Clinical Pediatrics: Open Access
Open Access
ISSN: 2572-0775
ISSN: 2572-0775
Case Report - (2024)Volume 9, Issue 4
Heavy metal toxicity from soft tissue sources is rare and carries unique diagnostic and therapeutic challenges. Our case involves a previously healthy 4-year-old boy who presented to the emergency department due to worsening right hemiscrotal pain and swelling for 10 days, originally attributed to a torsed, unviable testicle. On surgical exploration, several tiny metallic beads were found and later identified as containing mercury.
Heavy metal toxicity; Foreign bodies; Chelation therapy; Lead; Mercury
On further imaging, thousands of hyperdensities were identified in his scrotal and gluteal regions, along with elevated serum concentrations of lead and mercury. The origin of these foreign bodies remains unknown. Our case discusses the unique challenges of heavy metal toxicity originating from soft tissue foreign bodies involving both urgent surgical evaluation and chelation therapy. Our patient tolerated chelation therapy and partial surgical removal of the foreign bodies without signs of sequela after discharge, despite chronic heavy metal toxicity.
A previously healthy 4-year-old boy presented to the emergency department due to worsening right hemiscrotal pain and swelling for 10 days. This was his third presentation for these symptoms, which were originally attributed to a torsed, nonviable testicle. On exam, he had an enlarged right hemiscrotum with purple-red discoloration (Figure 1). A scrotal ultrasound showed normal appearance of the testicle but a heterogenous collection in the anterior scrotal wall with hypervascularity and multiple foci of gas concerning for possible necrotizing fasciitis. Initial laboratory evaluation was notable only for a hemoglobin of 8.8 g/dL with normal inflammatory markers. The patient was started on vancomycin, piperacillintazobactam, and clindamycin and admitted for further management and urgent urologic evaluation.
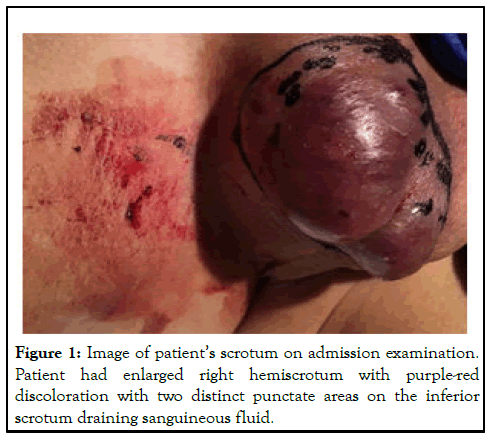
Figure 1: Image of patient’s scrotum on admission examination. Patient had enlarged right hemiscrotum with purple-red discoloration with two distinct punctate areas on the inferior scrotum draining sanguineous fluid.
Upon surgical exploration, reactive scrotal tissue was found without evidence of testicular involvement or infection. Multiple small metallic spheres (0.5 mm-1 mm diameter) were embedded in subcutaneous tissue and within the scrotum (Figure 2). Plain radiography followed by CT revealed extensive spread of hyperdensities throughout the right gluteal muscles, bilateral scrotum, perineal fat, and bilateral thighs (Figures 3 and 4).
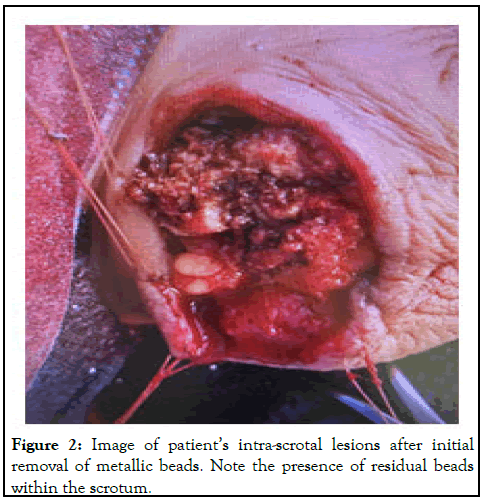
Figure 2: Image of patient’s intra-scrotal lesions after initial removal of metallic beads. Note the presence of residual beads within the scrotum.
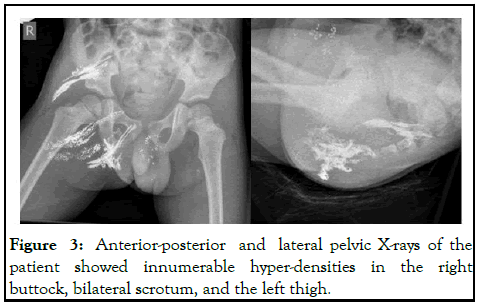
Figure 3: Anterior-posterior and lateral pelvic X-rays of the patient showed innumerable hyper-densities in the right buttock, bilateral scrotum, and the left thigh.
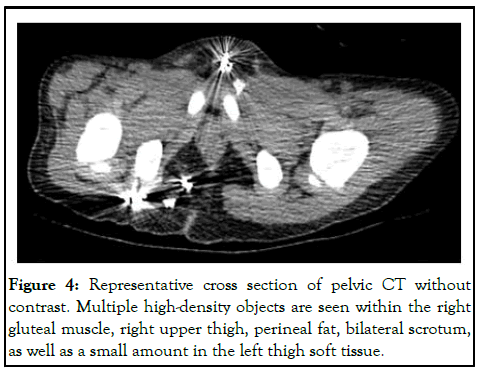
Figure 4: Representative cross section of pelvic CT without contrast. Multiple high-density objects are seen within the right gluteal muscle, right upper thigh, perineal fat, bilateral scrotum, as well as a small amount in the left thigh soft tissue.
Heavy metal testing revealed a blood mercury concentration of 621.1 mcg/L (normal<5 mcg/L) and a blood lead concentration of 120 mcg/dL-130 mcg/dL (normal<5 mcg/dL). 24-hour urine lead and mercury levels were 417.8 mcg/L (normal 0 mcg/L) and >80.0 mcg/L (normal<10 mcg/L), respectively. The zinc protoporphyrin level was elevated to 320 μmolZPP/molHem (normal 30 μmol/mol-80 μmol/mol). The metallic spheres removed during the initial scrotal exploration were found to consist primarily of mercury. Histopathology of the surgical specimens was non-specific, showing dark, spherical globules surrounded by neutrophils, histiocytes, and fibrosis consistent with acute and chronic inflammation (Figure 5).
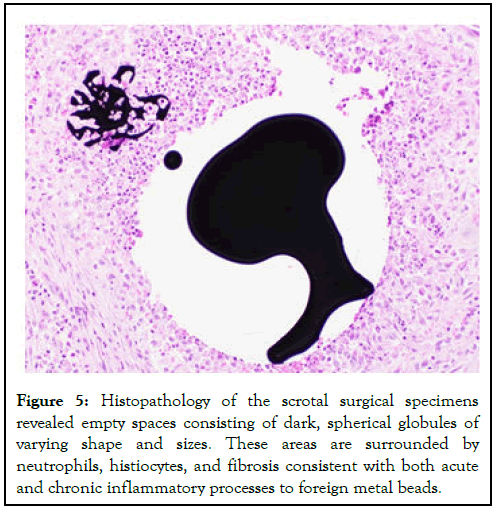
Figure 5: Histopathology of the scrotal surgical specimens revealed empty spaces consisting of dark, spherical globules of varying shape and sizes. These areas are surrounded by neutrophils, histiocytes, and fibrosis consistent with both acute and chronic inflammatory processes to foreign metal beads.
Hospital course
The California poison control system was consulted for guidance in managing heavy metal toxicity. Chelation with succimer was started on hospital day 9 after precise serum metal levels resulted. After extensive multidisciplinary consultations, the patient underwent surgical exploration of the right thigh and buttock on hospital day 16, which revealed countless liquid metal spheres <1 mm in diameter encased in granulomatous material, of which only a small portion could be removed. During his entire 22-day hospitalization, the patient remained asymptomatic beyond pain localized to surgical sites. Serial bedside developmental assessments revealed no cognitive deficits.
At the time of discharge, the origin of the metal in his soft tissue remained unclear. The patient had spent the majority of his first three years of life with his father in China, during which no history was available. Because lead was not conclusively found in the metal samples, we explored possible alternative sources. No source of lead was identified during a home evaluation, and history revealed no use of alternative or herbal medicines. The patient did not have any insight into the origin of the beads. Ultimately, the distribution pattern of the metal on radiography is highly suggestive of intramuscular and intra-scrotal injections of both elemental mercury and lead fragments. Child Protective Services (CPS) was involved throughout the hospitalization, and the patient was ultimately placed in CPS custody. The patient has been well since discharge. His most recent blood lead level was 21.6 mcg/dL and blood mercury 187.9 mcg/L ten weeks after discharge. He remains on succimer therapy. Intramuscular and intra-scrotal injections of elemental mercury and lead fragments.
Heavy metal toxicity is a common concern worldwide. Though most individuals with heavy metal toxicity are exposed via the gastrointestinal tract or the inhalation of metallic dust, there are case reports of toxicity originating from soft tissue sources, including lead toxicity due to retained lead bullet fragments [1,2], and mercury toxicity from injuries with thermometers [3], self-harm attempts [4,5], and alternative medical practices [6]. Heavy metal toxicity from soft tissue sources carries unique diagnostic and therapeutic challenges. While symptoms may not correlate well with serum concentrations, early evaluation and diagnosis can expedite chelation therapy or surgical removal to minimize long term sequelae.
Patients with subcutaneous mercury injections often present weeks to months later with localized abscess formation [5]. Depending on the amount and duration of the exposure, subcutaneous mercury injection can also cause significant systemic symptoms. Case reports of adult patients describe renal and neurological sequelae, including acute tubular necrosis [7], headaches, visual disturbances, psychiatric symptoms [5], ataxia, and vomiting [8]. The blood mercury levels of these patients ranged from 26.3 mcg/L to 300 mcg/L. Our patient had a higher blood mercury level (621.1 mcg/L) than these cases, but he remained asymptomatic. This suggests that systemic symptoms of chronic soft tissue mercury exposure may be highly variable.
Reports of subcutaneous mercury injection in children are rare. In 2014, media outlets reported on a child from China who had several similarities to our case. This five-year-old boy was found to have elemental mercury of unknown origin erupting from his buttocks. Within weeks, the boy was unable to walk and became encephalopathic. Radiographs demonstrated a strikingly similar pattern of hyperdensities in the buttocks and scrotum as in our case. His blood mercury concentration was reported as “200 times normal.” He was treated with a combination of chelation and surgical debridement and improved dramatically.
Though laboratory analyses were unable to conclusively determine whether the foreign bodies contained lead, we suspect that the elevated lead levels in our patient were also a result of subcutaneous injection. Our patient had radiologic signs of diffuse involvement in both his scrotal and buttock regions, but only the scrotal samples were tested by the state laboratory. Given the patient’s elevated lead levels without a clear alternative etiology, we suspect that the buttock injections contained lead.
Reports of subcutaneous injections of lead are also rare. Our patient’s lead levels were well above normal, though he remained asymptomatic.
Lead levels greater than 100 mcg/dL are traditionally associated with severe neurologic sequelae. Despite a lead level of 120 mcg/ dl-130 mcg/dl, our patient had no neurologic symptoms. The lack of symptoms at such an elevated level strongly suggests a chronic exposure. This has been observed in children within gold mining communities of Zamfara, Nigeria. Moreover, our patient’s elevated zinc protoporphyrin and fibrotic histopathology were also consistent with chronic exposure, at least 8 to 12 weeks prior to presentation. Studies of retained lead-containing bullet fragments show that serum lead levels increase with the number of retained fragments and can remain elevated for years after exposure. Symptoms range from asymptomatic to florid lead toxicity and do not seem to correlate with serum lead level.
Possibly the most perplexing aspect of this case is the origin of the lead and mercury. The likelihood of chronic exposure, in combination with the similarities of our case to the child in China, suggests that our patient may have received lead and mercury injections before coming to the United States from China. Mercury was long considered by Eastern civilizations to have magical and medicinal properties, though it is pure speculation to suggest lingering beliefs played a role here. Nonetheless, the mystery of who inflicted this and why remains unsolved.
The treatment options for heavy metal toxicity from a soft tissue source include surgical removal and chelation. Surgical removal was performed in all the aforementioned published cases of mercury toxicity with success. However, the distribution of thousands of millimeter-sized pellets throughout anatomically complex sites, as in our patient, presents an extraordinary surgical challenge. Removing all foreign material appears nearly impossible, and each attempt carries the risk of permanent physical disfigurement and infertility. On the other hand, leaving metal behind carries the risk of future toxicity. Chelation is a less invasive intervention, but inadequate alone. Though chelation can be initiated rapidly, there is conflicting evidence about chelation prior to surgical removal. Historically, there has been concern that chelation could cause increased neurotoxicity if metal is still present in the gastrointestinal tract or in the soft tissue. Recent animal studies have had contrary results. Ideally, both chelation and surgical removal would be performed as soon as safely possible. We suggest making these decisions in conjunction with a surgeon and medical toxicologist. Because the majority of our patient’s metal burden could not be removed surgically, his long-term prognosis is unclear. Chelation with succimer continues, which carries the risk of the depletion of essential elements and stunted growth and development, though this would be difficult to distinguish from chronic lead and mercury toxicity.
In a young child with chronic soft tissue exposure to heavy metals, such as mercury and lead, alternative medical practices and child abuse must be considered in the differential diagnosis. The management of lead and mercury toxicity originating from soft tissue foreign bodies involves urgent surgical evaluation and chelation therapy. Minuscule deeply imbedded foreign bodies present a unique risk and challenge for surgical removal.
Because severe heavy metal toxicity is rare in the United States, prompt involvement of the state’s poison control experts can inform clinical decision making. A multidisciplinary approach including pediatricians, surgeons, and medical toxicologists should be used. Children may also need long-term follow up with experienced outpatient clinicians given their high risk of developmental complications.
The authors acknowledge the medical staff of the Santa Clara valley medical center and the California poison control system, for their contributions to the patient’s evaluation, diagnosis, and management.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed ]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Landsman A (2024) 4-Year-Old Boy with Right Scrotal Pain, Discoloration and Swelling. Clin Pediatr. 9:275.
Received: 14-May-2020, Manuscript No. CPOA-24-4234; Editor assigned: 19-May-2020, Pre QC No. CPOA-24-4234 (PQ); Reviewed: 02-Jun-2020, QC No. CPOA-24-4234; Revised: 15-May-2024, Manuscript No. CPOA-24-4234 (R); Published: 12-Jul-2024 , DOI: 10.35248/2572-0775.24.09.275
Copyright: © 2024 Landsman A. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.