
Anesthesia & Clinical Research
Open Access
ISSN: 2155-6148

ISSN: 2155-6148
Research Article - (2024)Volume 15, Issue 4
Background and Aim: Pain management is a key factor in the prehospital and perioperative periods of patients with hip and pelvic fractures. It has been known that the coverage of articular nerves around hip joints is critical for effective analgesia and the spread of conventional analgesics doesn’t cover the obturator nerve therefore, may not cause effective analgesia. Since, block covers most of the hip joint articular nerves, this technique provides better analgesia as compared to conventional analgesics.
Methods: Forty ASA I/II/III patients belonging to age groups 18-75 years with radiologically confirmed pelvic or acetabulum fractures were enrolled in randomized control trial. Patients were randomly allocated to one of the groups 20 patients received PENG Block (Group A) and 20 patients received traditional analgesics (Group B).
Results: There was significant difference in Numerical Rating Scale (NRS) scores at all-time intervals. There was statistically significant difference in need for rescue analgesics and antiemetic’s.
Conclusion: Ultrasound guided PENG block provides better analgesia with reduced NRS Score, need for antiemetic and improves vitals in patients with pelvic or acetabulum fractures.
PENG Block, pelvic fractures, acetabulum fractures, NRS Score, Quadriceps weakness
Pain is the most frequent complaint of patients presenting to Emergency Department with pelvic/acetabulum fractures. Surgical fixation and use of various pain management modalities are the mainstay of treatment, but in a country like ours, there is limited manpower and resources, leading to poor pain management with increased hospital stay, immobilization and increased cost on patient [1,2]. Pharmacological management include Non-Steroidal Anti-inflammatory Drugs (NSAIDS) and opioids and its use depends on the severity of pain. These drugs have many side effects and can be deleterious specially in the elderly population [3]. Regional anesthesia techniques have become quite popular due to their effective pain control and decrease in incidence of opioids or NSAIDs related adverse effects. Commonly used peripheral nerve blocks include Femoral Nerve Block (FNB), Fascia Iliaca Block (FIB) and 3–in–1 Femoral Nerve Block. Though these blocks provide good analgesia but as evident from anatomical structure of hip joint and its sensory nerve supply, these blocks don’t cover all the nerves completely. A newer technique, Pericapsular Nerve Group (PENG) block is hypothesized to provide better analgesia by covering all the sensory supply of anterior hip joint with the advantage of motor sparing effect which helps the patients to mobilize early [4,5]. Our hypothesis was that PENG block provides better analgesia in patients with pelvic or acetabulum fractures as compared to traditional pain management techniques (both pharmacological as well as non-pharmacological) in emergency department. Our primary objective was to compare the analgesic effects and duration of action of PENG Block analgesia. The secondary objectives were to compare the need of rescue analgesia for 48 hours and to compare patient satisfaction and other side effects. As PENG Block is relatively a new block, studies regarding its efficacy in pain control and motor sparing effects are limited to case reports, there have been no published literature on Indian population and the results of previous studies are limited.
This, randomized control trial was conducted in tertiary care center after approval from institutional ethics committee and with Clinical Trials Registry India (CTRI) Registration Number 2021/12/038856. 40 patients with radiologically confirmed and hemodynamically stable belonging to American Society of Anesthesiologists (ASA)-I, II and III categories belonging to age group of 18-75 years were included. Patients who refused to participate in the study, with known allergy to local anesthetics, with history of coagulopathies or on anti-coagulants/anti platelets and with infection at the block site were excluded from the study. All the patients were explained about the technique. Written informed consent was taken for the participation in the study and use of patient’s data for research and educational purposes. The study followed modified guidelines set by Indian Council of Medical Research (ICMR) and Helsinki Declaration.
Using randomization technique, patients were divided into two groups. Patients belonging to Group A received PENG block. They were subjected to routine pre anesthetic check-up for regional anesthesia after taking informed written consent. The patients were informed about the technique, NRS scale and patient satisfaction scale. The patients were brought to the procedure room in emergency department. IV lines were secured with Ringer Lactate (RL) and vitals were recorded in form of Pulse rate, Non-invasive Blood Pressure (NIBP) and SpO2 before the block. Vitals were then recorded at the intervals of 30 min for two hours and then 6 hourly for 48 hours. The block was given with 20 mL of 0.25% bupivacaine with 4 mg (1 mL) of dexamethasone (Total 21 mL) under ultrasound guidance. Group B served as a control group with patients receiving analgesics as per the protocol of orthopedics department of the institute.
PENG block was administered with patient in supine position with low frequency curvilinear USG transducer (2-5 MHz) placed in transverse plane over Anterior Inferior Iliac Spine (AIIS). Medical end of the probe was rotated to align with Iliopubic Eminence (IPE) and superior pubic ramus. Structures viewed were IPE, iliopsoas muscle and tendon, femoral artery. The target site was bone surface of ilium lateral to psoas tendon. A 22G needle was inserted from lateral to medial using in plane technique (Figure 1). As the needle was in musculofascial plane, negative aspiration was done to confirm the lack of inadvertent vascular puncture. A total of 21 mL local anesthetic solution was injected while observing elevation of iliopsoas muscle and psoas tendon (Figure 2).

Figure 1: Ultrasound guided Pericapsular Nerve Group (PENG) block.
Figure 2: Local anesthetic being deposited around psoas tendon.
Pain scoring was done with the help of NRS scale, vitals monitoring and ability to perform a straight leg raising test of affected limb at interval of 30 min for 2 hours and then 6 hourly for 48 hours in the patients belonging to both the groups. Rescue analgesics in the form of Intramuscular (IM) diclofenac 75 mg and IV tramadol 50 mg were given when NRS was more than 5 and time was recorded. Total consumption of analgesics was calculated at the end of 48 hours. Any complications like nausea, vomiting, delirium, hematoma, accidental inoculation of drugs into vessels, paresthesia etc. were also recorded.
The data was recorded and entered in MS Excel, then analyzed using Statistical Package for Social Sciences (SPSS) version 22. Qualitative variables (frequency and percentage) between two groups were analyzed by applying Chi-square test whereas quantitative variables (mean and standard deviation) were calculated using unpaired T test. p<0.05 was taken as statistically significant.
Demographics and baseline vitals details were comparable in both the groups. The mean age of the patients in the study was 46.85 years Standard Deviation (SD=16.6 years) with range of 18-70 years. Heart Rate (HR) and Blood Pressure (BP) were consistently monitored at the predefined time intervals of 6, 12, 24 and 48 hours. The mean HR among the individuals of two groups was comparable (p=0.538). When the groups were subsequently followed up at different intervals, HR of patients in group A was found to be significantly lower as compared to patients enrolled in group B (Table 1). There was no significant difference in Mean Arterial Pressure (MAP) between two groups at subsequent follow-ups as compared to baseline measurements.
| Variables | Groups | ||
|---|---|---|---|
| Heart Rate | A (n=20) | B (n=20) | P value |
| Mean ± Standard deviation | Mean ± Standard deviation | ||
| At 6 h | 79.35 ± 7.081 | 87.95 ± 7.571 | 0.001 |
| At 12 h | 79.65 ± 6.8 | 88.85 ± 7.028 | <0.001 |
| At 24 h | 80.1 ± 6.882 | 87.35 ± 6.175 | 0.001 |
| At 48 h | 79.15 ± 5.687 | 88.4 ± 7.556 | <0.001 |
Table 1: Comparison of heart rate between the two groups.
Patient Movement Assessment (PMA) was done by flexion of affected hip and a straight leg raise test to 15⁰ between two groups (Figure 3). Chi square test was applied for comparison between the groups and at 0 min, p value came out to be 1 (p>0.05) which was not significant. While at 30 min, 80% patients in Group A depicted movement while 20% patients couldn’t. Meanwhile 40% patients in Group B depicted movement at 30 min and 60% couldn’t. On comparing, p value came out to be 0.02 (p<0.05) which was significant indicating that there is difference in PMA at 30 min in both the groups.
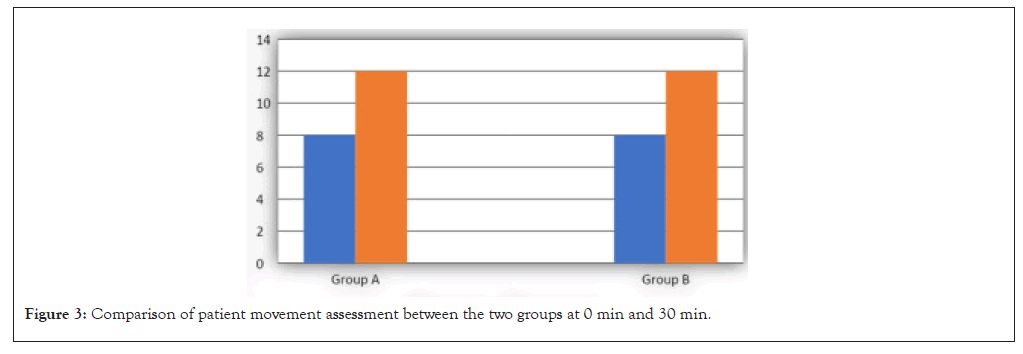
Figure 3: Comparison of patient movement assessment between the two groups at 0 min and 30 min.
5 patients in Group A required analgesia more than once while 18 patients in Group B required analgesia more than once. On comparing, p value came out to be <0.001 which was significant (Table 2).
| Variables | Group | |||||
|---|---|---|---|---|---|---|
| A (n=20) | B (n=20) | |||||
| Frequency (n) | Proportion (%) | Frequency (n) | Proportion (%) | P value | ||
| Time | No | 11 | 55.0 | - | - | |
| <24 h | 3 | 15.0 | 20 | 100.0 | <0.001 | |
| 24-36 h | 3 | 15.0 | - | - | ||
| 37-48 h | 3 | 15.0 | - | - | ||
| Total | 20 | 100.0 | - | - | ||
Table 2: Time required for first rescue analgesia.
Among Group A, 5 patients required antiemetic while 13 patients in Group B required antiemetic. Hence patients in Group A required significantly less antiemetic than patients enrolled in Group B (p=0.025). There was decline in mean NRS score among group A patient who maintained NRS score of 3.15 to 3.90 meanwhile group B patients maintained NRS Score of 6.35 to 6.60 at most of time intervals. The reduction in NRS Score was significantly greater in Group A patients as compared to Group B patients (p<0.001) except at the baseline (Table 3 and Figure 4).
| Variable | Group | ||
|---|---|---|---|
| Pain Assessment Score Numeric rating scale (NRS) | A (n=20) | B (n=20) | P value (Unpaired T test) |
| Mean ± Standard deviation | Mean ± Standard deviation | ||
| 0 min | 6.80 ± 1.24 | 7.15 ± 1.42 | 0.42 |
| 30 min | 3.90 ± 1.58 | 7.00 ± 1.45 | <0.001 |
| 60 min | 3.35 ± 1.13 | 6.60 ± 1.46 | <0.001 |
| 2 h | 3.25 ± 1.25 | 6.25 ± 1.83 | <0.001 |
| 6 h | 3.15 ± 1.30 | 6.50 ± 1.57 | <0.001 |
| 12 h | 3.25 ± 1.41 | 6.35 ± 1.66 | <0.001 |
| 24 h | 3.35 ± 1.49 | 6.40 ± 1.50 | <0.001 |
| 36 h | 4.00 ± 1.37 | 6.45 ± 1.53 | <0.001 |
| 48 h | 4.20 ± 1.32 | 6.45 ± 1.66 | <0.001 |
Table 3: Comparison of Pain Assessment Score (PAS) Numeric rating scale (NRS) between two groups.
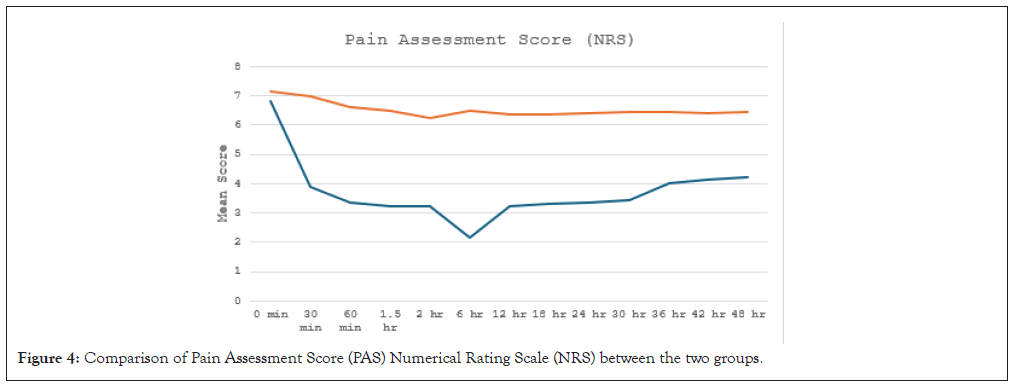
Figure 4: Comparison of Pain Assessment Score (PAS) Numerical Rating Scale (NRS) between the two groups.
The present study shows that PENG Block is suited for complete hip analgesia as compared to conventional analgesia methods. It has been known that the coverage of hip joint articular nerve is critical for an effective analgesia [6]. Magnetic Resonance Imaging (MRI) findings have shown that the spread of conventional analgesic does not cover the obturator nerve, therefore, may not cause effective analgesia. Since, PENG block covers more hip joint articular nerves, it seems that this technique can cause better analgesia compared with the conventional analgesic. It showed PENG block with impressive effects on dynamic pain score and good preoperative analgesia. Pericapsular Nerve Group Block (PENG) has been deemed as a safe and effective regional technique for postoperative pain after hip surgery targeting anterior capsule of the hip joint [5]. As reported by Ahiskalioglu et al., it is hypothesized that Local Anesthetic (LA) agent will spread in the transverse plane and show lumbar plexus block-like effect in high volume PENG block applications [7]. An anatomic study by Short et al., demonstrated that high branches of both the femoral and obturator nerves (Figures 5 and 6), provide innervation to the anterior hip capsule and that the anterior hip capsule receives the major sensory innervation, whereas the posterior and inferior capsules have minimal sensory fibers [8]. In a cadaveric study, Gerhardt et al., demonstrated that when dye was used for PENG block, it stained the entire anterior hip capsule areas related to the articular branches of femoral, obturator and accessory obturator nerves [9].
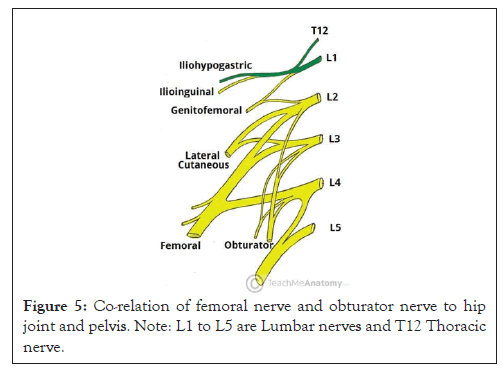
Figure 5: Co-relation of femoral nerve and obturator nerve to hip joint and pelvis. Note: L1 to L5 are Lumbar nerves and T12 Thoracic nerve.
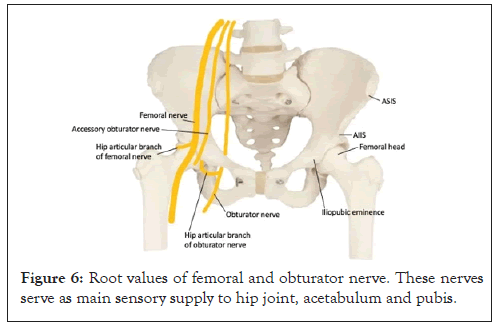
Figure 6: Root values of femoral and obturator nerve. These nerves serve as main sensory supply to hip joint, acetabulum and pubis.
In the present study, as patients belonged to elderly age group, 25% over 60 years of age; doses of systemic analgesics administered are often limited by the fear of inducing serious adverse events. Therefore; PENG block was found to be safe with minimal side effects in the elderly age group. In the present study, there was a significant difference in the movement assessment of the patients in which PENG block was administered. Compared with systemic analgesia, pain on movement within 30 min after PENG block placement was significantly less by approximately 3.1 out of 10. Allard et al., also reported that the immediate mobility of the operated limb (quadriceps) as measured by the Medical Research Council (MRC) scale was different between the two groups, with an average mobility rating of 5 in the PENG block group versus 2 in the femoral block group [10]. In a similar study conducted by Mosaffa et al., the authors found that after 15 min of block, as well as, after 12 hour of post-surgery, Visual Analogue Scale (VAS) score was significantly reduced in the PENG block group compared with the conventional analgesia group [11]. The first time of the analgesic consumption after surgery was significantly longer in the PENG block compared with the conventional analgesia and the total dose of morphine consumption for 24 hours significantly reduced in the PENG block compared with the conventional analgesic group. Orozco et al., reported minimal pain up to 72 hours postoperatively with little or no rescue analgesics required, in a retrospective case series of patients undergoing hip arthroscopic surgery receiving PENG block [12]. However, Patel et al., report that their large historical cohort data suggested that the analgesic efficacy of the PENG block was clinically equivocal to systemic analgesia alone for ambulatory hip arthroscopy [13].
In the present study there was a NRS above or equal to 4 was observed after 36 hours in the PENG block group, more so in the patients of anterior acetabulum fractures and was significantly less than those participants who did not receive PENG block. In a study, Pagano et al., reported that median reduction of pain in their case series on administering PENG block was 4.83 points in preoperative Numerical Rating Scale (NRS) at rest and 6 points in dynamic state. Interestingly, the patients in this case series presented different hip pathologies and all of them reported significant preoperative pain relief and satisfactory postoperative analgesia [14].
We need more studies, dye injection studies to confirm the spread of local anesthetics and randomized control trials to establish its efficacy, safety and advantages over other regional analgesic techniques.
Ultrasound guided PENG Block significantly provides better analgesia than conventional multimodal analgesics. In our study the patients were mainly elderly and the PENG block was found to be effective in improvement in the Visual Analogue Scale (VAS) score as well as in the improvement of the range of motion which resulted in decrease incidence of deep vein thrombosis. It significantly reduces NRS Score, need for antiemetic and improves vitals in patients with pelvic or acetabulum fractures. It was better tolerated by patients as compared to systemic analgesics. We need more studies, dye injection studies to confirm the spread of local anesthetics to establish PENG block efficacy, safety and advantages over other regional analgesic techniques as our study included different hip pathologies and the PENG block was found to be effective in all up to some extent in improving the VAS score.
All research performed by department of Anesthesia, Indira Gandhi Medical College, Shimla, Himachal Pradesh, India.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Mahajan S, Pandit N, Kashyap S, Kaushal S (2024). A Randomised Control Trial of Pericapsular Nerve Group (PENG) Block Analgesia in Pelvic or Acetabulum Fractures. J Anesth Clin Res. 15:1149.
Received: 20-Jul-2024, Manuscript No. JACR-24-33037; Editor assigned: 22-Jul-2024, Pre QC No. JACR-24-33037 (PQ); Reviewed: 09-Aug-2024, QC No. JACR-24-33037; Revised: 20-Aug-2024, Manuscript No. JACR-24-33037 (R); Published: 26-Aug-2024 , DOI: 10.35248/ 2155-6148.24.15.1149
Copyright: © 2024 Mahajan S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.