Journal of Clinical & Experimental Dermatology Research
Open Access
ISSN: 2155-9554
ISSN: 2155-9554
Case Report - (2019)Volume 10, Issue 2
We report a 16-month-old black girl received at emergency with a history of generalized and itchy bullous and post-bullous eruption occurred 24 hours after administrating ibuprofen for acute otitis. The diagnosis of bullous toxidermia was retained and the evolution was quickly favorable. She was seen seventy-two hours after leaving hospital for pruritic papulo-vesiculo-bullae located on the head, face, necklines, buttocks, perineum and legs after eating crustacean on the day before. The biopsy of a papulo-bullae lesion led to (after the different stains (hematoxylin, Giemsa, toluidine blue) corroborating with immunohistochemical typing with anti CD117) the diagnosis of bullous cutaneous mastocytosis.
Bullous mastocytosis; Bullous dermatoses; Childhood; Mast cells; Tryptase
Mastocytosis is a heterogeneous group of disorders characterized by the abnormal accumulation or proliferation of mast cells in one or more organs. The target organ most often concerned is the skin [1-5].
Mastocytosis affects children in almost two thirds of cases. In 90% of childhood cases, it is a pure skin attack in the form of pigmentary urticaria (65%), or solitary mastocytoma (10-35%). It is also possible to have a diffuse mastocytosis with a lower incidence (1-8%), the bullous form of which is the most frequent, and observed in 62-66% of cases [2,4,6,7].
Many factors such as drugs, histamine-rich-food or histaminoliberators food, can cause mast cell degranulation responsible for that symptomatology [2,4,6,8]. We report a case of diffuse cutaneous mastocytosis in its bullous form which simulates a bullous toxidermia in a black infant.
A 16-month-old black girl with a history of allergic rhinitis was received at emergency hospitalization for large, very itchy bullae and post-bullous erosions. The little girl was reported to be the only child of a non-consanguineous parent. Her pregnancy, childbirth and developmental history were said to have gone well. The bullous detachments were reported to have occurred 24 hours after she was administered ibuprofen for acute otitis.
The physical examination found in a very irritable infant, 1-4 cm, clear, brittle blisters with very large and oozing post-bullous erosions. The lesions were located on the face, the front, the back necklines, the abdomen, the labia majora, the inguinal folds and the buttocks. There was no damage to the mucous membranes, palms or plants (Figure 1). The rest of the physical examination was unremarkable. The clinical diagnosis of bullous toxidermia attributable to ibuprofen was retained. The evolution was quickly favorable in one week under symptomatic treatment. The evolution was quickly favorable under a treatment made of chlorhexidine solution bath, 2% aqueous eosin wash, mequitazine syrup.
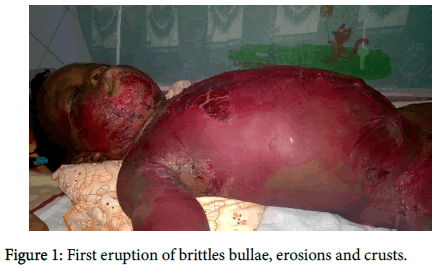
Figure 1. First eruption of brittles bullae, erosions and crusts.
Seventy-two hours after leaving hospital, she was seen in consultation for intense pruritus inducing insomnia, causing fluid lesions. This time, there was no prior drug intake, but rather crustacean consumption on the day before. The physical examination found a patient in good general condition, with vesiculo-bullae showing clear content, with an urticarial base, some of which are eroded (Figure 2). These lesions were located on the head, the face, the necklines, the buttocks, the perineum and the legs in a roughly symmetrical manner. Koëbner's phenomenon was noted on the right leg. The mucous membranes, the palms and the plants were unharmed. There was no hepatosplenomegaly. The rest of the physical examination was normal.

Figure 2. Second eruption of papulo-vesiculo-bullae on the face, neck and back necklines.
The following hypotheses were put forward: acute eczema, bullous cutaneous lichen and bullous mastocytosis. The biopsy of a papulobullous lesion was performed. It showed after the different stains (Hematoxylin Eosin, Giemsa and Toluidine blue) epidermolysis, a peri-capillary mononuclear infiltrate with a predominance of mast cells in the superficial dermis. Immunohistochemical typing with anti CD117 was positive (Figures 3-7). A hypereosinophilia with 1800 cells/mm3 was found at the blood count. The liver test was normal. The diagnosis of the bullous form of diffuse cutaneous mastocytosis was retained. There was no clinical sign pointing to systemic attack. Tryptasemia was 17 ng/mL (standard<15 ng/mL). The mutation of the c-kit receptor was not sought because the parents lacked money.
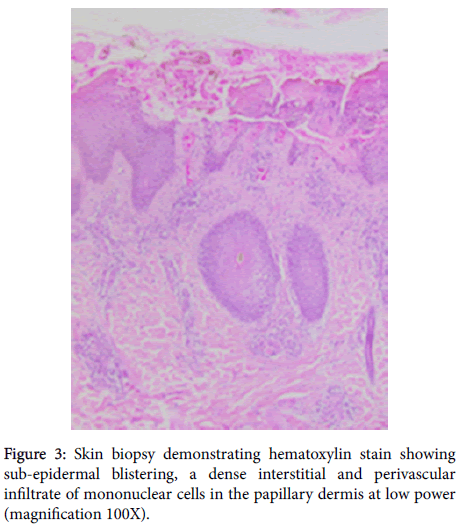
Figure 3. Skin biopsy demonstrating hematoxylin stain showing sub-epidermal blistering, a dense interstitial and perivascular infiltrate of mononuclear cells in the papillary dermis at low power (magnification 100X).
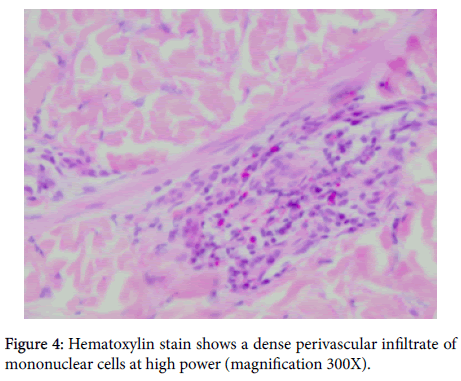
Figure 4. Hematoxylin stain shows a dense perivascular infiltrate of mononuclear cells at high power (magnification 300X).
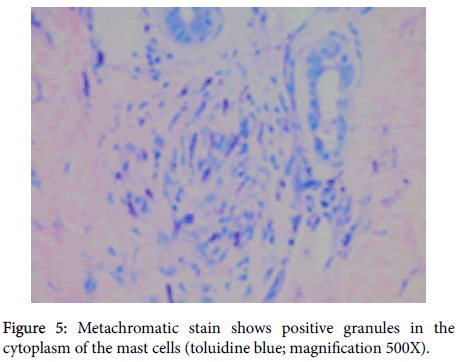
Figure 5. Metachromatic stain shows positive granules in the cytoplasm of the mast cells (toluidine blue; magnification 500X).
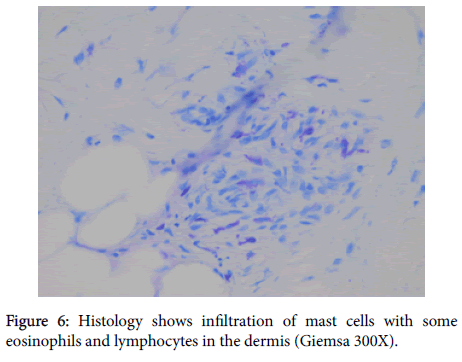
Figure 6. Histology shows infiltration of mast cells with some eosinophils and lymphocytes in the dermis (Giemsa 300X).
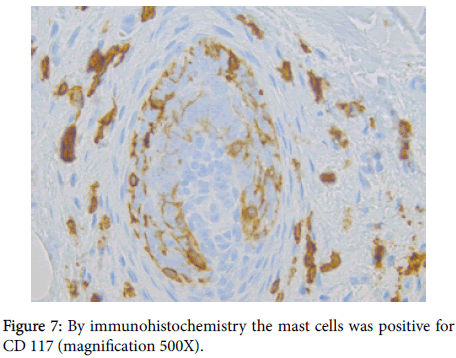
Figure 7. By immunohistochemistry the mast cells was positive for CD 117 (magnification 500X).
Complete disappearance of the lesions was obtained in 2 weeks with the general corticosteroid therapy (Betametasone: 1 mg/kg/day) associated with Ketotifen and hydroxyzine. The decreasing dose of oral corticosteroid was performed over 6 weeks without any side effects. An eviction list of triggers was given to her parents. The parents have been also instructed on the use of an anaphylaxis emergency kit including bexamethasone syrup and an epinephrine autoinjector pen in case of hemodynamic shock.
After one year of follow-up, two small eruptions were observed, leaving pruritic papulo-bullous lesions on her legs. The first episode followed the consumption of peas and the second followed citrus consumption.
Mastocytosis is a rare disease in children that occurs in the majority of cases before the age of 2 years. Neonatal forms are rare [2,3,6,8-11]. It results most often from a mutation of the c-Kit receptor, present in children in about 86% of cases. This mutation induces the proliferation and activation of mast cells in the connective tissue, as well as the release of mediators, such as histamine and tryptase. Rare familial forms exist with dominant autosomal transmission and variable penetrance [3,5,8,12].
Early manifestations may appear as infiltrated skin with a pasty consistency, sometimes giving a "peau d'orange" or "peau chagrine" appearance. It can be associated with nodular lesions, urticarial papules. Pruritus is most often severe and is found in 80% of patients. Diffuse cutaneous mastocytosis may induce extensive bullous detachments. In that case, the bullae are the primous cutaneous sign. They usually have a clear content and are arranged linearly (by Köbner phenomenon) or grouped in a closet on the scalp, trunk and limbs [1-3,5,9]. Briggman et al showed that the massive release of serum proteases namely chymase and cathepsin G, caused by mast cell degranulation, leads to lysis of the dermo-epidermal junction which induces bullous detachments [6]. Sometimes the contents of the bubbles can be hemorrhagic. This phenomenon is secondary to the secretion of heparin by mast cells and exposes to a higher risk of mortality [3,4,6,12].
In children with generalized bullous eruption, the risk of developing systemic disorders is higher. These manifestations are flushing, convulsions, nausea, vomiting, diarrhea, headache, dyspnea or syncope. They can be responsible for hemodynamic instability or even anaphylactic shock or sudden death. These complications related to the release of histamine, are observed even in the absence of cutaneous lesions. Gastrointestinal symptoms are present in 60 to 80% of cases depending on the series, with a risk of gastric ulcer and digestive hemorrhagies [1,2,4,6,11,12].
Biologically, the dosage of histamine is not very specific. Although it may be normal, the only dosage currently recommended is that of tryptase. In adults, tryptasemia greater than 20 ng/mL has a specificity of 98% and a sensitivity of 83 to 93% in favor of systemic involvement; however, this correlation has not been demonstrated in children. Serum tryptase is a good reflection of mast cell proliferation and especially bone marrow infiltration, but high levels can be observed in myeloid hemopathies, urticaria or during anaphylactic shock [2,4,8,11]. Histopathology plays a key role in the diagnosis [5,7]. In children, further investigations are justified only in the presence of hematological abnormalities, visceral failure or in case of diffuse cutaneous mastocytosis with signs of extra-cutaneous involvement such as lymphadenopathy, hepatosplenomegaly [1,2,4].
The lesions of cutaneous mastocytosis are caused by various stimuli including histamine-releasing drugs such as nonsteroidal antiinflammatory drugs in the case of our patient. Histamines-rich-foods such as crustaceans, peas or histamino-liberators foods such as citrus fruits can also cause lesions. Various traumatisms including surgical procedures, stress, immunological stimuli (insect bite), infections are also involved [1,2,4,6,8,9,12]. The removal of these factors is essential in the management of this disease.
Apart from the neonatal form whose prognosis is reserved, evolution is spontaneously resolving before adolescence. It may persist in adulthood with dermographism and hyperpigmentation [2-5,8,12]. This bullous form of diffuse cutaneous mastocytosis often presents a problem of differential diagnosis with other bullous dermatoses in children, such as staphylococcal scalded skin syndrome (SSSS), bullous impetigo, bullous congenital ichthyosiform erythroderma, epidermolysis bullosa, erythema multiforme or a bullous toxidermia in our case [2,4,8,10-12].
The goal of treatment is to control the symptoms of degranulation of mast cells and stop their proliferation. Management must consider the many factors that provoke mast cell degranulation with the widest possible eviction list. H1 and H2 antihistamines and local corticosteroids are used in the first intention. Ketotifen appears effective for controlling mastocytosis. Disodium cromoglycate sometimes has an effect on pruritus, diarrhea and flushing. In severe forms, it is possible to resort to systemic corticosteroid therapy or even treatment with interferon alpha or cyto-reducing therapies. In some cases, the benefit of imatinib-mesylate has been demonstrated. Antiseptics are used to prevent superinfection in case of vesicular or bullous lesions. Children should be equipped with an injectable adrenaline pen for use in case of deep hypotension or shock [2-4,6,12].
Diffuse bullous mastocytosis is an exceptional and severe form of cutaneous mastocytosis. Our clinical case shows the importance of the contributing factors in the occurrence of this disease. The diagnostic and therapeutic approach is not always easy. But we must know how to evoke a bullous mastocytosis in front of pruritic blisters associated with a dermographism. In addition to anaphylactic shock, the enlarged bullous form must also be considered an emergency and treated as such.
Citation: Bérénice D, Christiane K, Alida K, Nadège A, Alain G, Fabrice A, et al. (2019) A Diffuse Bullous Cutaneous Mastocytosis Mimicking a Bullous Toxidermia in a Black Child. J Clin Exp Dermatol Res 10: 1000486. doi:10.4172/2155-9554.1000486
Received: 27-Dec-2018 Accepted: 07-Feb-2018 Published: 20-Feb-2019
Copyright: © 2019 Bérénice D et al. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Sources of funding : GB´s PhD-project on ethical challenges and decision-making in nursing homes has been financially supported by the Norwegian Extra Foundation for Health and Rehabilitation through EXTRA funds (grant no. 2008/2/0208).