Journal of Psychology & Psychotherapy
Open Access
ISSN: 2161-0487
ISSN: 2161-0487
Research - (2024)Volume 14, Issue 3
Objective: To study the Fear of Cancer Recurrence (FCR) of individuals with Non-Small Cell Lung Cancer (NSCLC); this research focused on developing and validating a prediction model to identify which individuals with NSCLC were at high risk of relapse fear.
Materials and methods: The sociodemographic and clinical variable data of 347 NSCLC patients from the department of thoracic surgery, cancer hospital of Chinese academy of medical sciences from December 2020 to September 2022 were collected by convenience sampling. The t-test, Analysis of Variance (ANOVA), and nonparametric test were used to test the difference of a single factor in the disease fear scores of patients with NSCLC with different demographic characteristics and disease-related conditions. After the disease fear scores were converted into binary data (fear and no fear), the univariate logistic regression analysis was conducted according to the univariate analysis. Multivariate logistic regression analysis was conducted by adjusting the relevant covariates to establish a risk prediction model for NSCLC patients to fear disease progression.
Results: Gender, ethnicity, family per capita monthly income, and hope level were independent predictors of cancer recurrence fear in patients with non-small cell lung cancer. The model established by these predictors showed that the area under the curve was 0.891, 95% confidence interval: 0.858-0.924.
Conclusion: This study developed a validated and easy-to-use prediction algorithm that can be used to identify patients at high risk of recurrence fear with moderate accuracy.
Non-small cell lung cancer; Fear of cancer recurrence; Prediction model
Lung cancer is the second most widely occurring cancer and the most common cause of cancer-related death around the globe. According to the global cancer data statistics in 2020, about 2.2 million new lung cancer cases worldwide, and about 1.8 million patients die of lung cancer annually. The mortality rate is more than 25% and ranks first annually. Histologically, Non-Small Cell Lung Cancer (NSCLC) makes up approximately 85% of all lung cancer cases, and the incidence rate has been rising in recent years [1]. Currently, the primary treatment of NSCLC follows the principle of comprehensive treatment based on surgery, including radiotherapy, chemotherapy, molecular targeted therapy and neoadjuvant immunotherapy [2]. With the development of treatment technology, a survey shows that the competitive survival rate of lung cancer patients in the five years’ post-surgery has increased from 71.7% to 85.4%. In addition, molecular targeted therapy and immunotherapy have shown good results for individuals with sensitive gene mutations and advanced NSCLC post-surgery, improving the survival time of patients and making it possible to reduce the rate of metastasis and recurrence [3]. In recent years, there have been studies on neoadjuvant immunotherapy [4-6]. An important treatment method for locally advanced lung cancer is a preoperative treatment followed by surgery. Preoperative chemotherapy immunotherapy and adjuvant immunotherapy can improve the prognosis of selected respectable lung cancer patients, which makes some patients suspected of lymph node metastasis before surgery achieve a decline or can be operated on [7]. However, evidence suggests that 50% of patients after surgery still face the risk of recurrence and metastasis, bringing a heavy psychological burden to the affected individuals [8,9].
After a patient is diagnosed with cancer, the Fear of Cancer Recurrence (FCR) is among the most worrying problems of affected individuals, and it is also their common experience. Therefore, they seek the help or support of experts. FCR is defined as "fear, worry or anxiety related to the possibility of cancer recurrence or progression" [10]. Therefore, the FCR may pose a problem, whether for patients who are curable and afraid of a recurrence of cancer or for those who are afraid of the progression of cancer in its advanced stage. Patients with psychological illnesses such as generalized anxiety disorder or illness anxiety disorder may have a higher risk of serious fear of recurrence. However, the FCR of most patients only reaches a clinically meaningful level and cannot be regarded as a psychological disease, indicating that FCR is a unique and important mental health problem. Mild FCR usually improves over time. However, if the FCR becomes serious, it may cause significant damage to health and quality of life [11]. This psychological state of fear and worry runs through the entire course of treatment and survival. It profoundly impacts the survival time and quality of life of individuals with cancer. Another study shows that about 49% of cancer patients have various degrees of FCR. If they live in fear for a long time, it reduces their compliance to treatment, seriously affecting their quality of life and social functions, and increases their medical expenses [12]. The study found that FCR is the most common psychological reaction of patients with breast, colorectal, testicular, head, neck, lung, endometrial, thyroid, and other cancers [13]. Some data show that the detection rate of FCR is the highest among lung cancer patients, and this psychological reaction can be considered as a disease that affects the mental health of patients. The high occurrence rate and potential severity of FCR are noteworthy [14]. It makes cancer survivors feel unfortunate and reduces their compliance with follow-up recommendations. Studies show a correlation between FCR and depression, poor quality of life and impaired daily functions [15]. Some patients avoid follow-up and screening, which may lead to the risk of late recurrence and shorten their survival time. On the contrary, some patients may constantly check their bodies and consult doctors frequently, wasting medical resources and causing long-term persistent anxiety. Therefore, early and effective identification, prediction and evaluation of FCR have become the focus of clinical attention.
For patients with early NSCLC, the recurrence rate after surgery is high, causing serious anxiety in patients. In the context of precise medical treatment of tumours, medical staff needs to identify people with lung cancer who are prone to fear and timely and predictive treatment and nursing. FCR is an emerging research topic. There are validated tools to evaluate FCR, including some specially developed for clinical trials [16,17]. However, currently, it is not possible to evaluate FCR systematically. How to evaluate patients accurately and comprehensively with early NSCLC, identify the correlation between cancer recurrence fear and various predictive factors, develop reliable prediction tools, and identify the FCR of individuals with NSCLC at an early stage has become the key to prolonging the survival time and improve the quality of life of individuals with NSCLC diagnosed at an early stage. Although some studies have explored the correlation factors of relapse fear in patients with NSCLC, some contradictory conclusions have been drawn due to the limited number of potential predictors. There is no research to explore the risk prediction model of FCR in patients with early NSCLC. Therefore, this research was conducted to determine predictors of FCR in individuals with NSCLC. Furthermore, a prediction algorithm was developed which can help clinicians and nurses identify potential high-risk patients with FCR.
This study was approved by the research ethics committee of cancer hospital of Chinese academy of medical Sciences, (22/055-3256).
Patient’s selection and data collection
Using the convenient sampling method, 347 individuals with Non-Small Cell Lung Cancer (NSCLC) hospitalized in the department of thoracic surgery, cancer hospital of Chinese academy of medical sciences from December 2020 to September 2022 were selected as the study subjects.
The inclusion criteria of the study were as follows:
• Age ≥ 18 years.
• Patients diagnosed with malignant nodules by preoperative imaging and confirmed as NSCLC by intraoperative frozen pathological examination.
• Patients who provided their informed consent, willing to participate in the investigation.
Exclusion criteria were as follows:
• Cognitive impairment
• Obstacles in communication (different language) or inability to understand the text. The sample size was estimated according to the algorithm designed by the cross-sectional survey: 
In this algorithm, π and δ represent the occurrence rate and allowable error, respectively. After setting α as 0.05, π as 0.5, and δ as 0.5, the expected sample size of 347 cases was calculated.
Survey instrument
Questionnaire: The researcher designed and collected sociodemographic variables, including gender, age, etc. Simultaneously, the following clinical variables were collected: Combined basic diseases, radiotherapy, chemotherapy, incidence frequency, etc. Fear of Progression Questionnaire‐Short Form (FoP-Q-SF): It was prepared by Mehnert, et al. and translated into Chinese by Wu Qi-yun, et al. [18,19]. There were 12 items, with a score range of 12 to 60 points. The Likert 5 rating was assigned 1 to 5 points from "never" to "always". The higher the score, the stronger the fear. The correlation coefficient between Chinese and original entries ranged from 0.58 to 0.71. The coefficient of Cronbach's α was set to 0.88. The Herth Hope Index (HHI) was compiled by the American Herth [20], and translated and revised by Chinese scholar Zhao Haiping, et al. [21]. It is widely used to determine the levels of hope in individuals with cancer. The scale comprised three subscales: Positive attitude towards reality and the future (4 items), adopting positive actions (4 items), and maintaining close relationships with others (4 items), which are composed of 12 items. Each item was scored with Likert 4. The total score on the scale ranged from 12 to 48. The higher the score, the higher the patient's hope level. The hope level measured was 12 to 23 points, indicating a low level of hope; 24~35 points indicated a moderate level of hope; 36~48 points indicated elevated hope levels. The Herth scale had good reliability, validity and feasibility, with a retest reliability of 0.92, internal consistency reliability of 0.87, and construct validity of 0.85.Investigation methods
This research was carried out strictly per the Helsinki declaration's provisions. This study employed a convenient sampling method to collect data through the face-to-face issuance of an electronic questionnaire QR code. For patients who visited the department of thoracic surgery of cancer hospital of the Chinese academy of medical sciences between September 2021 and September 2022, all patients who met the study criteria were pre-investigated and completed the questionnaire anonymously during their hospitalization based on their actual condition. The information in the forms was then verified by comparing the medical records of subjects in the hospital's information system to ensure the accuracy of the information.
Statistical analysis
The sociodemographic and clinical aspects of patients, the hope level scale, and the fear of disease progression scale scores were statistically described (the measurement data of normal distribution were expressed by mean ± standard deviation; the measurement data of skewed distribution were expressed by median ± interquartile range; the counting data were expressed by rate or constituent ratio). T-test, analysis of variance and nonparametric test were used to test the univariate difference of disease fear scores of patients with NSCLC having different demographic characteristics and disease-related conditions. After the conversion of FCR to binary data (fear and no fear), a univariate logistic regression analysis was conducted. According to the univariate analysis, a multivariate logistic regression analysis was carried out by adjusting the relevant covariates. A risk prediction model for fear of cancer progression in individuals with NSCLC was established. By drawing the Receiver Operating Characteristic curve (ROC), the Area Under the ROC (AUC), i.e., C statistics, was calculated to evaluate the discrimination ability of the risk prediction model for fear of disease progression. AUC below 0.6 presented low discrimination, 0.6-0.75 presented medium discrimination, and above 0.75 presented high discrimination. The calibration ability of the prediction model was evaluated by the Hosmer-Lemeshow goodness of fit test. The difference between the model's predicted value and the actual observation value was not significant (P>0.05), and the model had good calibration ability. Simultaneously, the Decision Curve Analysis (DCA) was drawn to assess the clinical effectiveness of the risk diagnosis model.
Baseline table of social demography and clinical variables
In this research, 365 questionnaires were distributed, out of which 347 were eventually returned, with an effective recovery rate of 95%. Among them, the majority of patients were female (207; 59.7% (n=347)). The Han nationality accounted for the highest proportion (318; 91.6% (n=347)). Most patients had received general secondary and higher education (204; 58.8% (n=347)) were married (323; 93.1% (n=347)). The average monthly income per capita was (126; 36.3% (n=347)), and more than half of the patients had no smoking history (285; 82.1% (n=347)) and no family history (237; 68.3% (n=347)). More than 85.0% of the patients were in the early stage of pathological staging and had no metastasis (92.5% (n=347)) (Table1).
| Variable | All participants, n (%)/mean (SD) |
|---|---|
| Gender, (n=347) | |
| Male | 140 (40.3%) |
| Female | 207 (59.7%) |
| Age, year | 53.77 ± 11.28 |
| Ethnicity, (n=347) | |
| Han nationality | 318 (91.6%) |
| Ethnic minorities | 29 (8.4%) |
| Education level, (n=347) | |
| Junior high school or below | 76 (21.9%) |
| High school graduate | 67 (19.3%) |
| College graduate or above | 204 (58.8%) |
| Marital status, (n=347) | |
| Unmarried | 15 (4.3%) |
| Married | 323 (93.1%) |
| Divorced | 9 (2.6%) |
| Monthly income, (n=347) | |
| <3000, yuan | 61 (17.6%) |
| 3000-5000, yuan | 126 (36.3%) |
| 5001-10000, yuan | 92 (26.5%) |
| >10000, yuan | 68 (19.6%) |
| Place of residence, (n=347) | |
| City | 20 (5.8%) |
| Villages and towns | 91 (26.2%) |
| Rural | 236 (68.0%) |
| Living alone, (n=347) | |
| Yes | 96 (27.7%) |
| No | 251 (72.3%) |
| Smoking, (n=347) | |
| Yes | 62 (17.9%) |
| No | 285 (82.1%) |
| Family history, (n=347) | |
| Yes | 110 (31.7%) |
| No | 237 (68.3%) |
| Combined with the underlying disease, (n=347) | |
| Yes | 115 (33.1%) |
| No | 232 (66.9%) |
| Course classification, (n=347) | |
| 0-12, month | 278 (80.1%) |
| 13-36, month | 49 (14.1%) |
| >36, month | 20 (5.8%) |
| Number of lesions, (n=347) | |
| A single | 187 (53.9%) |
| Multiple | 160 (46.1%) |
| T, (n=347) | |
| T0 | 295 (85.0%) |
| T1 | 45 (13.0%) |
| T2 | 6 (1.7%) |
| T3 | 1 (0.3%) |
| T4 | 0 (0%) |
| N, (n=347) | |
| N0 | 321 (92.5%) |
| N1 | 10 (2.9%) |
| N2 | 16 (4.6%) |
| N3 | 0 (0.0%) |
| Preoperative tumor indicators, (n=347) | |
| Normal | 197 (69.1%) |
| Abnormal | 88 (30.9%) |
| Chemotherapy, (n=347) | |
| Yes | 31 (8.9%) |
| No | 316 (91.1%) |
| Radiotherapy, (n=347) | |
| Yes | 9 (2.6%) |
| No | 338 (97.4%) |
| Medical payment method, (n=347) | |
| Own expense | 22 (6.3%) |
| Public expense | 39 (11.2%) |
| Medical insurance | 286 (82.4%) |
| Fear of illness score, (n=347) | 29.10 ± 9.10 |
| Health hope index, (n=347) | 22.97 ± 3.44 |
Table 1: Demographic data of the participants, (n=347)
Comparison of FCR scores with the general data of patients
The outcomes of the univariate analysis revealed significant differences in FCR scores among patients with NSCLC of different ages, education levels, per capita monthly income, residence, whether they had received chemo and radiotherapies, and hope levels (P<0.05) (Table 2).
| Variable | N | Score (mean ± SD) | t/Fvalue | p value |
|---|---|---|---|---|
| Gender, (n=347) | -1.347 | 0.179 | ||
| Male | 140 | 27.28 ± 9.73 | ||
| Female | 207 | 30.33 ± 8.442 | ||
| Age, year, (n=347) | 16.295 | <0.001 | ||
| 18-35, year | 30 | 32.73 ± 7.12 | ||
| 36-60, year | 219 | 30.45 ± 9.33 | ||
| >60, year | 98 | 24.96 ± 7.66 | ||
| Ethnicity, (n=347) | -1.413 | 0.159 | ||
| Han nationality | 318 | 28.89 ± 8.94 | ||
| Ethnic minorities | 29 | 31.38 ± 10.49 | ||
| Education level, (n=347) | 4.411 | 0.013 | ||
| Junior high school or below | 76 | 26.43 ± 10.87 | ||
| High school grad | 67 | 29.31 ± 7.83 | ||
| College graduate or above | 204 | 30.02 ± 8.59 | ||
| Marital status, (n=347) | 2.007 | 0.136 | ||
| Unmarried | 15 | 33.67 ± 8.77 | ||
| Married | 323 | 28.88 ± 8.99 | ||
| Divorced | 9 | 29.44 ± 11.90 | ||
| Monthly income, (n=347) | 9.107 | <0.001 | ||
| <3000, yuan | 61 | 29.30 ± 10.32 | ||
| 3000-5000, yuan | 126 | 31.60 ± 9.52 | ||
| 5001-10000, yuan | 92 | 25.32 ± 6.69 | ||
| >10000, yuan | 68 | 29.41 ± 8.36 | ||
| Place of residence, (n=347) | 5.357 | 0.005 | ||
| City | 20 | 26.80 ± 11.52 | ||
| Villages and towns | 91 | 31.68 ± 9.51 | ||
| Rural | 236 | 28.30 ± 8.52 | ||
| Living alone, (n=347) | ||||
| Yes | 96 | 29.07 ± 9.14 | -0.032 | 0.975 |
| No | 251 | 29.11 ± 9.09 | ||
| Smoking, (n=347) | 13 | -1.73 | 0.088 | |
| Yes | 62 | 27.00 ± 10.91 | ||
| No | 285 | 29.55 ± 8.60 | ||
| Family history, (n=347) | 0.472 | 0.637 | ||
| Yes | 110 | 29.44 ± 9.00 | ||
| No | 237 | 28.94 ± 9.15 | ||
| Combined with the underlying disease, (n=347) | -1.347 | 0.179 | ||
| Yes | 115 | 28.17 ± 8.48 | ||
| No | 232 | 29.56 ± 9.36 | ||
| Course classification, (n=347) | 0.733 | 0.481 | ||
| 0-12, month | 278 | 28.81 ± 9.09 | ||
| 13-36, month | 49 | 30.39 ± 9.11 | ||
| >36, month | 20 | 30.00 ± 9.24 | ||
| Number of lesions, (n=347) | ||||
| A single | 187 | 28.84 ± 9.43 | -0.56 | 0.576 |
| Multiple | 160 | 29.39 ± 8.69 | ||
| T, (n=347) | 1.571 | 0.196 | ||
| T0 | 295 | 29.31 ± 9.13 | ||
| T1 | 45 | 26.96 ± 8.35 | ||
| T2 | 6 | 34.00 ± 11.15 | ||
| T3 | 1 | 34.00 ± 0.00 | ||
| T4 | 0 | 0 | ||
| N, (n=347) | 0.303 | 0.739 | ||
| N0 | 321 | 29.17 ± 8.92 | ||
| N1 | 10 | 29.40 ± 11.23 | ||
| N2 | 16 | 27.38 ± 11.42 | ||
| N3 | 0 | 0 | ||
| Preoperative tumor indicators, (n=285) | -0.572 | 0.568 | ||
| Normal | 197 | 28.45 ± 8.43 | ||
| Abnormal | 88 | 29.16 ± 10.22 | ||
| Chemotherapy, (n=347) | 2.779 | 0.006 | ||
| Yes | 9 | 37.33 ± 10.47 | ||
| No | 338 | 28.88 ± 8.97 | ||
| Radiotherapy, (n=347) | 3.208 | 0.001 | ||
| Yes | 31 | 34.03 ± 10.16 | ||
| No | 316 | 28.61 ± 8.85 | ||
| Medical payment method, (n=347) | 1.638 | 0.196 | ||
| Own expense | 22 | 30.86 ± 10.51 | ||
| Public expense | 39 | 26.87 ± 8.54 | ||
| Medical insurance | 286 | 29.27 ± 9.09 | ||
| Health hope index, (n=347) | 6.018 | 0.015 | ||
| Low (12-23) | 160 | 27.81 ± 9.761 | ||
| Medium (24-35) | 187 | 30.20 ± 8.35 | ||
| High (36-48) | 0 |
Table 2: Comparison of fear of illness scores between sociodemographic and clinical characteristics (t test/analysis of variance)
Multivariate linear regression analysis of risk factors of FCR in patients with NSCLC
Statistical methods were used to further study the relationship between sociodemographic and clinical variables and FCR in patients with NSCLC to determine the independent predictors of FCR. Values were assigned to all variables, and the information summary after the assignment is shown in Table 3.
| Variable | Coding |
|---|---|
| Gender | 1=Male, 2=Female |
| Age | 1=18-35, 2=36-60, 3=>60 |
| Ethnicity | 1=Han nationality, 2=Ethnic minorities |
| Education level | 1=Junior high school or below, 2=High school graduate, 3=College graduate or above |
| Marital status | 1=Unmarried, 2=Married, 3=Divorced |
| Monthly income | 1 ≤ 3000, 2=3000-5000, 3=5001-10000, 4 ≥ 10000 |
| Place of residence | 1=City, 2=Villages and towns, 3=Rural |
| Living alone | 1=Yes, 2=No |
| Smoking | 1=Yes, 2=No |
| Family history | 1=Yes, 2=No |
| Combined with the underlying disease | 1=Yes, 2=No |
| Course classification | 1=0-12month, 2=13-36month, 3 ≥ 36month |
| Number of lesions | 1=Single, 2=Multiple |
| T | 0=T0, 1=T1, 2=T2, 3=T3, 4=T4 |
| N | 0=N0, 1=N1, 2=N2, 3=N3 |
| Preoperative tumor indicators | 1=Normal, 2=Abnormal |
| Chemotherapy | 1=Yes, 2=No |
| Radiotherapy | 1=Yes, 2=No |
| Medical payment method | 1=Own expense, 2=Public expense, 3=Medical insurance |
| Fear of progression | 0=12-33, 1=34-60 |
| Social support rating scale | 1=Yes, 2=No |
| Herth hope index | 1=12-23, 2=24-35, 3=36~48 |
Table 3: Coding of categorical variable
The maximum likelihood method was used to determine the predictive effect of each variable on FCR. The calibration ability of the prediction model was evaluated by the Hosmer- Lemeshow goodness of fit test. P=0.72>0.05, indicating no statistically significant difference between the predicted value of the model and the actual observed value. The results showed a high calibration ability of the prediction model. According to the outcomes of univariate logistic regression, the difference was significant. After adjusting the relevant covariates and controlling the confounding factors, the results of multivariate adjustment of logistic regression showed that:
• The risk of fear of relapse in female patients was 2.81 times higher than that in male patients or (95 % CI): 2.81 (1.354, 5.825), p<0.01.
• The risk of fear of disease in patients with ethnic minorities was about 35.09 times that of Han patients, or (95 % CI): 35.09 (4.05, 303.86), p<0.001.
• The risk of fear of disease in patients with a monthly income of 5001-10000 yuan is about 0.008 times that of patients with a monthly income of <3000 yuan, or (95 % CI): 0.008 (0.001, 0.125) p<0.001.
• The risk of disease fear in patients with moderate hope level was about 2.022 times that in patients with mild hope level, or (95 % CI): 2.022 (1.044, 3.916), p<0.05 (Table 4).
| Variable | CrudeOR (95%CI) | p value | Adjusted for | Adjusted OR (95%CI) | p value |
|---|---|---|---|---|---|
| Gender, (n=347) | Age, ethnicity, monthly income, chemotherapy, radiotherapy, family history | ||||
| Male (Ref.) | - | - | - | - | |
| Female | 1.752 (1.059, 2.898) | 0.029 | 2.808 (1.354, 5.825) | 0.006 | |
| Age, year, (n=347) | Gender, ethnicity, monthly income, chemotherapy, radiotherapy, family history | ||||
| 18-35, year (Ref.) | - | - | - | - | |
| 36-60, year | 0.781 (0.357, 1.708) | 0.536 | 1.059 (0.384, 2.920) | 0.913 | |
| >60, year | 0.115 (0.040, 0.333) | 0.000 | 0.000 | 0.994 | |
| Ethnicity, (n=347) | Gender, age, monthly income, family history, chemotherapy, radiotherapy, | ||||
| Han nationality (Ref.) | - | - | - | - | |
| Ethnic minorities | 2.377 (1.096, 5.156) | 0.028 | 35.093 (4.053,303.862) | <0.001 | |
| Education level, (n=347) | Gender, age, ethnicity, marital status | ||||
| Junior high school or below (Ref.) | - | - | - | - | |
| High school graduate | 1.494 (0.684, 3.264) | 0.314 | 2.920 (0.669, 6.555) | 0.204 | |
| College graduate or above | 1.735 (0.915, 3.288) | 0.091 | 2.920 (0.968, 8.813) | 0.057 | |
| Marital status, (n=347) | Gender, age, ethnicity, education level | ||||
| Unmarried (Ref.) | - | - | - | - | |
| Married | 0.737 (0.245, 2.218) | 0.588 | 2.006 (0.376, 10.698) | 0.415 | |
| Divorced | 0.571 (0.085, 3.833) | 0.564 | 2.396 (0.182, 31.576) | 0.507 | |
| Monthly income, (n=347) | Gender, age, ethnicity, family history, chemotherapy, radiotherapy | ||||
| <3000, yuan (Ref.) | - | - | - | - | |
| 3000-5000, yuan | 1.572 (0.816, 3.028) | 0.177 | 2.527 (.974, 6.557) | 0.057 | |
| 5001-10000, yuan | 0.109 (0.035, 0.341) | <0.001 | 0.008 (0.001, 0.125) | 0.001 | |
| >10000, yuan | 1.143 (0.540, 2.416) | 0.727 | 0.922 (0.307, 2.775) | 0.886 | |
| Place of residence, (n=347) | Gender, age, ethnicity, marital status | ||||
| City (Ref.) | - | - | - | - | |
| Villages and towns | 3.224 (0.879, 11.826) | 0.077 | 1.223 (0.213, 7.027) | 0.822 | |
| Rural | 1.846 (0.522, 6.527) | 0.341 | 0.940 (0.164, 5.401) | 0.945 | |
| Living alone, (n=347) | Gender, age, preoperative tumour indicators | ||||
| Yes (Ref.) | - | - | - | - | |
| No | 0.866 (0.514, 1.460) | 0.590 | 0.718 (0.388, 1.329) | 0.292 | |
| Smoking, (n=347) | Gender, age, ethnicity, education level | ||||
| Yes (Ref.) | - | - | - | - | |
| No | 1.202 (0.636, 2.271) | 0.572 | 0.466 (0.162, 1.336) | 0.155 | |
| Family history, (n=347) | Gender, age, ethnicity, monthly income, family history, chemotherapy, radiotherapy | ||||
| Yes (Ref.) | - | - | - | - | |
| No | 0.758 (0.460, 1.248) | 0.276 | 0.630 (0.340, 1.170) | 0.143 | |
| Combined with the underlying disease, (n=347) | Gender, age, family history, chemotherapy, radiotherapy | ||||
| Yes (Ref.) | - | - | - | - | |
| No | 1.323 (0.790, 2.218) | 0.287 | 1.339 (0.659, 2.720) | 0.420 | |
| Course classification, (n=347) | Gender, age, ethnicity, family history | ||||
| 0-12, month (Ref.) | - | - | - | - | |
| 13-36, month | 1.414 (0.734, 2.722) | 0.300 | 0.825 (0.367, 1.852) | 0.641 | |
| >36, month | 1.570 (0.603, 4.090) | 0.356 | 1.312 (0.340, 5.068) | 0.694 | |
| Number of lesions, (n=347) | Gender, age, ethnicity, family history | ||||
| Single (Ref.) | - | - | - | - | |
| Multiple | 1.102 (0.686, 1.771) | 0.688 | 0.826 (0.428, 1.596) | 0.570 | |
| T, (n=347) | Gender, age, ethnicity, chemotherapy, radiotherapy | ||||
| T0 (Ref.) | - | - | - | - | |
| T1 | 0.471 (0.202, 1.096) | 0.080 | 0.808 (0.281, 2.329) | 0.694 | |
| T2 | 2.554 (0.505, 12.911) | 0.257 | 8.025 (0.975, 66.071) | 0.053 | |
| T3 | 4126273147 (0) | 1.000 | 270497179179 (0) | 0.999 | |
| N, (n=347) | Gender, Age, Ethnicity, Chemotherapy, Radiotherapy | ||||
| N0 (Ref.) | - | - | - | - | |
| N1 | 1.135 (0.287, 4.486) | 0.857 | 1.121 (0.091, 13.787) | 0.929 | |
| N2 | 0.611 (0.170, 2.196) | 0.450 | 1.876 (0.212, 16.621) | 0.572 | |
| Preoperative tumor indicators, (n=285) | Gender, age | ||||
| Normal (Ref.) | - | - | - | - | |
| Abnormal | 1.231 (0.694, 2.185) | 0.478 | 1.959 (0.032, 8.719) | 0.540 | |
| Chemotherapy, (n=347) | Gender, age, ethnicity, family history | ||||
| Yes (Ref.) | - | - | - | - | |
| No | 0.477 (0.224, 1.017) | 0.055 | 0.367 (0.072, 1.869) | 0.227 | |
| Radiotherapy, (n=347) | Gender, age, ethnicity, family history | ||||
| Yes (Ref.) | - | - | - | - | |
| No | 0.176 (0.043, 0.719) | 0.016 | 0.000 | 0.993 | |
| Medical payment method, (n=347) | Gender, age, ethnicity, family history | ||||
| Own expense (Ref.) | - | - | - | - | |
| Public expense | 0.525 (0.167, 1.649) | 0.270 | 1.224 (0.292, 5.124) | 0.782 | |
| Medical insurance | 0.645 (0.260, 1.597) | 0.343 | 1.101 (0.354, 3.423) | 0.868 | |
| Health hope index, (n=347) | Gender, age, ethnicity, family history | ||||
| Low (12-23) (Ref.) | - | - | - | - | |
| Middle (24-35) | 1.646 (1.013, 2.675) | 0.044 | 2.022 (1.044, 3.916) | 0.037 |
Table 4: Logistic regression model analysis of influencing factors of disease fear.
Establishment of a risk prediction model for FCR
Construction of prediction model: According to logistic regression, an equation was established to identify meaningful variables. The risk prediction model of FCR of early NSCLC patients in this study was established as follows: The final model logit(P)=-1.033* gender-3.558* nationality+1.008* monthly income (3000-5000)-4.723* monthly income (5000-10000)- 0.704* total hope score. The equation was used for prediction for FCR. If the predictive value was greater than 0.5, the patients were expected to suffer from psychological imbalance. If it was less than 0.5, the patients were expected to not suffer from psychological imbalance.
Predictive value of prediction model for FCR of patients with early NSCLC
The AUC of the risk prediction model for fear of cancer progression in individuals with early NSCLC constructed in this study is 0.891 (95% CI: 0.858-0.924), P<0.001, and the diagnostic model had a high degree of differentiation. Figure 1, shows that the coordinates of the point closest to the upper left of the coordinate map were 0.751 and 0.894 for specificity and sensitivity, respectively, i.e., at this tangent point, the sensitivity and specificity of the model were both maximum, and the Youden index was also the maximum.
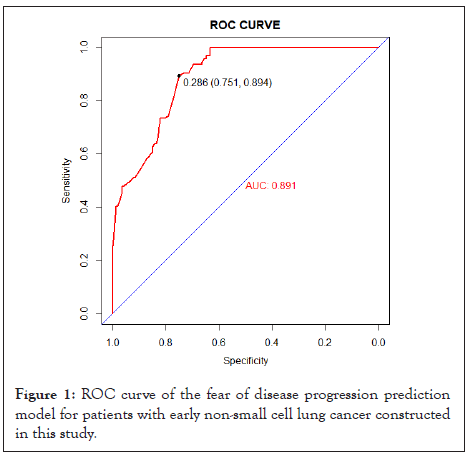
Figure 1: ROC curve of the fear of disease progression prediction model for patients with early non-small cell lung cancer constructed in this study.
The univariate results showed statistically significant differences in FCR scores among NSCLC patients of different ages, education levels, family per capita monthly income, residence, whether they had received chemo and radiotherapies, and hope levels (p<0.05). Among them, the per capita monthly income and hope levels of families were included in the final regression equation. Therefore, the age, education level, residence and whether they underwent radiotherapy and chemotherapy were not included in the regression equation as discussed here.
This study showed significant differences in the total score of FCR among patients of different ages (P<0.05). The younger the patient, the higher the degree of FCR, which was accordant with the findings of Sun H, et al. [22]. This might be due to the different lifestyles at different ages. For example, young patients with early NSCLC have poor psychological tolerance due to unpredictable futures, therefore, getting diagnosed with a malignant tumour breaks their life balance, including life planning, goals and work, and it is difficult to live as before, causing the patient to lose confidence in life and fear of the future. Uncertainty about the disease or treatment effect leads to increased psychological distress. Dave also pointed out that age is an important independent factor that affects the FCR of cancer patients [23]. The younger the patients, the greater their expectation of the expected survival period and the more they worry about the future, the more serious their FCR.
This study showed that the total FCR scores of individuals with different levels of education were significantly different (P<0.05). The higher the education level, the more serious the FCR of the patients, which is accordant with the research findings of Lin Shuaishuai, et al. on 118 patients with nasopharyngeal carcinoma undergoing radiotherapy [24]. The reasons might be that the higher the education level, the easier it is to understand the disease occurrence, development and final process through various sources, and the more likely it is to worry about the recurrence or metastasis of cancer, resulting in a more serious FCR. This study contradicts the results reported in some foreign studies on cancer survivors. Therefore, healthcare professionals should be more attentive to these individuals and explain the progress of the disease and the current advanced technologies along with multiple treatment methods to patients in an easy-to- understand language to reduce their anxiety and psychological effect of FCR. The FCR level of patients living in villages and towns is the highest. This might be due to the rapid development of the national economy, culture and medical treatment that has made most countries or towns develop relatively fast. The residents have greatly improved conditions in all aspects, received more knowledge about cancer, and their per capita income has also increased. Improving medical conditions has prompted residents to pay special attention to their health. Therefore, the degree of FCR is more serious after knowing the tumour.
This study showed a significant difference in the total FCR scores of patients who have received or have not received chemotherapy and radiotherapy (P<0.05). The degree of FCR in patients who received radiotherapy or chemotherapy before surgery was higher than that in individuals who did not receive treatment, which is accordant with prior research findings [25]. The theoretical model of FCR emphasizes the triggering effect of medical investigation and exposure to cancer hints and the continuous impact of frequent inspection, seeking comfort and long-term belief in disease. Personal factors, such as psychological vulnerability and cognitive style, play a role in the development and persistence of severe FCR. The iatrogenic factors related to new cancer treatment may also lead to FCR. The development of NSCLC treatment methods, such as radiotherapy, chemotherapy, targeted therapy, immunotherapy and other measures, has extended the duration of treatment. Evaluation criteria have changed compared to traditional treatment methods such as surgery, radiotherapy, and chemotherapy. The evaluation time is lengthening along with the survival period of patients. These factors have exacerbated fear and uncertainty [24]. The effect monitoring after radiotherapy and chemotherapy and the recurrence signs related to the new therapy, as well as the increase of information to predict individual treatment response or recurrence risk, have increased the FCR of patients [26]. This further suggests that healthcare personnel should be more attentive to these individuals, encourage doctors and nurses to understand FCR, and study the potential role of long-term treatment, close monitoring and provide personalized information about disease recurrence risk, encourage patients and their families to also understand FCR and receive psychological education and comfort which is conducive to improving the doctor-patient relationship ultimately benefiting patients.
The outcomes of this research highlighted that the FCR level of female patients was higher, which is consistent with the research conclusion of Zhang Chengbin [27]. The FCR level of female patients facing unpredictable futures is higher than that of men. Foreign studies have also pointed out that women show a higher degree of FCR than men [28]. The reasons may be that individual behaviour is affected by psychological, physiological and social factors. Considering that women shoulder multiple pressures in life, such as taking care of family and work simultaneously, their FCR levels are higher than men. In addition, as women are relatively more vulnerable than men, their psychological pressure is far greater than that of men in terms of changes in appearance and role loss caused by cancer treatment. Other studies have shown that women are more likely to be emotional [29]. Behavioural research shows that women score higher than men on the scale of negative emotional experiences [30]. When women are diagnosed with cancer, they may suffer from a mental breakdown and be afraid of failing to take good care of their families due to their reduced working ability after treatment [31]. This suggests that medical personnel should pay special attention to women, adopt different ways of comfort and guidance according to their different personalities and physiques, and formulate scientific and reasonable nursing measures for women patients. We can also guide female patients from the family perspective, mobilize a stronger social support system, and encourage patients to establish confidence in overcoming the disease.
The results of this study showed that the FCR of ethnic minority patients was higher than that of Han people, which may be related to the cultural background, religious beliefs and ethnic differences of ethnic minorities. Medical staff should give targeted guidance according to the national culture and religious beliefs of different patients, which also requires medical staff to know more about the cultures of different nationalities and religions at ordinary times, to better understand their psychology and take practical guidance measures to help patients reduce the level of FCR.
The results of this study showed that patients with average family income per month at a low or medium level have a higher level of FCR because they can't afford medical expenses. They worry that the recurrence will further increase the family's economic burden, affecting their living standard. This leads to guilt for using the family's resources [32]. Research data shows that the economic burden of lung cancer and gastric cancer patients is US $9970 per capita [33]. Given the national conditions of developing countries and the huge population, the Chinese government's medical investment proportion is lower than that of most countries in the world. Due to insufficient government investment, the high cost of medical care eventually transfers to individuals, society and medical institutions. Although the economic burden of patients with different types of cancer differs from their average annual family income, the economic burden of the disease is extremely heavy. Secondly, although the number of people undergoing physical examination in China is increasing yearly, there is still a big gap compared with the coverage rate of nearly 90% in some developed countries [34]. A survey shows that the health awareness level of Chinese residents needs to be improved. For people with low and middle income, their awareness of disease screening, physical examination and other disease prevention is relatively low [35]. NSCLC grows slowly; most early lung cancer can be found through physical examination, such as computed tomography. However, because of their limited income level, these people are unwilling to pay for health examinations themselves. It may be that lung cancer is in the middle and advanced stages when it is detected, and the best stage of radical surgery has been missed. In the end, people's desire for survival will force patients and their families to seek all kinds of methods in the hope of possible miracles, and the cost of these methods is often huge. A study on NSCLC shows that the average medical cost of Chinese patients with NSCLC in the last three months is about US $16955. Even if some of them can be reimbursed by medical insurance, it is unaffordable for most Chinese families [36]. Therefore, under the influence of many factors such as treatment means, survival period, prognosis and treatment cost, the disease fear level of the Chinese population is higher.
The results of this study showed that the FCR of patients with moderate hope levels was higher than that of patients with low hope levels. The risk of disease fear in patients with moderate hope level was about 2.022 times that in patients with mild hope level, or (95% CI): 2.022 (1.044, 3.916), P<0.05. It might be due to a large number of patients in the medium hope level in the sample size. Hope theory points out that hope, as the main concept of positive psychology, helps individuals maximize their potential by studying people's positive psychological capital and positive power [37], improving their hope index, helping eliminate negative emotions, improving self-acceptance and confidence in overcoming diseases. Hope has become a new nursing goal and rehabilitation concept in the modern bio-psycho-social medical model. Hope theory has been applied to clinical nursing [38]. Snyder's hope theory highlights that hope is a basic dynamic state based on interaction. In nursing practice, it can lead patients to see hope, establish positive goals, face diseases with positive attitudes, and promote rehabilitation. In previous studies, the beliefs and motivations of patients have not been used to assess the relapse fear of lung cancer patients. Therefore, this study found that hope level can be used as an independent predictor of FCR of early NSCLC patients. This study suggested that the hope level can be included in future assessments. The risk of FCR can be more completely identified by assessing the positive internal beliefs of individuals, which can help medical staff formulate better intervention strategies. Make full use of the guiding role of hope theory to guide patients positively, eliminate negative emotions in patients, make patients hopeful for the future, and improve their self-acceptance and confidence in overcoming diseases.
Based on cross-sectional survey data analysis, this study preliminarily constructed a risk prediction model for early NSCLC patients with FCR. The AUC is 0.891 (95% CI: 0.858- 0.924), the sensitivity is 0.894, and the specificity is 0.751, which reflects that this model is operable as it can better identify patients with early NSCLC patients and high levels of FCR. A total of 19 risk factors were included in this study for the final investigation. Gender, nationality, per capita monthly income of families and hope levels were identified as predictors of FCR. Finally, a prediction model was developed.
Simultaneously, the corresponding risk scores were objectively calculated after the value of each prediction factor was added to the prediction algorithm. Most FCR patients with clinically significant levels can be identified early and accurately and benefit more from psychological intervention. Therefore, this prediction algorithm has great potential to evaluate the effect of FCR intervention programs aimed at reducing early NSCLC patients by predicting FCR. This prediction model is suitable for nurses to evaluate the FCR levels of NSCLC patients in the early outpatient period and patients after surgery and for community nurses to evaluate the FCR levels of follow-up cancer patients. Medical staff can use the risk prediction model to timely find patients with psychological disorders caused by excessive fear according to the actual situation of patients, timely carry out prevention and provide personalized nursing intervention to reduce the fear of patients, thus enhancing their confidence in overcoming diseases and improving their quality of life. However, the study shows that patients with cancer and advanced tumour in the chemotherapy period have a high fear of progression, and they need to be evaluated during the hospital treatment period. The prediction model in this study has only reference value to evaluate the results of these people. In the later stage, the research samples should be further expanded, verified, revised, and applied to the expanded population. Simultaneously, the influencing factors included in the model built in this research need to be widened to further verify the accuracy of its evaluation. As an auxiliary tool, clinicians can integrate predictive models into clinical practice and patient management based on their judgments and preferences.
There is no risk prediction model for FCR of early NSCLC patients China and other countries. This study systematically analysed the influencing factors of FCR of early NSCLC patients and preliminarily constructed a targeted risk prediction model to help doctors and nurses identify the high FCR level of early NSCLC patients and provide tools and a scientific basis for their prevention and intervention. Through the univariate and multivariate logistic regression analyses on the social demography, clinical variable data and hope levels of patients with early NSCLC, this study found the FCR levels and related influencing factors and constructed a risk prediction model. The results were as follows: Gender, nationality, per capita monthly income and hope level acted as independent influencing factors of FCR. However, more variables can be included in the prediction model in the following research. This model has significance for identifying high-risk groups and predicting the level of FCR and provides a new reference method for clinical evaluation. This study also has its limitations. First, although 19 sociodemographic and clinical factors have been considered, fear can be assessed through various complex questionnaires. Secondly, only a single centre sample is selected for the survey scope, and a multicentre, large sample sampling survey method can be conducted in the future to increase the representativeness of the sample and reduce bias; This study is a cross-sectional study to explore the influencing factors of FCR in early NSCLC patients. In the future, more research methods such as longitudinal research and qualitative interview will be further used to explore the psychology of FCR in early NSCLC patients, to provide further guidance for clinical intervention. The risk prediction model for fear of disease progression level of early lung cancer patients initially constructed in this study is limited by time and should be further verified, revised and applied in subsequent studies.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar][PubMed] .
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Schoral] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Liu M, Liu L, Lv Z (2024) A Cross-Sectional Study on the Prediction Model of Fear of Cancer Recurrence in Individuals with Non-Small Cell Lung Cancer. J Psychol Psychother.14:480.
Received: 30-Apr-2024, Manuscript No. JPPT-24-31012; Editor assigned: 03-May-2024, Pre QC No. JPPT-24-31012 (PQ); Reviewed: 17-May-2024, QC No. JPPT-24-31012; Revised: 24-May-2024, Manuscript No. JPPT-24-31012 (R); Published: 31-May-2024 , DOI: 10.35841/2161-0487.24.14.480
Copyright: © 2024 Liu M, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.