a given model: the less information a model loss, the higher the quality of that model. It is given by:
AIC = -2 log(likelihood) + (pk)
where p denotes number of independent variables in the model and k is some constant, k=1 for the exponential model and k=2 for the Weibull, log-logistic and log-normal models [13].
Model diagnostics checking
The Cox-Snell residual plot was done to determine whether the AFT model is well fitted. Residual plots can also be used in the graphical assessment of the adequacy of a fitted model. Thus, the plot of the estimated hazard rate of the Cox-Snell residuals should give a straight line with unit slope and zero intercept if the fitted model is good [13].
Ethical issues
The ethical clearance and permission were obtained from the Research Ethical Review Board of the College of Natural Sciences, Jimma university before starting data collection. An ethical clearance letter from Jimma university was given to the manager of the JUMC and a permission letter was obtained. The research was collected: (1) Respondent history from records (hard/electronic sources) only by a trained health professional assigned by the concerned institute; (2) All data collected was treated with maximum confidentiality; the identity of the respondents was never exposed to anyone at any time by any means; (3) The information/data was never used for any other purpose than for the scientific goal and was never transferred to any third party with the identity of the respondents.
Descriptive statistics
A total of 325 infants were included in this study. There were 166 (51.08%) female and 159 (48.92%) male infants in the study. The minimum and maximum birth weights were 970 g and 2490 g respectively. We observed 286 (88%) events recovered from low weight and 39 (12%) censored observations. The result of birth place showed that 172 (52.92%) were born in urban and 141 (81.98%) of them have develop normal weight, were 153 (47.08%) born in rural from which 145 (94.77%) were develop normal weight. The infants birth status showed that a total of 228 (70.15%) infants were singleton birth and 195 (85.53%) of them have develop normal birth weight and 97 (29.85%) were multiple birth. The infants preterm birth showed that a total of 237 (72.92%) infants were normal birth, from those 204 (86.08%) of them have develop normal birth weight and 88 (27.08%) were prematurely birth. Likewise, the infants weight at birth showed that a total of 255 (78.46%) infants were born with low birth weight (1500-2500), from those 246 (96.47%) of them have develop normal birth weight and 70 (21.54%) infants were born with very low birth weight (<1500) (Table 1).
| Variables | Categories | Number of infants | Events (%) | Median (days) | 95% CI |
|---|---|---|---|---|---|
| Residence | Rural | 153 | 145 (94.77) | 16 | (14,17) |
| Urban | 172 | 141 (81.98) | 8 | (7,8) | |
| Birth status | Single | 228 | 195 (85.53) | 8 | (8,9) |
| Multiple | 97 | 91 (93.81) | 22 | (20,25) | |
| Abortion | No | 269 | 233 (86.62) | 9 | (9,10) |
| Yes | 56 | 53 (94.64) | 27 | (25,31) | |
| Gender | Female | 166 | 154 (92.77) | 15 | (13,17) |
| Male | 159 | 132 (83.02) | 8 | (8,9) | |
| Preterm | Normal | 237 | 204 (86.08) | 9 | (8,9) |
| Prematurely | 88 | 82 (93.18) | 22 | (20,26) | |
| Gravidity | 1 | 103 | 89 (86.41) | 11 | (10,13) |
| 2-4 | 172 | 155 (90.12) | 10 | (9, 12) | |
| >4 | 50 | 42 (84.00) | 11 | (9,16) | |
| Parity | 1 | 125 | 113 (90.40) | 10 | (9,12) |
| 2-4 | 154 | 137 (88.96) | 10 | (10,13) | |
| >4 | 46 | 36 (78.26) | 10 | (9,16) | |
| Maternal age | <20 | 32 | 29 (90.63) | 27 | (26,35) |
| 20-34 | 254 | 224 (88.20) | 10 | (10,12) | |
| >34 | 39 | 33 (84.62) | 8 | (7,10) | |
| Antenatal care | No | 145 | 132 (91.03) | 16 | (15,19) |
| Yes | 180 | 154 (85.56) | 8 | (8,8) | |
| Birth weight | VLBW | 70 | 40 (57.14) | 20 | (16,25) |
| LBW | 255 | 246 (96.47) | 10 | (9,11) |
Note: CI: Confident Interval; VLBW: Very Low Birth Weight; LBW: Low Birth Weight.
Table 1: Frequencies and percentages of categorical covariates of LBW infants who were enrolled in JUMC.
Out of those mother who gave birth of <2500 g newborn, majority, 254 (78.15%) of them were aged between 20-34 years. From those mothers, majority, 172 (59.92%) of them had 2-4 gravidity. From those mothers, majority, 154 (47.38%) of them had 2-4 parity, followed by mothers those had only 1 parity (primapara), 125 (38.46%). Regarding ANC visits of mothers during pregnancy, 145 (44.62%) of them had not had ANC visits regularly, while 180 (55.38%) had had ANC visits regularly in their recent pregnancy. In the case of history of abortion, out of total mothers, 269 (82.77%) had never had an abortion before.
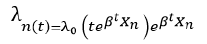
Kaplan Meier survival curve estimates
From Figure 1 we observe that, the line for birth place (rural), birth status (multiple), history of abortion (yes), gender (female), preterm (prematurely), gravidity (2-4), parity (2-4), maternal age (<20), ANC visits (no) and birth weight (EVLBW (<1000 gm)) lies above their respective (belonging) categories, which indicates that they are prolonged longer to develop normal weights from low birth weights.
Figure 1: Kaplan-Meier survival plots of some selected categories of predictor variables. 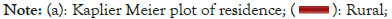




Based on the result of log rank test, we found that except for the categories of graviditiy and parity, there were significant differences in survival probability to recovery of patients in different categories of residence, birth status, history of abortion, gender, preterm birth status, maternal age, ANC visits and weight at birth at 5% level of significance (Table 2).
| Variables | Chi square | DF | P-value |
|---|---|---|---|
| Residence | 80.5 | 1 | <0.001 |
| Birth status | 210 | 1 | <0.001 |
| Abortion | 112 | 1 | <0.001 |
| Gender | 81.4 | 1 | <0.001 |
| Preterm | 127 | 1 | <0.001 |
| Gravidity | 1.2 | 2 | 0.6 |
| Parity | 0.3 | 2 | 0.9 |
| Maternal age | 60.2 | 2 | <0.001 |
| Antenatal care | 114 | 1 | <0.001 |
| Birth weight | 18.3 | 1 | <0.001 |
Note: DF: Degrees of freedom.
Table 2: The result of log rank test for categorical variables.
Evaluation proportionality hazard assumption
The proportional hazards assumption, which asserts that the hazard ratios are constant overtime and it is important to use fitted proportional hazards model. From Table 3, we observe that the goodness of fit test gives a significant global p-value and the global null hypothesis that the proportionality assumption holds is rejected, the PH model is inappropriate in this case. As a result, the AFT model was used to analyze the survival time to normal weight of LBW infants.
| Variables | Chi square | DF | P-value | Does PH assumption hold? |
|---|---|---|---|---|
| Residence | 33.07 | 1 | <0.001 | No |
| Birth status | 19.97 | 1 | <0.001 | No |
| Abortion | 1.22 | 1 | 0.27 | Yes |
| Gender | 16.92 | 1 | <0.001 | No |
| Preterm | 1.04 | 1 | 0.309 | Yes |
| Maternal age | 4.02 | 2 | 0.134 | Yes |
| Antenatal care | 6.14 | 1 | 0.013 | No |
| Birth weight | 6.72 | 1 | 0.001 | No |
| Global | 54.55 | 9 | <0.001 | No |
Note: PH: Proportional Hazard; DF: Degrees of Freedom.
Table 3: Global test for proportional hazards assumption.
Acceleration failure time model fitting
In the univariable AFT model analysis, all the covariates are statistically significantly associated with time to normal weight of LBW infants except gravidity and parity which were insignificant at a 25% level of significance. The covariates that were found to be significant in the univariable analysis were included in the multivariable analysis. The multivariable survival analysis in the study was done by considering the exponential, Weibull and loglogistic distributions for the baseline hazard function.
AFT parametric models
Parametric models such as exponential, Weibull, log-logistic and log-normal models were carried out to identify a model that fits the data better. The summary of log-likelihood and AIC is presented in Table 4. The rule is that any model that conforms to the observed data should adequately lead to a smaller AIC. Hence, the log-logistic model appears to be with minimum AIC and Bayesian Information Criterion (BIC) values among all other competing parametric models, revealing that it is the most efficient model to identify the predictors of the waiting time to normal weight of LBW infants.
| Model | AIC | BIC | -2LL |
|---|---|---|---|
| Exponential | 2029.806 | 2067.644 | 2009.8 |
| Weibull | 1520.766 | 1562.388 | 1498.8 |
| Log logistic | 1515.954 | 1557.576 | 1494 |
| Log normal | 1549.838 | 1591.46 | 1527.8 |
Note: AIC: Akiake Information Criteria; BIC: Bayesian Information Criterion.
Table 4: Model comparison to identify the predictors of the waiting time to normal weight of LBW infants.
The result for log-logistic, which is a relatively efficient model, is presented in Table 5, with the estimated values of the coefficients, acceleration factor ( φ ) and its 95% CI. Although the proportional hazard assumption was violated. Nevertheless; residence, birth status, history of abortion, gender of infants, status of preterm, maternal age, ANC follow up and birth weight had a statistically significant association with the waiting time for the normal weight of LBW infants based on the log-logistic model at 5% level of significance.
| Variables | Categories | Coefficient (β) | Se (β) | φ (95% CI) | P-value |
|---|---|---|---|---|---|
| Residence | Intercept | 2.701 | 0.085 | 14.865 (12.606,17.601)* | 0 |
| Rural | Reference | ||||
| Urban | -0.125 | 0.045 | 0.882 (0.808,0.965)* | 0.006 | |
| Birth status | Single | Reference | |||
| Multiple | 0.388 | 0.056 | 1.474 (1.321,1.646)* | 0 | |
| Abortion | No | Reference | |||
| Yes | 0.337 | 0.055 | 1.401 (1.257,1.562)* | 0 | |
| Gender | Female | Reference | |||
| Male | -0.124 | 0.038 | 0.883 (0.820,0.951)* | 0.001 | |
| Preterm | Normal | Reference | |||
| Prematurely | 0.163 | 0.049 | 1.177 (1.069,1.295)* | 0.001 | |
| Maternal age | <20 | Reference | |||
| 20-34 | -0.196 | 0.059 | 0.822 (0.732,0.923)* | 0.001 | |
| >34 | -0.238 | 0.075 | 0.788 (0.681,0.912)* | 0.001 | |
| Antenatal care | No | Reference | |||
| yes | -0.208 | 0.044 | 0.812 (0.745,0.885)* | 0 | |
| Birth weight | VLBW | Reference | |||
| LBW | -0.093 | 0.045 | 0.911 (0.835,0.995)* | 0.038 |
Note: (*): p-value <0.05; VLBW: Very Low Birth Weight; LBW: Low Birth Weight; (φ): Acceleration factor; CI: Confidence Interval.
Table 5: Multivariable analysis using the log-logistic parametric survival model.
Accordingly, the estimated coefficient of urban status residence is -0.131, which suggests that infants those born in urban decrease the duration of developing normal weight from LBW approximately by 12 percent ( φ =0.877, 95% CI: (0.808, 0.952)) compared to those born in rural. The estimated coefficient of multiple birth status is 0.378, which suggests the multiple birth increase the duration of developing normal weight among LBW infants approximately 1.46 times higher than singleton birth (( φ =1.459), 95% CI: (1.316, 1.617)). The estimated coefficient of male infant is -0.139, which suggests that male born infants decrease the duration of developing normal weight by 13 percent ( φ =0.870, 95% CI: (0.809, 0.936) compared to those female infants. The estimated coefficient of prematurely preterm birth status is 0.159, which suggests the prematurely birth status increase the duration of developing normal birth weight of infants approximately 1.17 times higher than normal status of preterm ( φ =1.172), 95% CI: (1.070, 1.285). Likewise, the estimated coefficient of low birth weight for weight at birth 1000- 1500 gm and 1500-2500 gm are -0.257 and -0.356 respectively, which suggests that very low birth weight (1000- 1500 gm) and low birth weight (1500-2500 gm) categories of infants birth weight decrease the duration of developing normal weight of infants approximately by 23 and 30 percent ( φ =0.773), 95% CI: (0.658, 0.910) and ( φ =0.700), 95% CI: (0.602, 0.815) compared to those infants weight birth is extremely very low birth weight (<1000 gm).
Considering to maternal case the estimated coefficient of infants born from mothers those had abortion is 0.259, which suggests that infants born from mothers those had abortion increase the duration of developing normal weight for LBW infants approximately by 1.30 times higher than infants born form mothers those had not abortion (φ =1.296), 95% CI: (1.165, 1.441). The estimated coefficient of 20-34 and >34 categories of maternal age is -0.207 and -0.226, which suggests that 20-34 and >34 categories of age mothers of infants decrease the duration of developing LBW to normal weight approximately by 19 and 20 percent ( φ =0.813, 95% CI: (0.727, 0.909) and (φ=0.798), 95% CI: (0.694, 0.917) compared to those <20 aged mothers of infants. Moreover, the infant’s mothers who have regular ANC follow up shorten the duration of developing LBW to normal weight approximately by 18 percent ( φ =0.816, 95% CI: (0.755, 0.883) compared to infant’s mothers who have no regular ANC follow up.
Model diagnosis
Cox-Snell residuals plots rejects a choice of exponential, Weibull and log-normal models, compared to log-logistic model (Figure 2). The line made by Cox-Snell residuals of log-logistic model is reasonably straight and has approximately unit slope and zero intercept. This indicates that log-logistic model is adequate, efficient and appropriate model for analyzing normal weight among LBW infants’ data at JUMC.
Figure 2: Cox-Snell residuals for exponential, Weibull, log-logistic and log-normal models.
The quantile-quantile plot was made for assessing the validity of log-logistic accelerated failure time model using two different groups of participants. The plot, appear to be nearly linear for all covariates. This suggested that the acceleration failure time model would be appropriate for the data (Figure 3).
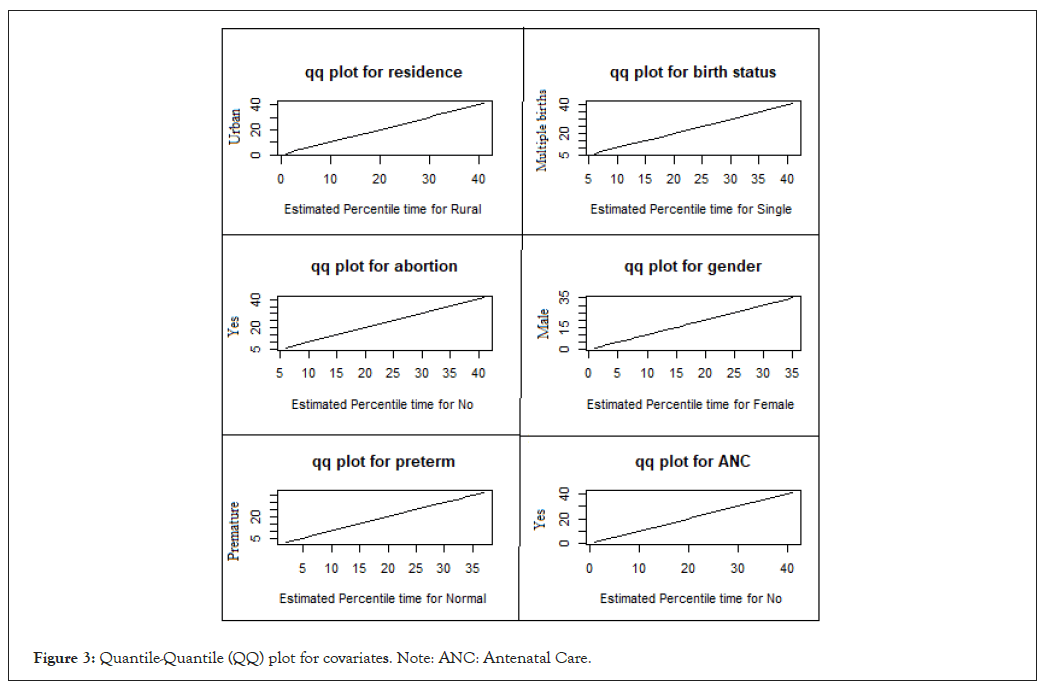
Figure 3: Quantile-Quantile (QQ) plot for covariates. Note: ANC: Antenatal Care.
The despite all the advantages of the Cox model in terms of modeling time-to-event data such as waiting time to normal weight for LBW infants, it has drawbacks when the proportional hazard assumption is violated. When the assumption of proportional hazard was violated, fully, parametric AFT models can be used as an alternative to model time-to-event data such as time to normal weight for LBW infants. In this study, AFT model was employed to analyze time to normal weight among LBW infant data. Among the parametric AFT models, the log-logistic parametric model fitted the data well. The median time to normal weight of the LBW infants was 10 days. The study revealed that males had shorter time to develop normal weight than that of females. This finding is similar to the studies conducted in Nigeria by Olowonyo [13]. The urban place residence is another risk factor for time to normal weight of the LBW infants according to the findings of this study. Urban place of residence had shorter duration of LBW infants compared to rural place of residence. This is similar with the studies of Olowonyo [14]. Regarding preterm birth, results showed that infants born prematurely increase the duration of developing normal weight from LBW infant approximately by 18 percent ( φ =1.177) compared to infants those born in normal gestational age. This is similar with the study found by Seid, Olowonyo and Tema [8,14,15].
Likewise, weight at birth results showed that infants born with very low birth weight (1000-1500 gm) and low birth weight (1500-2500 gm) decrease the duration of developing normal weight from LBW infant compared to those infants born with extremely very low birth weight (<1000 gm). This was in line with a study conducted in southern Ethiopia by Woelile [16]. Neonates with birth weights of less than 1000 gm were threepoint six times the hazard of death compared with neonates with birth weights of 1500-2500 gm.
Considering maternal case the results of history of abortion showed that infants born from those mothers having an abortion history’s increase the duration of LBW approximately 1.30 higher than infant’s mothers those have no an abortion ( φ =1.296, 95% CI: (1.165, 1.441)).
In addition, results showed that multiple birth infant had increase the duration of LBW approximately 1.46 higher than singleton birth infants ( φ =1.459, 95% CI: (1.316, 1.617)). This was supported by studies conducted in Nigeria and Ethiopia Ipadeola, Tema, which state that, multiple births are significantly associated with low birth weight compared with singleton births (Odds Ratio (OR)=0.59, p<0.001) [14,15].
Also, the result of our study revealed that, infants who born from those mothers aged 20-34 and >34 categories decrease the duration of developing LBW to normal weight from LBW approximately by 19 and 20 percent ( φ =0.813) and ( φ =0.798) compared to those <20 aged mothers of infants. This is in line with the study of Khatunand and Ipadeola, that revealed teenage mothers were more likely to give birth to children with low birth weight [14,17]. Here, positive significant association was observed for mothers’ age at birth and child’s weight at birth. Children from mothers in the age range 25 to 39 years were about 1.26 times more likely to weigh more at birth compared with children from teenage mothers (p<0.05).
Furthermore, infant who born from mothers those had regular ANC follow up decrease the duration of LBW approximately by 18 percent ( φ =0.816) compared to those infants born from mothers those had no regular ANC follow up. This is similar with the study that found by Siza and Khatun, which found that there was statistically significant difference between the proportions of LBW infants from mothers who did not receive antenatal care (28.6%) and those who attended for the services (13.8%) ( χ² =8.8; P=0.01) [17,18].
This study had some limitation. Because of the retrospective nature of the study, lack of full records on some factors like mother education level, nutrition of mother, medical complication during pregnancy, HIV status of mother and lack of information on some common drugs taken to LBW infants.
In this study, the log-logistic parametric model has the smallest possible AIC and could be taken as the best fitted model for the data well as compared to other parametric models. Based on the log-logistic model, among the factors of time to normal weight for LBW infants, urban as place of residence, singleton birth, male as gender, very low birth weight of birth weights, infants born with normal gestational age, infant’s mother those who have no abortion, infant’s mothers those have regular ANC follow up and infant’s mother those highly aged were reduce duration to develop normal weight from LBW. The median time to normal weight of the LBW infants was 10 days.
Ethical approval for this study was received from Jimma university, college of Natural and Computational Sciences Research and Ethics Review Board (Ref. No: RPG/331/2022). The author requested to collect data from Jimma University Medical center and granted permission to collect data from patients’ cards. Informed consent to use the data for doing this research was obtained from Jimma University Medical center because the study was retrospective. All procedures performed were in accordance with the Helsinki Declaration. Confidentiality of data was kept at all levels of the study and the data was not used for other purposes other than for this study.
All the authors have read and approved the overall work of this manuscript.
Data will be available upon reasonable request from the corresponding author.
The author(s) declared no potential conflicts of interest exist.
There was no funding for this study.
FT and FL conceived and designed the study, analyzed and interpreted data. FT drafted the manuscript. KS and AB, provided overall and helped drafting the paper and reviewed the paper. Each of the authors read and approved the final manuscript.
The author(s) acknowledge Jimma University Medical center for allowing us to use data and the staff members of the hospital for their support during data collection from patient chart.
[Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Lelisa F, Sisay K, Tesfaye F, Banbeta A (2023) Survival Analysis of Recovery of Weight Among Low Birth Weight Infants in Jimma University Medical Center, Jimma, Ethiopia. Adv Pediatr Res. 10:067.
Received: 29-Nov-2023, Manuscript No. LDAPR-23-28267; Editor assigned: 01-Dec-2023, Pre QC No. LDAPR-23-28267 (PQ); Reviewed: 15-Dec-2023, QC No. LDAPR-23-28267; Revised: 22-Dec-2023, Manuscript No. LDAPR-23-28267 (R); Published: 29-Dec-2023 , DOI: 10.35248/2385-4529.23.10.067
Copyright: © 2023 Lelisa F, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.