Journal of Cancer Science and Research
Open Access
ISSN: 2576-1447
+44 1478 350008
ISSN: 2576-1447
+44 1478 350008
Case Report - (2023)Volume 8, Issue 2
Primary squamous cell carcinoma of the parotid gland is a rare and an aggressive malignancy and has devastating consequences. Although managed with radical surgery and adjuvant radiotherapy, the outcome of this disease remains dismal. It is vital to distinguish these tumors from metastatic squamous cell carcinoma and other primary malignancies of the parotid gland via clinical and histological examinations. We hereby report a case of a young male patient presented with a progressively increasing mass in the left parotid region, with radiology and pathology consistent with primary parotid gland SCC along with lung metastasis. He received palliative chemotherapy initially but later passed away due to progression of disease.
Tumor; Squamous Cell Carcinoma (SCC); Parotid cancer; Neoplasm
Parotid neoplasms account for 70%-80% of the salivary gland tumors of which Squamous Cell Carcinoma (SCC) is the rarest histological subtype [1,2]. SCC de novo from the parotid gland reported only 0.3%-6.9% of all parotid malignancies. In addition, SCC of the salivary glands is related to comparatively poor prognosis [3]. The diagnosis of parotid SCC depends on the exclusion of high grade mucoepidermoid carcinoma and metastatic SCC. Still to this date, the presenting features and optimal choice of management for primary SCC of the parotid gland are not fully comprehended, even if it is subclassified as a high grade tumor [4,5]. SCC is epithelial in origin, consisting of epidermal cells associated with keratin pearls, intracellular keratinization and intercellular bridges [6]. Primary parotid SCC has a unique and unequivocal set of characteristics setting it apart from other parotid cancers.
A 30 year-old non-smoker male with Insulin Dependent Diabetes Mellitus (IDDM) on insulin for 20 years who presented with painful swelling of his left parotid which was progressively increasing over the last 2 months along with intermittent productive cough for 2 months, with progressive dysphagia for 15 days with no history of hemoptysis or hoarseness of voice. On examination, a firm mass measuring about 6 × 5 cm was present in the left parotid around the angle of mandible, mildly tender and fixed to skin. The overlying skin was normal with no ulceration and left cervical lymph nodes were palpable as well (Figure 1). The devastating outcome in this case could be explained secondary to delay in seeking medical care and our patient’s financial stresses which proved to be fatal for him. Overall delay in seeking medical care, lack of awareness and financial problems are the major factors in our country for high rates of morbidity and mortality.
On investigating further, Computerized Tomography (CT) of face and neck showed an isolated left parotid tumor measuring 6.3 × 4.9 × 7.5 cm (AP × TS × CC) infiltrating into the carotid space medially and anteriorly abutting the left masseter muscle (Figure 2). Moreover CT of the chest revealed bronchiectatic and fibroatelectatic changes predominantly in the left upper lobe. Some alveolar nodular infiltrates which were consistent with metastatic disease. Fine-needle aspiration cytology from the lesion showed multiple scattered aggregates and clusters of malignant keratinizing squamous epithelial cells with enlarged dense hyperchromatic irregular nuclei and keratinized cytoplasm. Several ghost cells were also seen. This was followed by Trucut biopsy of left cervical lymph node left cervical lymph node which was consistent with keratinizing squamous cell carcinoma with individual cell keratinization and keratin pearl cytoplasm (Figure 1).
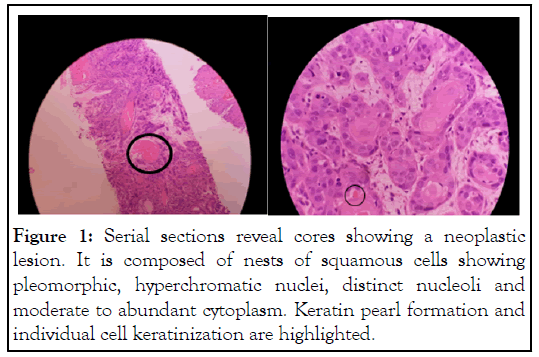
Figure 1: Serial sections reveal cores showing a neoplastic lesion. It is composed of nests of squamous cells showing pleomorphic, hyperchromatic nuclei, distinct nucleoli and moderate to abundant cytoplasm. Keratin pearl formation and individual cell keratinization are highlighted.
Figure 2: CT scan showing left parotid gland enlargement with heterogeneous enhancement involving superficial and deep part.
The patient was briefed regarding the rarity and aggressive etiology of the disease he was advised chemotherapy protocol carboplatin and paclitaxel with a palliative intent. The patient received 5 cycles of chemotherapy over a period of four months. However, due to progressive disease, the patient passed away due to aspiration pneumonia.
Primary Squamous Cell Carcinoma (PSCC) is a unique entity of the parotid gland neoplasms. The scarce occurrence of the true primary parotid SCC, consisting of only 0.1%- 3.4% of all parotid malignancies, accounts for the restricted data on the subject [1]. Epidemiology of this aggressive tumor shows that it has a Male: Female ratio of 2:1 and presents in elderly individuals with a mean age of presentation at 64 years [7].
PSCC does not exhibit any specific growth model or clinical characteristics that could differentiate it from its other counterparts [5]. The typical presenting complaints of the individuals are a parotid mass, neck mass and facial paralysis in 17%-33% of the cases along with pain varying between 8%-33%. Moreover the mass may be fixed to the skin above or underlying structures [8].
This neoplasm originates from the ductal epithelium secondary to chronic inflammation consequently leading to metaplasia that turns into invasive squamous cell carcinoma [9]. The histological appearance shows intracellular keratinization, intercellular bridging, and keratin pearl formation with scanty mucus secretion. However, there is nothing to differentiate these squamous cell carcinomas from those originating from other areas [6].
The histology of the parotid malignancies therefore contribute significantly to the patient’s survival while fine needle aspiration cytology remains the principal choice of investigation in major salivary gland tumors [7]. Total parotidectomy and superficial parotidectomy with facial nerve conservation are the ideal form of treatment for primary SCC of the parotid gland and other classes of high-grade parotid carcinomas with the extent of surgery directly related to the extent of cancer [5].Furthermore another population based study analyzed 191 patients from 1988-1998 with SCC of the major salivary glands showing that SCC had one of the worst outcomes along with a 5-year actuarial survival of 46.1% [10]. Previous studies have shown that involvement of clinically palpable nodes in the neck worsened prognosis in the primary SCC of the parotid gland [11]. Moreover, age more than 60 years, ulceration of the skin, deep fixation and facial nerve involvement are other factors associated with significantly poor prognosis [7].
The devastating outcome in this case could be explained secondary to delay in seeking medical care and our patient’s financial stresses which proved to be fatal for him. Overall delay in seeking medical care, lack of awareness and financial problems are the major factors in our country for high rates of morbidity and mortality. Primary squamous cell carcinoma of the parotid is an uncommon malignancy usually presenting in advanced stages with facial nerve involvement and distant metastasis. It's an aggressive malignancy and prognosis correlates most strongly with clinical stage, emphasizing the importance of early diagnosis which if delayed results in poor outcomes. It is aggressive malignancy with a relatively poor outcome and therefore requires a belligerent multimodality.
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
Citation: Khan YN, Mala A, Kumar V, Osmani AH (2023) A Rare Case of Parotid Gland Neoplasm with Squamous Cell Origin. J Can Sci Res. 8:528.
Received: 02-Jan-2023, Manuscript No. JCSR-23-21477; Editor assigned: 05-Jan-2023, Pre QC No. JCSR-23-21477(PQ); Reviewed: 19-Jan-2023, QC No. JCSR-23-21477; Revised: 26-Jan-2023, Manuscript No. JCSR-23-21477(R); Published: 02-Feb-2023 , DOI: 10.35248/2576-1447.23.8.533
Copyright: © 2023 Khan YN, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.