
Journal of Clinical Trials
Open Access
ISSN: 2167-0870

ISSN: 2167-0870
Case Report - (2023)
Background: Chylous ascites refers to accumulation of milk-like peritoneal fluid rich in triglycerides in the abdominal cavity and is a rare presentation. The remaining causes of chylous ascites include lymphatic malformation, cirrhosis, tuberculosis, and malignancy.
Case Presentation: A 68-year-old man presented to our geriatric department with abdominal distention and edema of both lower limbs. The abdominal ultra-sound showed high volume ascites and the diagnostic paracentesis revealed milk-like peritoneal fluid rich in triglycerides. Upper digestive endoscopy was performed and revealed poorly differentiated gastric adenocarcinoma on biopsy. The patient was transferred to oncology department and died 2 weeks later.
Conclusion: Chylous ascites may be the earliest manifestation of poorly differentiated gastric adenocarcinoma, even if not accompanied by other symptoms of malignancy.
Poorly differentiated gastric adenocarcinoma; Chylous ascites; Paracentesis.
Chylous asicites is defined as the milk-like peritoneal fluid and triglycerides-rich (>200 mg/dL) intraabdominal effusion. Chylous asicites may also be divided into congenital chylous asicites and secondary chylous asicites according to the etiology [1]. Congenital chylous asicites mostly occurs in infants within 3 months, usually related to congenital lymphatic vessel development abnormalities. Secondary chylous asicites can be divided into traumatic (such as trauma, iatrogenic injury, etc.) and non-traumatic (such as cirrhosis, infection, malignancy, inflammation, autoimmune diseases, drugs, etc.). The remain causes of chylous asicites include lymphatic malformation (32%), cirrhosis (11%), tuberculosis (10%), malignancy (7%) [2]. Poorly differentiated gastric adenocarcinoma is of a relatively high malignant degree, and is usually found in the middle and late stage, and has a rapid onset, with a poor prognosis [3]. This paper reports a quite rare case of chylous ascites associated with poorly differentiated gastric adenocarcinoma and highlights the difficulties regarding diagnoses and some literature issues.
A 68-year-old man presented with a chief complaint of abdominal distention and edema of both lower limbs. He had medical history of type 2 diabetes in 2015 and bone tuberculosis surgery in 2019. There was no documented history of chronic alcoholism, chronic hepatic disease, weightloss, and fever, yellowish discoloration of skin, gastrointestinal bleeding, melena, dark-colored urine or pale stool. The abdominal ultrasound confirmed ascites.
At the time of consultation, his height was 173.0 cm, body weight was 105.0 kg, body mass index was 35.08; his vital signs were as follows: Body temperature 36.4°C, blood pressure 132/89 mmHg, heart rate at 94/min, oxygen saturation at 98% (room air); the movement dullness was positive.
Hematology and biochemistry investigation on presentation demonstrated B-type natriuretic peptide (12.30 pg/mL), urea nitrogen (3.90 mmol/L), blood creatinine (61.80 umol/L), high C-reactive protein (19.40 mg/L), Neutrophil counts (7.25 × 109/L), Percentage of neutrophils (82.66%), Serum albumin (31.00 g/L), Carcinoembryonic antigen (24.75 ng/mL), Carbohydrate antigen19-9 (>1200.00 U/mL), Carbohydrate antigen-125 (616.30 U/mL).
Abdominal Computed Tomography (CT) scan was performed and it revealed lateral wall of lesser curvature of stomach thickening and inner edge depression, Local ascending colon thickening, retroperitoneal lymph node enlargement (Figure 1).
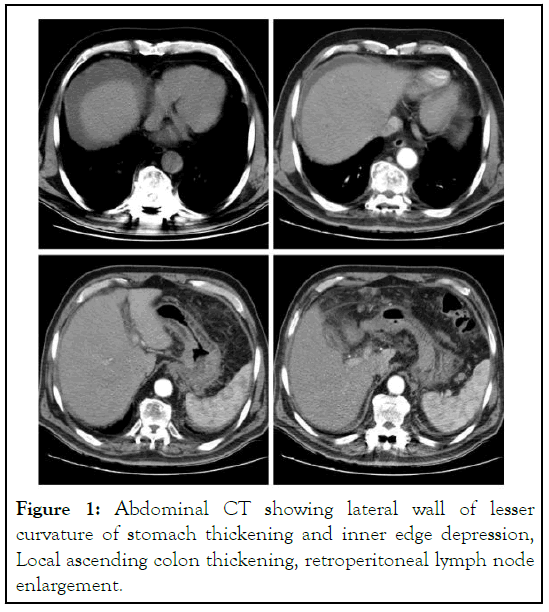
Figure 1: Abdominal CT showing lateral wall of lesser curvature of stomach thickening and inner edge depression, Local ascending colon thickening, retroperitoneal lymph node enlargement.
Paracentesis was performed and showed milk-like fluid rich in triglycerides (>200 mg/dL), diagnosing chylous ascites. Exfoliation cytology performed heterotype cells in ascites (Figure 2).
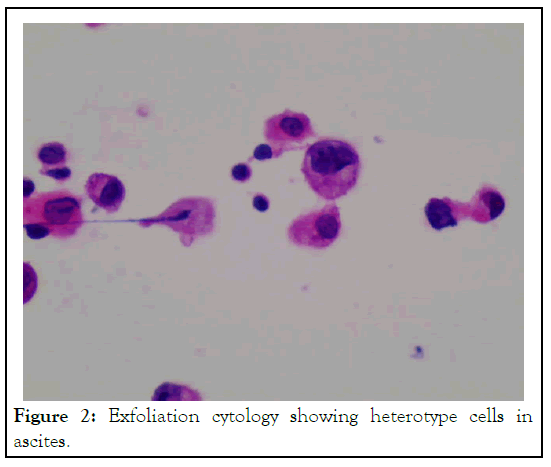
Figure 2: Exfoliation cytology showing heterotype cells in ascites.
Upper digestive endoscopy showed infiltrative ulcerated gastric lesions (3 cm × 4 cm) with signs of blood scab and white fur (Figure 3). The lesions histology revealed poorly differentiated gastric adenocarcinoma (Figure 4).
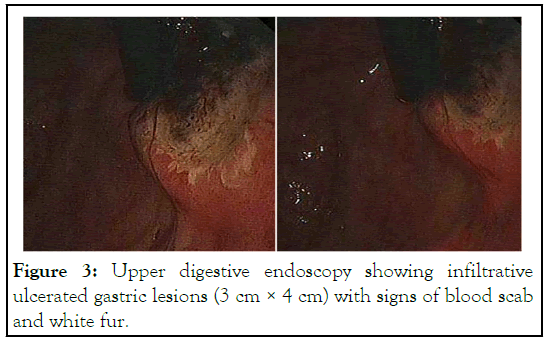
Figure 3: Upper digestive endoscopy showing infiltrative ulcerated gastric lesions (3 cm × 4 cm) with signs of blood scab and white fur.
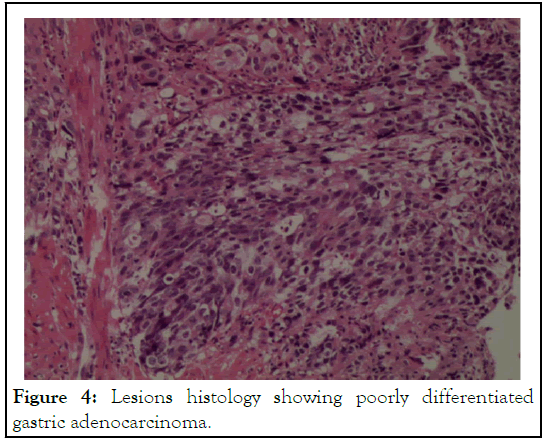
Figure 4: Lesions histology showing poorly differentiated gastric adenocarcinoma.
The patient was transferred to oncology department and treated by chemotherapy.
The most common clinical symptom of chylous ascites is abdominal distension (81%), followed by abdominal pain or peritonitis (11%), and a few patients are combined with overweight or dyspnea [4]. Other non-specific symptoms include anorexia, fatigue, diarrhea, edema, nausea, enlarged lymph nodes, early satiety, and low-heat in the afternoon, and night sweats. For patients with cirrhosis, jaundice, liver palm and spider nevus could be presented. Pay attention to the patient's history of malignancy, history of recent abdominal surgery, history of found mental hepatic disease, family history and history of tourism [5].
Laboratory examinations include: Hemocyte analysis, liver and kidney function, lactate dehydrogenase, adenosine dehydrogenase, tuberculosis antibodies, gamma-interferon test, tumor markers, etc. Auxiliary examinations include abdominal imaging, abdominal puncture and laboratory examination of ascites, lymphangiography, and lymphoscopy and so on.
Imaging examinations include abdominal CT, MRI, or ultrasound. It is necessary for the diagnosis of abdominal masses and enlarged lymph nodes. The imaging characteristics of abdominal CT scan in chylous asicites patients is the formation of fatty fluid surfaces. Similar imaging characteristics may be observed in abdominal ultrasound. PET-CT has some implications for the diagnosis of abdominal malignancy and lymphadenoma [6].
Abdominal paracentesis is the most important means for diagnosing and clarifying the nature of asicites. Laboratory examinations of chylous asicites include appearance of ascites, cell counts, lactate dehydrogenase, adenosine dehydrogenase, albumin, amylase, tuberculosis antibody, gram staining, and culture of ascites, cytological examination, and peritoneal biopsy.
Lipoprotein electrophoresis is the gold standard for the presence of chylomicrons in the chylous asicites [7]. When lipoprotein electrophoresis could not be performed, elevated triglyceride level is another important indicator for diagnostic chylous asicites. The cut-off value of the triglyceride for diagnostic chylous asicites is 187 mg/dL (2.13 mmol/L) and its sensitivity and specificity is up to 95% [8].
Lymph allography is considered a gold standard for the diagnosis of chylous asicites in the presence of lymphatic obstruction. Lymphangiography and lymphoscopy are suitable for selecting lymph nodes in patients requiring surgery, evaluation of therapeutic effect, enlarged retroperitoneal lymph nodes, in addition to showing leakage of the thoracic duct, fistula formation [9]. Lymphoscopy can accurately determine the location of lymphatic leakage and clarify a diagnosis combined with PET/CT.
In this report, despite the patient had history of bone tuberculosis surgery, he was without signs of chronic hepatic disease, heart failure, renal failure, hypothyroidism. He also did not have medical history of traumatic injury. In the clinical field, constitutional symptoms are common but not specific, such as abdominal distention and edema. Furthermore, abdominal pain, weight loss, diarrhea, steatorrhea, malnutrition, edema, enlarged lymph nodes, early satiety, fevers, and night sweats are others related features.
Our patient initially complained of abdominal distention and edema of both lower limbs. Others general aspects found were lateral wall of lesser curvature of stomach thickening, inner edge depression, and local ascending colon thickening and enlarged retroperitoneal lymph nodes at CT scan. Despite CT of the abdomen being an important imaging exam to diagnose ascites, in this case the ultrasound of the abdomen was decisive to confirm this hypothesis and lead to abdominal paracentesis. This procedure is the most important tool in evaluation and management of patients with ascites. The character of ascites was milk-like pattern and subsequent analysis disclosed high triglycerides levels.
Exfoliative cytology of ascites found heterotype cells. The histology revealed poorly differentiated gastric adenocarcinoma after upper digestive endoscopy due to ulcerated gastric lesions. Adenocarcinoma is a type of gastric cancer. Poorly differentiated gastric adenocarcinoma is one of the most common types of gastric adenocarcinoma, which is a more malignant type in gastric adenocarcinoma. Poorly differentiated gastric adenocarcinoma often has local lymph node metastasis, ascites or distant metastasis. The rate of surgical resection is low and the five-year survival rate is also relatively low even if chemotherapy [10]. Pathological results are the gold standard for the diagnosis of tumors.
After the diagnosis was confirmed, the patient was transferred to oncology department and treated by chemotherapy.
Chylous asicites is a rare disease, mostly secondary to a traumatic and non-traumatic etiology. Liver cirrhosis and malignancy are the main causes. The diagnosis is mainly based on the results of the asicites examination and the asicites is milklike and high triglyceride levels. At the same time, a conservative diet, such as high protein, low fat, rich in medium-chain triglyceride diet, is adopted. Some drugs, such as octreotide, somatostatin, and orlistat may work in some cases. This case has been clearly diagnosed as poorly differentiated gastric adenocarcinoma. Treatment of the malignancy is next required.
None.
[Cross Ref] [Google Scholar].
[Cross Ref] [Google Scholar] [Pub Med].
[Cross Ref] [Google Scholar] [Pub Med].
[Cross Ref] [Google Scholar] [Pub Med].
[Cross Ref] [Google Scholar] [Pub Med].
[Cross Ref] [Google Scholar] [Pub Med].
[Cross Ref] [Google Scholar] [Pub Med].
[Cross Ref] [Google Scholar] [Pub Med].
[Cross Ref] [Google Scholar] [Pub Med].
[Cross Ref] [Google Scholar] [Pub Med].
Citation: Liu X, Liu C (2023) A Case Report of Chylous Ascites due to Poorly Differentiated Gastric Adenocarcinoma. J Clin Trials. S22:001.
Received: 19-Apr-2023, Manuscript No. JCTR-23-23601; Editor assigned: 21-Apr-2023, Pre QC No. JCTR-23-23601(PQ); Reviewed: 05-May-2023, QC No. JCTR-23-23601; Revised: 12-May-2023, Manuscript No. JCTR-23-23601(R); Published: 22-May-2023 , DOI: 10.35248/2167-0870.23.S22.001
Copyright: © 2023 Liu X, e t al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.