Journal of Cancer Research and Immuno-Oncology
Open Access
ISSN: 2684-1266
ISSN: 2684-1266
Case Report - (2024)Volume 10, Issue 3
Background: Anastomotic Leakage (AL) following low anterior resection remains a serious complication related to mortality and recurrence. Even several methods to prevent and treat AL have been advocated, but the rate of AL, readmission and permanent stoma remain unchanged. We propose a novel method for treating AL after radical resection of low rectal cancer.
Case description: The patient was a 36-year-old male who was referred to the department of digestive surgery of our hospital due to intermittent hematochezia for 2 years. There are no other accompanying symptoms. Physical examination yielded the following: 9-12 o’clock in the Knee-Chest (KC) position, about 5 cm from the anal verge, with soft, mobile, unclear edges, and mild tenderness with no blood staining. The patient was pathologically diagnosed as rectal adenocarcinoma before admission and staged as cT3N2M0 by Computed Tomography (CT) and Magnetic Resonance Imaging (MRI), long-term radiotherapy (25 × 45 Gy) with chemotherapy (capecitabine), was performed after four cycles of CapeOX protocol, and the patient then underwent Transanal Total Mesorectal Excision (TaTME). 15 days after the surgery, the patient was readmitted due to hematochezia which caused by AL. We applied modified Bacon operation on this patient, and successfully performed a second operation two weeks later. Given its simple operation, few complications and effective treatment, Modified Bacon can be used for remedy anastomotic leakage after TaTME.
Conclusion: We propose modified Bacon operation to deal with anastomotic leakage which provides a new strategy to treat AL after Low Anterior Resection (LAR).
Modified bacon; Anastomotic leakage; Rectal cancer; Transanal total mesorectal excision; Low anterior resection
Rectal cancer is one of the most common malignant tumors of the gastrointestinal tract in the world, which has risen substantially incidence and mortality year by year. Until recently, the standard of strategy for Locally Advanced Rectal Cancer (LARC) patients consists of preoperative Chemoradiation (CRT) followed by Total Mesorectal Excision (TME) and adjuvant chemotherapy [1,2]. Preoperative chemoradiotherapy can decrease tumor staging, increase the resection rate and anal preservation rate, and reduce the local recurrence rate after surgery [3]. Preoperative chemoradiotherapy significantly increased the risk of postoperative anastomotic leakage in rectal cancer Jiang et al. found that Preoperative chemoradiotherapy may change the collagen structure of the distal doughnut which was associated with post-operative AL [4]. Low rectal cancer often requires Miles surgery to remove the tumor, reduce the recurrence rate, and improve the overall survival rate. This procedure requires removal of the anus and permanent sigmoidostomy, which can seriously affect the patient's quality of life and mental health [5]. Therefore, a large number of anal preservation procedures have emerged. With the recent progression of minimally invasive techniques for colorectal cancer, laparoscopic TME is one of the mainstream treatment of rectal cancer [6]. Compared to open surgery, laparoscopic TME has less blood loss, lower incidence of anastomotic leakage, higher internal sphincter preservation, and fewer incision complications [7]. Long-term follow-up showed that the overall survival rate and Disease-free survival rate of laparoscopic rectal cancer surgery were similar to that of open surgery. However, for patients with large tumor volume, obesity and pelvic stenosis, routine laparoscopic surgery fails to meet the TME standard, which may lead to positive incisal margin, the possibility of tumor residual, and the possibility of early postoperative tumor recurrence. In 2010, the first TaTME procedure was performed by Sylla et al. [8]. With the development of modern surgical technology, TaTME surgery has become one of the hotspots in recent decades. More and more clinical studies have found that Ta TME surgery has shorter operation time, fewer blood loss, lower incidence of postoperative complications and better postoperative oncology outcome than that of transabdominal Laparoscopic Total Mesorectal Excision (LapTME) [9-11]. Anastomotic leakage is one of the most common and serious postoperative complications with an incidence of 6% after low anterior resection for rectal cancer [12]. At present, the data reported by studies on the incidence of AL after TaTME are inconsistent. Sun et al. found that the incidence of AL after TaTME was 26.9%, which was significantly higher than that of LapTME (3.8%) [13]. However, studies have also found no difference in the incidence of AL after TaTME compared with LapTME [14-16]. Several risk factors for AL have been previously identified and include male gender, a low anastomosis, preoperative chemoradiation, age, comorbidity, and peri-operative bleeding [17,18]. Studies found that the mortality rate of rectal cancer within 30 days after surgery due to AL was 2.6%, and about 65% of patients with AL after Anterior Resection (AR) ended up with permanent stoma [19,20]. Up to now, there is no specific treatment for anastomotic leakage after AR, and most patients receive permanent stoma, which seriously endangers the physical and mental health of patients and increases the economic burden of patients. Herein, we report a new treatment of AL after low AR, providing a new treatment procedure for the clinical treatment of AL.
Patient data
A 35-year-old male patient was admitted to The First Affiliated Hospital of Air Force Medical University on Dec. 10, 2021,due to “intermittent hematochezia for 2 years”. The patient denied diarrhea, constipation or tenesmus. Three days prior, he visited to a local hospital for treatment. Sigmoidoscope found a huge mucosal bulge of the rectum 5cm from the anal margin, occupying 1/2 of the intestinal cavity. Biopsy indicated moderately differentiated adenocarcinoma.
Physical examination revealed the following: body temperature, 36℃, pulse, 90 beats/min, breath, 18 times per minute, blood pressure 117/73 mmHg, height 170 cm, weight 75 kg. Anal digital examination revealed the following: 9-12 o’clock in the Knee-Chest (KC) position, about 5 cm from the anal verge, with soft, mobile, unclear edges, and mild tenderness with no blood staining.
Preoperative preparation
Routine laboratory examination showed that tumor markers were within the normal range; carcinoembryonic antigen was 1.35 ng/ mL, carbohydrate antigen 19-9 was <8.74 U/mL, and carbohydrate antigen 125 was 8.68 U/mL. Computed Tomography (CT) and Magnetic Resonance Imaging (MRI) found a mass in the middle of rectum with several metastatic lymph nodes (Figures 1A-1D). The preoperative diagnosis was cT3N2M0 rectal cancer, according to the TNM classification. Further colonoscopy results suggested that a large mucosal uplift was observed 5 cm from the anal verge which was marked with titanium clamps (Figure 1E). Biopsy indicated moderately differentiated adenocarcinoma (Figure 1F).
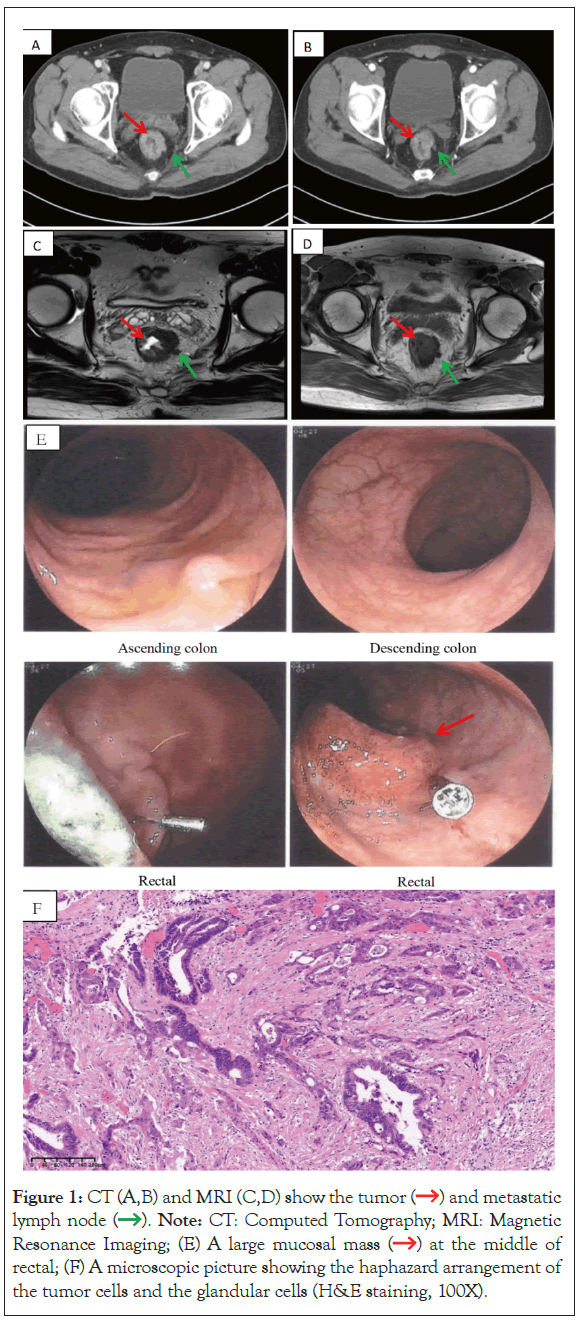
Figure 1: CT (A,B) and MRI (C,D) show the  and metastatic
lymph
and metastatic
lymph  . Note: CT: Computed Tomography; MRI: Magnetic
Resonance Imaging; (E) A large mucosal
. Note: CT: Computed Tomography; MRI: Magnetic
Resonance Imaging; (E) A large mucosal  at the middle of
rectal; (F) A microscopic picture showing the haphazard arrangement of
the tumor cells and the glandular cells (H&E staining, 100X).
at the middle of
rectal; (F) A microscopic picture showing the haphazard arrangement of
the tumor cells and the glandular cells (H&E staining, 100X).
Treatment
Reported data of Locally Advanced Rectal Cancer (LARC) showed a higher likelihood of Pathologic Complete Response (pCR) rate with Total Neoadjuvant Therapy (TNT). We therefore decided within our multidisciplinary team (MDT) to apply TNT strategy to this patient. After 4 cycles of CapeOX regimen, the patient underwent long-term radiotherapy (25 × 50 Gy) with chemotherapy (capecitabine) 6 weeks after chemoradiotherapy, routine preoperative examination showed that the tumor significantly reduced (Figure 2). The patient was admitted to our hospital on May 9, 2022. On May 10, 2022, the patient underwent laparoscopic TaTME with Preventive ileostomy (Figure 3). The patient was discharged on the 9th day after surgery.
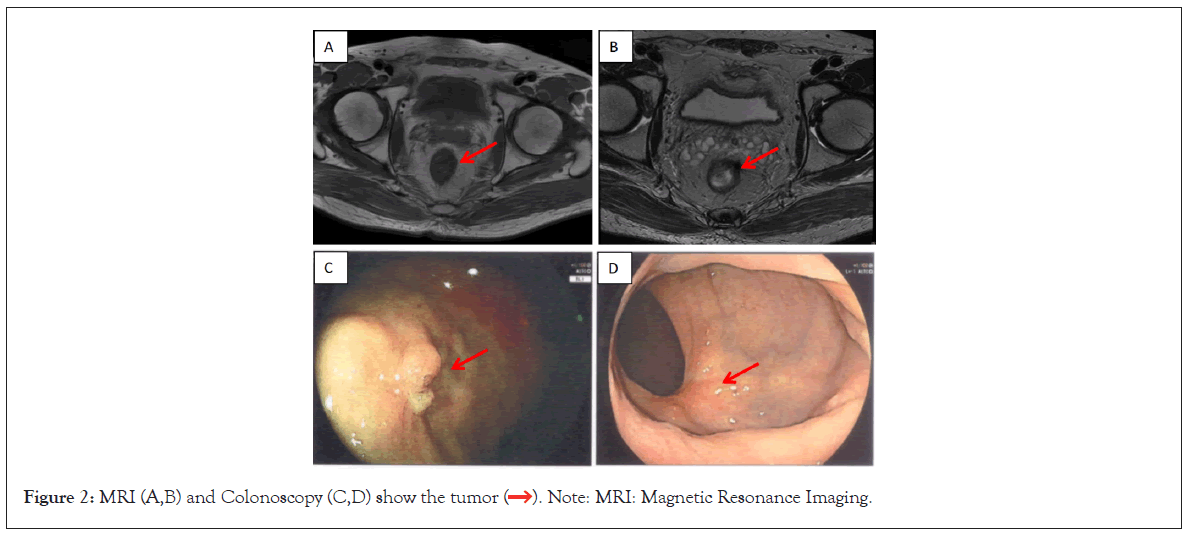
Figure 2: MRI (A,B) and Colonoscopy (C,D) show the  . Note: MRI: Magnetic Resonance Imaging.
. Note: MRI: Magnetic Resonance Imaging.
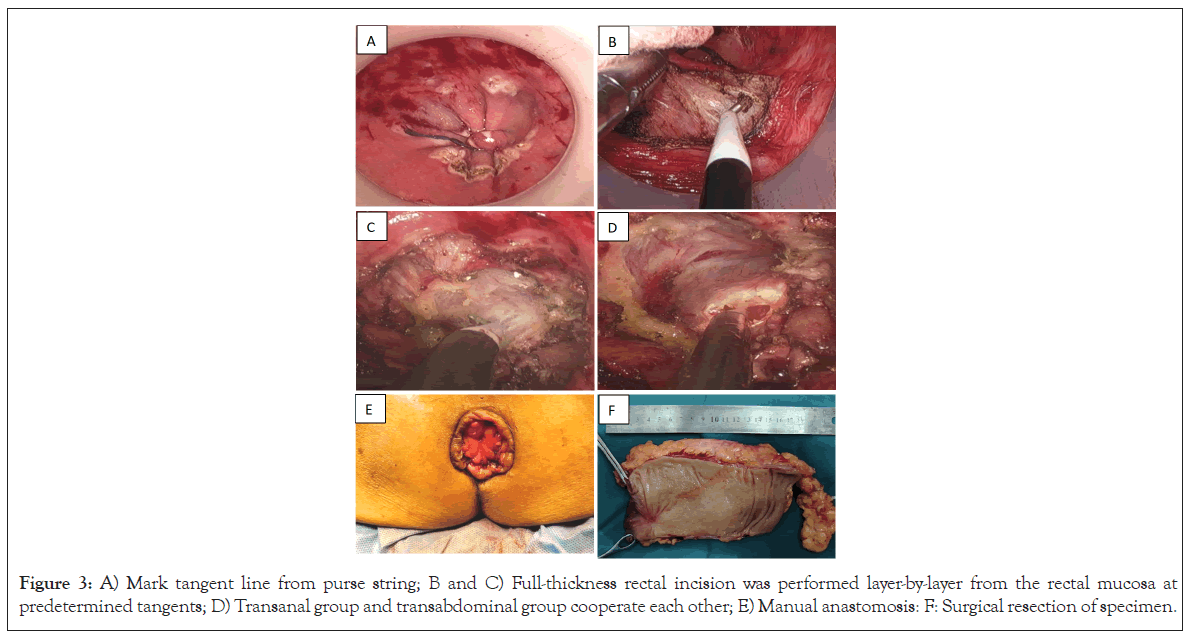
Figure 3: A) Mark tangent line from purse string; B and C) Full-thickness rectal incision was performed layer-by-layer from the rectal mucosa at predetermined tangents; D) Transanal group and transabdominal group cooperate each other; E) Manual anastomosis: F: Surgical resection of specimen.
Two weeks after surgery, the patient was readmitted with hematochezia. Anal digital examination found as follow. In the KC position, the anastomosis could be reached 2 cm away from the anus, and the anterior wall of the anastomosis could reach a defect about 1 cm in length, fresh blood flow could be seen after the withdrawal of the finger. Therefore we inferred that hematochezia was caused by AL. Transanal water-soluble radiography revealed the extravasation of contrast medium through the anastomosis, and AL was considered (Figure 4A). Numerous studies have found that anastomotic leakage may lead to permanent stoma. Given that modified bacon has fewer postoperative complications and good anal function, we decided to perform Bacon procedure on this patient. On May 26, 2022, the patient underwent ileostomy restoration and laparoscopic Bacon surgery (The splenic flexure of the colon was mobilized, and the descending colon was extruded out of the anus and fixed with 6-8 stitches of interrupted suture at the anus mucosa) (Figure 4B). The external colon was cut off at 1 cm below the dentate line 3 weeks after surgery (Figures 4C and 4D).
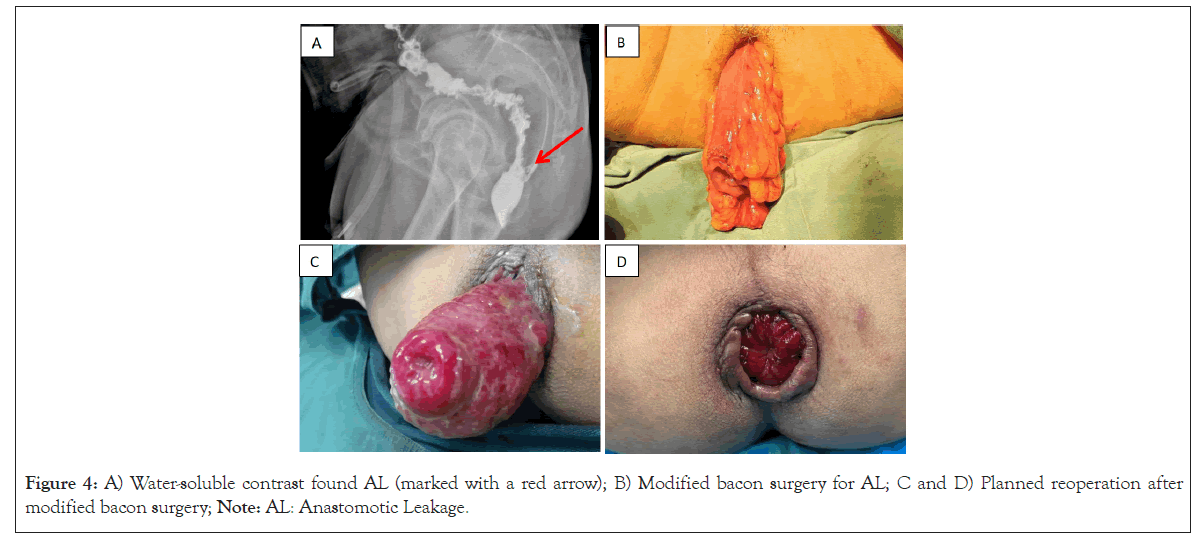
Figure 4: A) Water-soluble contrast found AL (marked with a red arrow); B) Modified bacon surgery for AL; C and D) Planned reoperation after modified bacon surgery; Note: AL: Anastomotic Leakage.
Follow-up
The patient was followed up by outpatient service 1 month and 3 months after surgery and once every 3 months after that, and a digital rectal examination was carried out. No evidence of tumor recurrence was found during follow-up. The patient was suffered from mild Low Anterior Resection Syndrome (LARS) after surgery.
AL is one of the most feared complications after Low Anterior Resection (LAR), with an incidence of about 10% [21]. Our previous study found that the incidence of AL after laparoscopic rectal cancer radical surgery was 6.6% [22]. As a “bottom-to-up” and “inside-to-outside” approach, TaTME is controversial among colorectal surgeons Liu et al. found that the incidence of AL in the TaTME group was 7.2%, which was similar with that in the LaTME group (5.3%). AL is classified into 3 grades (grade A, B, or C) according to its impact on clinical management [15]. Grade A leakage does not need special clinical treatment, whereas grade B leakage requires active therapeutic intervention but is manageable without re-laparotomy. Grade C AL requires re-laparotomy immediately [23]. AL was shown to associated with increased morbidity, poorer anal function and oncological outcomes [24-26]. A lot of measures were carried out to prevent, diagnose and treat the AL. Recent studies shown that preoperative bowel preparation can reduce the the risk of AL and Surgical Site Infections (SSIs) [27-29]. In daily work, temporary ileostomy was performed with LAR. The earlier studies of Montedori et al. found that using of a covering stoma was significantly associated with less AL and less urgent reoperation [30]. In contrast, temporary stomas cannot reduce the incidence of AL, but increase the incidence of nonelective reinterventions, readmissions, and higher costs [31,32]. The incidence of permanent stoma after LAR was various from 16.7% to 56%, and data shown that AL is one of the major risk factors for permanent stoma [33-35].
In order to avoid the risk of AL after LAR, the Bacon method was introduced by Bacon in 1945 [36]. In recent decades, modified Bacon operation gradually used in patients with low rectal cancer due to its advantages of no adjuvant abdominal incision and prophylactic stoma, no risk of AL, and good postoperative quality of life, but disputes still exist over the best choice of operation methods for patients with lower rectal cancer. A retrospective study found that the Bacon operation has smaller abdominal wounds, does not require the use of staplers and does not accompany with postoperative AL risk [37]. Similarly, Yang et al. found that modified Bacon operation is an effective treatment for lower rectal cancer owe to its relatively lower local recurrence and distal metastasis and better survival rate [38].
In this study, we firstly reported using modified Bacon method for the treatment of AL after LAR in the world. We found that this procedure has the following advantages: Firstly, the trauma of this operation is similar to that of conventional colostomy; Second. Permanent stoma can be avoided; Thirdly, the problem of AL and bleeding can be solved at the same time; Finally, normal anal structure and function can be preserved. Therefore, this study suggested that the modified Bacon operation is safe and effective in the treatment of severe AL after LAR which is worthy of clinical promotion. Further work and clinical trials need to be conducted on this matter in the future.
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Kunli Du and Pengfei Wang drafted and conceived of the manuscript. Jinqiang Liu and Jiahui Ren assisted in the drafting of the manuscript, edited the final version of the manuscript, and reviewed the literature. Ling Chen and Wei Hou made the histopathological and imaging diagnosis. Fan Feng and Jianyong Zheng made critical revisions to the manuscript. Gaozan Zheng and Shisen Li performed the operation and were involved in the drafting and editing of the manuscript. All authors read and approved the final manuscript.
None.
The authors declare that they have no competing interests.
The case report was approved by the Ethics Committee of the First Affiliated Hospital of the Air Force Medical University. And in accordance with the Declaration of Helsinki. The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
[Crossref] [Google Scholar] [Pub Med]
[Crossref] [Google Scholar] [Pub Med]
[Crossref] [Google Scholar] [Pub Med]
[Crossref] [Google Scholar] [Pub Med]
[Crossref] [Google Scholar] [Pub Med]
[Crossref] [Google Scholar] [Pub Med]
[Crossref] [Google Scholar] [Pub Med]
[Crossref] [Google Scholar] [Pub Med]
[Crossref] [Google Scholar] [Pub Med]
[Crossref] [Google Scholar] [Pub Med]
[Crossref] [Google Scholar] [Pub Med]
[Crossref] [Google Scholar] [Pub Med]
[Crossref] [Google Scholar] [Pub Med]
[Crossref] [Google Scholar] [Pub Med]
[Crossref] [Google Scholar] [Pub Med]
[Crossref] [Google Scholar] [Pub Med]
[Crossref] [Google Scholar] [Pub Med]
[Crossref] [Google Scholar] [Pub Med]
[Crossref] [Google Scholar] [Pub Med]
[Crossref] [Google Scholar] [Pub Med]
[Crossref] [Google Scholar] [Pub Med]
[Crossref] [Google Scholar] [Pub Med]
[Crossref] [Google Scholar] [Pub Med]
[Crossref] [Google Scholar] [Pub Med]
[Crossref] [Google Scholar] [Pub Med]
[Crossref] [Google Scholar] [Pub Med]
[Crossref] [Google Scholar] [Pub Med]
[Crossref] [Google Scholar] [Pub Med]
[Crossref] [Google Scholar] [Pub Med]
[Crossref] [Google Scholar] [Pub Med]
[Crossref] [Google Scholar] [Pub Med]
[Crossref] [Google Scholar] [Pub Med]
[Crossref] [Google Scholar] [Pub Med]
[Crossref] [Google Scholar] [Pub Med]
[Crossref] [Google Scholar] [Pub Med]
[Crossref] [Google Scholar] [Pub Med]
Citation: Du K, Wang P, Liu J, Zhen G, Li S, Ren J, et al. (2024). A New Way to Remedy Anastomotic Leakage after TaTme: A Case Report. J Cancer Res Immunooncol. 10:221.
Received: 01-Aug-2024, Manuscript No. JCRIO-24-33300; Editor assigned: 05-Aug-2024, Pre QC No. JCRIO-24-33300 (PQ); Reviewed: 19-Aug-2024, QC No. JCRIO-24-33300; Revised: 26-Aug-2024, Manuscript No. JCRIO-24-33300 (R); Published: 02-Sep-2024 , DOI: 10.35248/2684-1266.24.10.221
Copyright: © 2024 Du K, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.