International Journal of Physical Medicine & Rehabilitation
Open Access
ISSN: 2329-9096
ISSN: 2329-9096
Mini Review - (2024)Volume 12, Issue 2
Introduction: Conventional management of acute boutonniere deformity usually involves immobilization and typically results in two to four months out of work. Chronic fixed boutonniere often defies any acceptable correction with surgical or nonsurgical efforts. This is likely due to the delicately balanced interwoven but moveable shroud of supportive dense connective tissue at the extrinsic-intrinsic interface, which can adhere to the underlying bony phalanges during immobilization. We propose a safe method for early motion and hand use that can reduce adherence.
Methods: An understanding of the normal extrinsic-intrinsic anatomic relationships of adjacent digits takes advantage of variable forces at the inter phalangeal level when the Meta Carp Phalangeal (MCP) joints are in differing positions relative to one another. We call this the “relative motion concept,” which permits safe active motion with orthosis that protect the involved digit. Twenty-three patients with acute and chronic boutonniere deformity had their injured digit placed in a 15-20 degree greater MCP flexion orthosis compared to the adjacent digits, and were encouraged to otherwise maintain normal motion and use. The orthosis was maintained for six weeks in acutely injured patients. In fixed chronic cases, serial casting was used to achieve as much extension as possible (averaging minus 5 degrees), then a Relative Motion Flexion (RMF) orthosis was used for three months.
Results: The acute cases achieved as good or better range of motion as conventional management methods, maintaining full flexion and extension, and little or no therapy needed after six weeks of splinting. Patients with chronic boutonniere deformity maintained the extension achieved by serial casting (averaging minus 5 degrees extension) and all were able to flex to their palm. Range of motion improvement averaged 36 degrees.
Conclusion: For acute boutonniere deformity, this management technique significantly reduced morbidity, allowing functional use while healing and less therapy following treatment. For chronic boutonniere deformity, serial casting and prolonged use of RMF orthosis proved an attractive alternative to surgery.
Chronic boutonniere; Motion; Hand functioning
The relative motion concept is simple recognition that the normal functional anatomy of the Extensor Digitorum Communis (EDC) and Flexor Digitorum Profundus (FDP) muscle contraction forces vary significantly on the interphalangeal digits when there are relative differences in position of the adjacent MCP joints [1]. Using an orthosis to change and maintain the MCP joint relationship can harness these forces to advantage without requiring immobilization [2]. This is because the EDC and FDP are muscles with multiple tendons to each finger that pull equally, so change in MCP joint position of only one alters the amount of force on that digit. This was first recognized as a complication [3].
From surgeons suturing the EDC tendon to the FDP tendon over an amputation stump. This reduced the Range Of Motion (ROM) of the adjacent uninjured digits. Similarly, if the MCP joint was fused in full extension, none of the adjacent digits could flex to the palm, or if an FDP tendon was repaired after too much resection, it would be the only digit able to flex to the palm. Surgeons recognized that when a repaired long extensor tendon was placed in greater MCP extension there was laxity, so six weeks of immobilization was recommended in that position [4]. However, it was not appreciated that the laxity would be present throughout a range of motion as long as that digit maintained greater MCP extension than its neighbors. This was discovered in the late 1970’s following a simple cadaver study, and instituted in the 1980’s [5]. Since then, Relative Motion Extension (RME) orthotic management for long extensor repair and sagittal band rupture has become the favored management technique worldwide according to survey of the International Federation for Societies of Hand Therapy (IFSHT) because of its lower morbidity and earlier return to work [6].
While the relative motion concept to protect long extensor Zone IV-VII repairs is easily understood, its role for boutonniere deformity is not so evident because of the complicated delicately balanced extensor anatomic system. However, the concept is the same, with the unique advantage of offering simultaneous relative motion dual benefit in both the Dorsal Extension (EDC) and volar flexion forces to allow safe, early active motion using a RMF orthosis.
The anatomic rationale can be explained as follows [7]. Dorsally, the extrinsic EDC attaches to the intrinsic system by a trifurcation of the EDC tendon just proximal to the Proximal Interphalangeal (PIP) joint. It has a central slip that inserts into the dorsal base of the middle phalanx, where it can initiate extension, and two lateral slips, all three of similar size. Each of the two lateral slips unites with the interosseous tendons, and the lumbrical tendon on the radial side, to form the lateral bands (sometimes called conjoined lateral bands or lateral bundles). This direct attachment of the lateral band to the powerful EDC makes strong extension of the PIP and DIP joints possible, even in the complete absence of any intrinsic (lumbrical or interosseous) function if the MCP joints are stabilized to prevent hyperextension.
This can be seen in the median-ulnar palsied hand if the MP joints are splinted to avoid hyperextension. The EDC muscle alone will not extend the IP joints because of the proximal attachment of its tendons to the sagittal band and phalanx, causing MCP hyperextension instead of interphalangeal joint extension. Normally, the interosseous muscles provide the stabilization that allows EDC pull on the lateral bands and strong PIP and DIP extension. These lateral bands encircle the PIP joint, attached to one another proximally by a complex interwoven set of transverse, oblique and spiral fibers with additional tendon extension from the interosseous tendons to the central slip, known as the medial slips. This interwoven area overlying the PIP joint and distal extensor hood is sometimes called the arciform fibers and glides with finger motion as they attach across the proximal phalanx to both lateral bands [8].
Distal to the PIP joint the lateral bands approach one another and join to form the terminal tendon (sometimes called the conjoined tendon) that inserts into the distal phalangeal base. Between the two lateral bands distal to the PIP joints they attach to one another by the triangular ligament of Winslow. These attachments serve as a checkrein when the two bands move laterally. Winslow, a 17th century French anatomist, described how these bands glide laterally with PIP flexion and medially with extension, the latter in a cinching fashion between the MCP and DIP joints [9]. Thus, placing the MCP joint in greater flexion than its neighbors increases the force of the EDC, transferred via the lateral bands, to encourage medial migration as well as PIP and DIP extension.
On the volar side, the central slip pulls the entire proximal complex forward with flexion, placing slack on the lateral bands as they move laterally, preventing DIP extension with full PIP flexion, the so-called “floating finger.” The attachments of the distal extensor hood and the triangular ligament, along with the central slip insertion, prevent the lateral bands from moving volar beyond the axis of rotation of the PIP joint. When the central slip is disrupted in a boutonniere injury no deformity occurs until these injured support structures attenuate to an extent that allows migration below the axis with resultant deformity. This is why acute injury is often misdiagnosed as a sprain, only to become a boutonniere deformity days or weeks later. Central slip disruption alone will not cause the deformity. It is well known that the Fowler central slip tenotomy surgical procedure does not cause boutonniere deformity.
This is done to correct a swan neck deformity seen with chronic mallet deformity by rebalancing the system, and requires careful division of the central slip without damage to the overlying distal extensor hood or triangular ligament [10]. Afterward, no boutonniere deformity occurs if these structures are left uninjured. All three of these supportive structures must be disrupted or attenuated for boutonniere deformity to occur, as is well demonstrated in cadaver study [11] (Video 1). The lumbrical muscle is arranged in a volar position and exerts a volar force, although with EDC contraction the stabilized lateral band system transfers it dorsally to extend the DIP joint.
Video 1: Large deformity with/without relative motion flexion orthosis.
The lumbrical may also provide a volar force with active flexor profundus contraction because of its attachments to both the lateral band and the flexor profundus tendon. Placing the injured digit in greater MCP flexion relaxes the flexor profundus compared to its neighbors as well as the lumbrical muscle that arises from that profundus tendon. Thus, in an RMF orthosis there is greater force on the EDC dorsally, which encourages medial migration of the lateral bands, and there is less force volarly from the lumbrical muscle and volar interossei due to the relaxed flexor profundus, producing a dual benefit. A patient with acute boutonniere deformity is usually able to extend the IP joints when the MCP joint of the injured digit is placed in relative flexion using a tongue blade, pencil, or even stabilized with a finger (Figure 1). When placed and maintained in the RMF orthosis for six weeks the patient has hand function, and after six weeks usually requires no additional hand therapy. This is equally rewarding following acute open boutonniere repair if one lateral band remained intact.
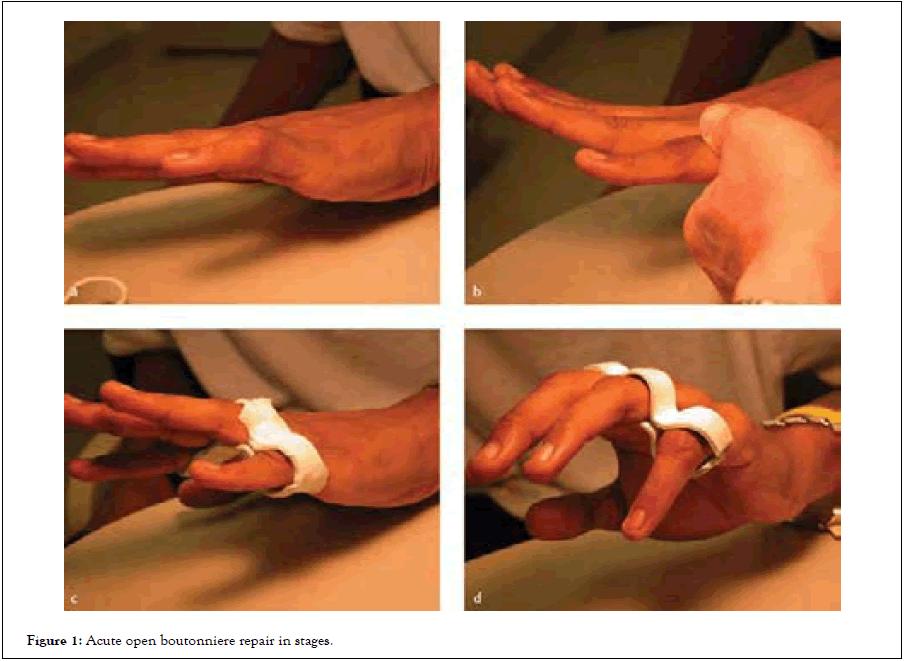
Figure 1: Acute open boutonniere repair in stages.
Chronic boutonniere deformity
Chronic boutonniere deformity has been a conundrum, with multiple operations recommended, none of which are universally successful. Indeed, results are so poor that Steichen, et al., recommended not operating at all on patients whose deformity was no worse than 30 degrees from full extension if they had adequate flexion. Simple prolonged extension splinting has been equally disappointing, with function loss during treatment and difficulty recovering flexion afterwards. We have found satisfactory results if serial casting can recover at least 20 degrees from full extension and the patient wears a functional RMF orthosis for a full three months afterwards. Our series of 15 chronic boutonniere patients were serially casted to an average of 5 degrees from full extension (0-20 degrees), then functioned in a 15-20 degree greater MCP flexion orthosis for three months, allowing most to continue work activities. All met the Strickland and Steichen criteria of “excellent” (20-90 degrees) three months after treatment [12]. Arslan, et al., recently used this method in a larger series with similar results [13-15].
The use of the relative motion concept for long extensor tendon repair and sagittal band rupture treated with RME orthoses is now well accepted. Its use for boutonniere deformity is not yet established, although the anatomic principles are the same. Using a 15-20 degree RMF orthosis, one usually sees prompt correction in the acute closed injured patient, and persistent correction after six weeks. Use for chronic boutonniere deformity requires correction of the fixed contracture by serial casting into extension followed by three months of RMF orthotic use. While the role of RMF following surgical repair for acute boutonniere has been successful, it remains to be seen if this will also be true after chronic boutonniere repair when it has not been possible to serially cast to a minus 20 degrees extension level. Thus far, we have been able to cast our patients adequately and recommend this as preferable to a surgical approach, which is still an alternative if serial casting fails. All of the patients in both groups have a Strickland and Steichen classification of “excellent” and we have not seen recurrent boutonniere deformity in any of these patients.
Citation: Merritt WH (2024) A Novel Management Technique for Acute and Chronic Boutonniere Deformity that Permits Immediate Active Motion and Functional Hand use. Int J Phys Med Rehabil. 12:720.
Received: 23-Dec-2023, Manuscript No. JPMR-23-28626; Editor assigned: 26-Dec-2023, Pre QC No. JPMR-23-28626(PQ); Reviewed: 09-Jan-2024, QC No. JPMR-23-28626; Revised: 17-Jan-2024, Manuscript No. JPMR-23-28626(R); Published: 25-Jan-2024 , DOI: 10.35248/2329-9096.24.12.720
Copyright: © 2024 Merritt WH. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.