Journal of Cell Science & Therapy
Open Access
ISSN: 2157-7013
ISSN: 2157-7013
Commentary - (2021)
The immune system is the body's protection against contamination and malignant growth. It is comprised of billions of cells that are partitioned into a few distinct sorts. Lymphocytes, a subtype of white platelets, include a significant piece of the insusceptible framework. There are three kinds of lymphocytes. B lymphocytes (B cells) make antibodies to fight infection.T lymphocytes (T-cells) have several functions, including helping B lymphocytes to make antibodies to fight infection, and directly killing infected cells in the body.Natural killer cells also attack infected cells and eliminate viruses.
Immunotherapy
Immunotherapy is a sort of therapy that uses the body's own safe framework to battle disease. It improves the body's capacity to distinguish and kill malignant growth cells. It is dependent on the idea that resistant cells or antibodies can perceive and kill malignant growth cells.
Resistant cells or antibodies can be delivered in the research facility under firmly controlled conditions and afterward given to patients to treat malignant growth. A few sorts of immunotherapy are either supported for use or are under investigation in clinical preliminaries to decide their viability in treating different kinds of malignant growth.
How it works?
Lymphocytes are gathered from a patient. Lymphocytes are gathered through apheresis, a strategy during which blood is removed from the body and at least one blood parts (like plasma, platelets or white platelets) are taken out. The excess blood is then gotten back to the body. Lymphocytes are reengineered in a research center. The T-cells are shipped off a research center or a medication fabricating office where they are hereditarily designed, by bringing DNA into them, to deliver illusory antigen receptors (CARs) on the outside of the phones. After this reengineering, the T-cells are known as "illusory antigen receptor (CAR) T-cells." CARs are proteins that permit the T-cells to perceive an antigen on designated tumor cells. The reengineered CAR T-cells are then increased. The quantity of the patient's hereditarily adjusted T-cells is "extended" by developing cells in the research center. When there are sufficient of them, these CAR T-cells are frozen and shipped off the emergency clinic or focus where the patient is being dealt with. At the medical clinic or therapy focus, the CAR T-cells are defrosted and afterward imbued into the patient. Numerous patients are given a short course of at least one chemotherapy specialists, called "lymphodepletion," before they get the imbuement of CAR Tcells. Vehicle T-cells that have been gotten back to the patient's circulation system duplicate in number. These are the "assailant" cells that will perceive, and assault, cells that have the designated antigen on their surface. The CAR T-cells might help guard against repeat. Vehicle T-cells might kill the entirety of the malignant growth cells and may stay in the body a very long time after the imbuement has been finished. The treatment has brought about long haul reductions for certain sorts of blood malignancy (Figure 1).
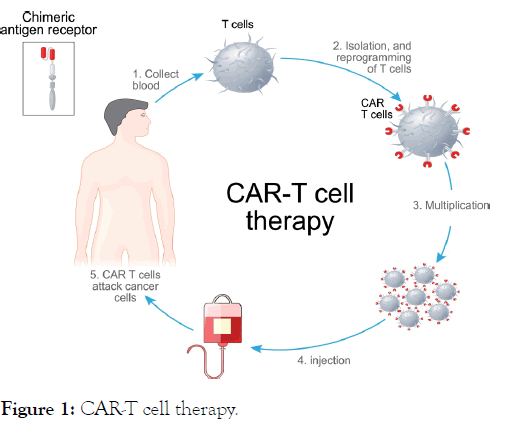
Figure 1: CAR-T cell therapy.
Fanciful antigen receptor T-cell clinical preliminaries have produced amazing outcomes in the early results of CAR T-cell treatment patients with blood diseases. In certain examinations, up to 90 percent of youngsters and grown-ups with B-ALL whose infection had either backslid on various occasions, or neglected to react to standard treatments, accomplished reduction in the wake of getting CAR T-cell treatment. Backslides might be because of the tumor cells losing the statement of the bunch of separation (CD-19) antigen, the restricted ingenuity of CAR Tcells, or hindrance of CAR T-cell action. Investigations of CAR T-cell treatment in other blood malignant growths, including Chronic Lymphocytic Leukemia (CLL), just as various myeloma, additionally show potential. Examination is likewise under way, investigating the utilization of CAR T-cell treatment in the treatment of strong tumors. Most patients partaking in CAR Tcell preliminaries have just been followed for a moderately brief time frame; be that as it may, information giving data about early reactions to treatment is quick arising. Specialists will actually want to foresee the span of these reactions after preliminary members have been followed over the long haul. It is significant for more pediatric and grown-up patients to be taken on clinical preliminaries. Bigger examination tests, assessed over more broadened periods, will assist analysts with advancing the effect of this kind of treatment, approaches to diminish its poisonousness and work on the administration of unfriendly incidental effects.
Chimeric Antigen Receptor T-cells have changed the immunotherapeutic therapy of disease: invigorating outcomes in headstrong and backslid B-cell malignancies have been distributed. Neurologic confusions, strong growth the executives and allogeneic develops require further examination. All in all, further plan changes will empower CAR T-cells to unequivocally reshape the field of malignancy immunotherapy.
Citation: Ramos D (2021) A Brief Discussion about CART-Cell Therapy. J Cell Sci Therapy.S5:312.
Received: 06-Aug-2021 Accepted: 20-Aug-2021 Published: 27-Aug-2021 , DOI: 10.35248/2157-7013.21.s5.312
Copyright: © 2021 Ramos D. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.