Journal of Food: Microbiology, Safety & Hygiene
Open Access
ISSN: 2476-2059
ISSN: 2476-2059
Review Article - (2022)Volume 7, Issue 11
Listeria monocytogenes foodborne outbreaks remain one of the leading causes of illnesses, hospitalizations and deaths on a global scale. Convenient foods and global food behavior changes has forced increasing number of people to consume foods prepared outside their homes, potentially exposed to hazards of poor hygiene practices along the production chain in foodservice establishments. Few resources are directed at developing countries for the investigation of foodborne disease outbreaks and incidences of listeriosis may pass uninvestigated, unrecognized, unreported or undocumented. Persistence of contamination at retail establishment’s is a reality not well understood and further studies are required to gather facts that influence the fate of L. monocytogenes. Although incidences in many food categories have improved, the rate has remained constant during the last decade, with current outbreaks repeatedly in small outbreaks than previously recognized. In developing nation’s particularly Sub-Saharan regions documentations lagging behind and it’s not clear whether absents of these reports means no outbreaks present. Realization of current upsurge from food vehicles not traditionally associated with L. monocytogenes and understanding of elimination steps by food retailers after outbreaks provides key knowledge about exposure mitigation with prevention of its growth remains a principle control element.
Foodborne disease outbreak; Listeria monocytogenes; Listeriosis; Retail establishments; Foodborne illness outbreak
Total removal of Listeria monocytogenes contaminants from retail food establishment’s facilities after a foodborne outbreak or food recall is increasingly challenging and most retail food establishments lacks laboratory facilities to confirm its absence or presents. As a result the fate of L. monocytogenes after foodborne outbreak is not known. Foodborne illness is any disease that enters the human body through the consumption or handling of contaminated food or water. There are more than 250 different known foodborne diseases, and they can be caused by bacteria, viruses, parasites, or harmful toxins and chemicals that have contaminated food. According to the CDC estimates, 1 in 6 individuals (or forty eight million human beings) each year are affected by foodborne illness while an estimated one hundred and twenty eight thousand (128,000) are hospitalized, and three thousand (3000) die. This makes foodborne disease is a very significant problem of public health food safety concern. These estimates help us understand the scope of this public health problem. However, to develop effective prevention measures, we need to understand the types of foods or processing activities contributing to the problem. The globalization of the food supply and trade has resulted to the rapid and widespread international distribution of foods, with food supply chains now cross multiple national borders. The unfortunate part is that even contaminated foods can also be distributed and pathogens like L. monocytogenes can be inadvertently spread into new geographical locations from one nation to other exposing consumers with unfamiliar or exotic foodborne hazards. Several studies have been done on epidemiology, foodborne surveillances on various infections or illnesses to trace, identify and inspect food establishment’s characteristics and food safety conducts associated with foodborne outbreaks with all the scientists agreeing on the possible indicators of foodborne illness, food retail establishment characteristics and food safety practices that cause foodborne illnesses. However, little analytical studies have been done to trace what action or measures are put in place by every country in the world to ascertain or to make sure microbial contaminants are controlled or eliminated in a retail food establishment after a foodborne outbreak announcement or food recalls so that all facilities are free from causative agents. Foodborne diseases impede socioeconomic development by straining health care systems, and harming national economies, tourism and trade.
This review will highlight L. monocytogenes foodborne outbreaks, its fate in retail facilities and actions undertaken by food traders to make sure their facilities are free of microbial contaminants after outbreaks or food recalls. Further discussion will include infection of people with L. monocytogenes, foodborne Illness complaint history, foods more likely to contain L. monocytogenes, post foodborne outbreaks and investigation of a foodborne outbreak. Finally, this review also explores persons at risk of L. monocytogenes illness, guidance for listeriosis prevention amongst persons at risk and symptoms of L. monocytogenes illness. An introduction of WGS and rapid reliable routine testing methods of L. monocytogenes in retail establishments to establish control measures may help with knowledge to establish the fate of L. monocytogenes that can aid in the eradication and possible elimination of these events. Listeriosis is a serious foodborne infection usually caused by consumption of food contaminated with the pathogen L. monocytogenes. Nowadays scientific researchers use DNA analysis through WGS of L. monocytogenes bacteria isolated from patients and implicated food products to identify cases of illness that may have been part of the outbreak. The L. monocytogenes foodborne pathogen is obtained from diagnostic testing; Pulsed Field Gel Electrophoresis (PFGE) and Whole Genomic Sequencing (WGS) used to determine DNA fingerprint patterns. These molecular methods which targets nucleic acids are more accurate, reliable, can show genetically related or unrelated isolates, minimize incidences of false positive reports and simultaneously capable of tracing back the origin of the bacteria contamination as compared to conventional culture methods. Various researchers use bioinformatics metadata from their country’s database records of strains isolated from patients, contaminated food, food contact surfaces and the food production places. For instance in the USA, database from pulse net the national subtyping network made up of state and local public health laboratories and federal food regulatory laboratories that performs molecular surveillance of foodborne infections. PFGE and WGS are laboratory molecular techniques used by research scientists to produce DNA fingerprints for bacterial isolates such as L. monocytogenes. A bacterial isolate is a group of the same type of bacteria. Pulse net investigates bacterial isolates from sick people, contaminated food, and the places where food is produced. Most researchers have learned that a L. monocytogenes isolate that had been isolated from a sample of implicated food from a patient’s home during the outbreak investigation had a PFGE pattern combination or WGS sequence that was different or similar to the known pattern combinations in the outbreak. When pulse net database is searched for complement matching DNA finger print sequences from stains isolated in the course of the outbreak identifies consumers matching isolates and products that are contaminated can be tracked back or identified. Listeriosis is rarely reported in the Southern African Hemispheres in spite of the increasing rate of L. monocytogenes in several foodborne outbreaks reported in advanced countries. After the reported world’s largest outbreak of listeriosis in South Africa in 2017-2018 by Codelia Mondela a chronicle reporter on March 28 2018, the World Health Organization (WHO) under the WHO’s health emergencies programmer, the Global Outbreak Alert and Response Network (GOARN) and the International Food Safety Authorities Network (INFOSAN) has chosen sixteen African countries to provide financial assistance for awareness and readiness to a possible outbreak of L. monocytogenes in Africa. The sixteen countries in which the disease were feared to have broken into from neighboring South African were Angola, Botswana, the Demographic Republic of the Congo, Ghana, Lesotho, Madagascar, Malawi, Mauritius, Mozambique, Namibia, Nigeria, Swaziland, Tanzania, Uganda, Zambia and Zimbabwe. WHO considered these countries at risk of contracting the disease since they may have imported contaminated products from South Africa and may need help to improve their ability to prepare for, detection and responding the potential L. monocytogenes outbreak. Countries like Zimbabwe had since responded by banning the importation of all the implicated products, no studies has been done to ascertain that all retail establishment trading implicated products were free from L. monocytogenes contamination. The foodborne listeriosis had threatened the food safety of many countries in Southern Africa especially those depended on Ready To Eat (RTE) processed meat imports from South Africa. Implementation of national response plans, such as enhanced surveillance, total destruction or recall of implicated food products, detection of new cases, as well as undertaking risk or epidemiological assessment of all RTE implicated products in retail outlets and working to ensure safe food safety systems are put in place remain a big challenge in developing nations. Whether the foodborne pathogen is totally eliminated from the retail establishments or consumer residence after a foodborne outbreak report remain a big question. Food retail establishments are predicted to play an important role in L. monocytogenes transmission to human’s retail delicatessen in particular has been implicated as a significant reservoir. Food and Drug Administration (FDA). In recent years, fresh produce related L. monocytogenes outbreaks have increased in frequency and are recognized as a serious food safety icon of public health concern. Grocery stores and retailers were addressed as key checkpoints during produce transportation and distribution. The universal occurrence and incidences of L. monocytogenes in food, persistence in food processing establishments and the risk of contracting foodborne listeriosis have been thoroughly reviewed recently with all food scientists agreeing that L. monocytogenes is a serious food safety pathogen of public health concern. However its fate in retail establishments’ environments or facilities is not clearly stated to consumers’ guidance after announcement of a foodborne listeriosis and recalls of implicated food products. This review looks at its fate in retail establishments. Listeria monocytogenes is a small gram-positive coco-bacillus rod in shape (0.5 μm-4 μm in diameter and 0.5 μm-2 μm in length), non-spore-former, facultative anaerobe, catalase-positive, oxidase-negative, Esculin hydrolysis positive, Hippurate hydrolysis positive, CAMP positive bacteria with a tumbling motility at (20℃–25℃) on wet microscope preparations due to peritrichous flagella. This disease causing bacteria has been identified as the only Listeria species that can cause infection in both humans and animals which have been implicated in several foodborne outbreaks associated with human infections. However, other species such as L. Seeligeri and L. welshimeri have been reported more than two decades ago as agents of sporadic cases of listeriosis in human, but L. monocytogenes remains a significant cause of human foodborne illnesses [1-5]. Although it is ubiquitous in the environment, it is widely found in dump environments, animals, water, rotting vegetables and food processing facilities or establishments. Animals especially cattle can shed the pathogen in their droppings spreading it in the environment even if not showing symptoms of sickness. This foodborne pathogen is a halo tolerant which can survive some food preservation measures such as wide range of pH between (4.4-9.5), fairly low moisture content and can proliferate or grow under very low temperatures such as refrigeration conditions (4℃-8℃) and be able to thrive in a wide temperature range between (1℃-44℃) which makes it very difficult to control in food processing establishments or retail markets. RTE processed and raw products with a stable or relatively longer retail shelf display life are of particular public health food safety concern due to their possible longer contamination time length with L. monocytogenes. In retail shops facilities and food processing plants L. monocytogenes is able to successfully attach to many food contact surfaces, form and persist on biofilms and this character makes it a food industry pathogen of very serious food safety concern with threat to public consumers despite implementation of stringent sanitary protocols. Due to its pervasive, persistent and adaptable character, L. monocytogenes is capable of entering the food processing establishments, colonizing the food supply chain contaminating various processed food products or processing environments. This allows the pathogen to multiply and even to be resilient, persisting in food processing establishments for years and this may be evident of its hard to control shown by intermittent contamination of foods. Compared to other foodborne illnesses worldwide, listeriosis is occasional but it’s of very serious consequences. Listeria monocytogenes infection can also appear as a systemic (invasive) listeriosis with, high hospitalization, more severe symptoms and cases of high fatality rates, although in the majority of cases it is expressed as a light, febrile illness. According to the US FDA statistics at a glance, this foodborne disease has a high mortality rate ranging between (20-30) percent and 94% hospitalization rate even though there is adequate antibiotic treatment. Thus why listeriosis is amongst the fatal foodborne illnesses list. The occurrences of listeriosis is low in the general population despite the wide spread of the pathogen in the environment and the relatively high frequency of isolation in foods. The prevalence of invasive listeriosis is more pronounced in vulnerable population group’s including pregnant women, the elderly and people with immune compromised systems. Improved control measures for the past three decades have considerably diminished occurrence of L. monocytogenes in several food product categories, particularly in meats and processed agricultural products. However, the rate of illness has remained constant during the last decade. Additionally current foodborne epidemic reports have stood against the presumptions of existing consumer exposure assessments and our perception of the influence of L. monocytogenes existence in retail establishments, harboring in facilities and physical domain that interacts with specific constituents of a food on foodborne illness. Listeria monocytogenes is found everywhere in the food processing environment and its control in retail establishments’ facilities demand paying continual particular attention by food traders and regulatory authorities for public health concern. Therefore, better understanding the fate of this serious foodborne pathogen after an outbreak or food recalls is necessary to design better mitigation measures to counteract the occurrence of listeriosis linked to retail establishment’s contamination.
Infection of people with Listeria monocytogenes
Human beings contract listeriosis infection by consumption or handling of food, contact with food contact surfaces, equipment and animal products contaminated with L. Monocytogenes. Although healthy people rarely become seriously ill from this disease with 0.1 to 10 cases per 1 million people per year depending on the countries and regions of the world, it can be very malignant for pregnant women, elderly people above 65 years of age, unborn babies, newborns and individuals with immune compromised immune systems. These groups of people who are at higher risk of serious listeriosis infections should avoid consumption of high risk food products (contaminated meat, ready to eat processed meats, fresh produce and unpasteurized dairy products) usually implicated in foodborne outbreaks of L. monocytogenes bacteria. While these are high risk foods, listeriosis has been associated with virtually every food category when the food is not properly handled and prepared. Prompt antibiotic treatment can help curb the effects of listeria infection. An estimated 1,600 people become infected with listeriosis each year, and about 260 lose lives, with pregnant women and their newborn being more vulnerable as compared to any other groups. When a foodborne outbreak occurs due to the presents of L. monocytogenes in implicated food products, tracing back of suspected food products to a common source point of contamination requires a considerable duration of time for investigation. During this period where epidemiologic and microbiologic surveillances are made, consumers are exposed and new casualties continue to contract the disease and the timeline for total illness control can be prolonged. The initial diagnosis of listeriosis is made based on clinical symptoms and detection of the bacteria in a smear from blood, Cerebra Spinal Fluid (CSF), meconium of newborns (or the fetus in abortion cases), as well as from faces, vomitus, foods or animal feed. Various detection methods, including Polymerase Chain Reaction (PCR) and whole genomic sequencing are now available for accurate diagnosis of listeriosis in humans and rapid reliable methods must be adopted for retail establishments for easy detection Table 1 [6-10].
| Region and year | No. of Cases | Reported deaths | Implicated food product | Detection method | Affected states | Food recall | Reference |
|---|---|---|---|---|---|---|---|
| Portugal (2009-2012) | 30 | 11 | Cheese | WGS | Lisbon and Vale do Tejo region. | Yes | (Magalhaes et al., 2015) |
| Denmark (2013-2014) | 41 | 17 | Rolled pork sausages/ deli meat | WGS | Odense Copenhagen | Yes | (The Local. dk, 2014). A Danish media report. |
| USA and Canada (2015-2016) | 23 | 1(USA) | Packaged leafy green salads | PFGE, wgMLST and WGS | USA (12) and Canada | Yes | (Self et al., 2019) |
| European Union (EU) (2015-2018) | 32 | 6 | Frozen Corn | WGS | 5 EU Countries: (Austria, Denmark, Finland, Sweden and UK) | Ye | (FSN, 2018) |
| South Africa (2017-2018) | 1060 | 216 | Polony meat product | WGS | 9 Provinces | Yes | (NICD, 2018) |
| USA (2020) | 36 | 4 | Enoki Mushroom | WGS | 17 States | Yes | (CDC, 2020) |
| USA (April-June 2021) | 3 | 1 | Frozen fully cooked chicken products | WGS | 2 | Yes | (CDC, 2021) |
Table 1: Timeline of selected L. monocytogenes multistate outbreak infection cases in the world (2009-2021).
Although the cases of reported incidences of listeriosis are small, the high fatality rate associated with this foodborne infection makes it a serious public food safety health of concern. Many people especially in developing nations do not seek medical care for most foodborne illnesses, so their illnesses cannot be diagnosed or reported to public health officials and the disease will sometimes pass unnoticed. The foodborne L. monocytogenes outbreak occurred in South Africa in (2017-2018) period becomes the largest ever reported listeriosis outbreak in the world so far, but no available documentation with reports of cases linked to all other countries who were dependent on implicated foods imported from this country are available. As a result, most cases of the foodborne illnesses are not linked to the actual foodborne outbreak. There are so many reasons for not linking most foodborne illnesses to outbreaks because pathogens themselves can also spread in other ways, such as by water or cross contamination directly from one person to another person. In addition some detection methods such as culture independent test methods that may be in use in less developed nations may not provide the information needed to link it to an outbreak or relating to point source of contamination as compared to molecular methods like whole genomic sequencing. Exposure to contaminated food with high counts of L. monocytogenes is the principal route of infection although transmissions can also be between humans, notably from pregnant women to unborn babies. The pathogen can survive home or commercial refrigerated temperatures and there are high possibilities of spreading to food products or contact surfaces through cross contamination.
An overview of symptoms of L. monocytogenes infection
Human listeriosis can result in various symptoms, depending on the person and the organs of the body affected. Women who are pregnant experience fever, flu-like symptoms, fatigues and muscle aches. In most cases infections during pregnancy may lead to miscarriages, stillbirth, premature delivery or life threatening infection of newborn baby or even death of the baby if not treated. This is because pregnant women can pass L. monocytogenes to their unborn child in the womb or during giving birth. In individuals none other than pregnant, symptoms include headache, stiff neck, confusion, loss of balance, and convulsions in addition to fever and muscle aches. Comparing to other common foodborne pathogens species of Escherichia coli (E. coli), Salmonella and Vibrio L. monocytogenes incubation period can be prolonged or may not become apparent for some time before appearance of symptoms. However the incubation period is variable and symptoms can start appearing anything from 24 hours to 4 weeks after exposure to contaminated food, but symptoms appearance can range from the same day to up to 70 days later (Table 2) [11-15].
| Pathogen | Typical start time of symptoms appearance |
|---|---|
| E. coli | Three-four days |
| Listeria monocytogenes | one-four weeks |
| Salmonella | six hours-six days |
| Vibrio | one-two days |
Table 2: How long it typically takes for someone to have symptoms after being infected with some of the most common foodborne bacteria (CDC, 2021).
Selected multistate incidences of L. monocytogenes outbreaks in United States of America 2011-2021
When more than one person contracted the same illness from similar contaminated food or beverage, the incident is referred to as a foodborne disease outbreak. When the incident involves more than two different areas or regions it becomes a multistate outbreak. Suffering from foodborne diseases present an estimated 47. 8 million annual numbers of illnesses, 127.839 annual hospitalizations and 3.037 annual numbers of deaths transmitted through contaminated food. These estimates are due to 31 pathogens and unspecified agents transmitted through food. Officials from public health departments explore to gather facts about foodborne illnesses epidemic to control or manage them, so that there is no spreading of the disease to other people, and to acquire knowledge on how to stop similar incidences from occurring in the future. According to CDC statistics, about eight hundred verified cases of L. monocytogenes infection confirmed by laboratory analysis are reported annually in the United States of America and in most cases three or four outbreak incidences are identified. The foods that typically cause these outbreaks in USA have been identifies as Mexican-style soft cheeses made with unpasteurized milk, fresh agricultural produce, deli meats and hot dogs. This makes L. monocytogenes a very dangerous foodborne pathogen for humankind and be amongst the most frequent cause of foodborne hospitalizations or deaths as a result of microbial l diseases incidences in the United States of America. However in most African countries, L. monocytogenes foodborne outbreak reports with similar information are usually not readily available to the public which makes consumers not well informed, vulnerable and at risk of contracting these diseases (Table 3).
| Country | Year | Food type | Reported death | Hospitalization | Food recall | Reported cases | States |
|---|---|---|---|---|---|---|---|
| US | 2021 | Fully cooked chicken | 1 | 3 | Yes | 3 | 2 |
| US | 2021 | Soft Cheese | 1 | 12 | Yes | 13 | 4 |
| US | 2020 | Deli Meats | 1 | 12 | - | 12 | 4 |
| US | 2020 | Mushroom | 4 | 31 | Yes | 36 | 17 |
| US | 2019 | Hard boiled eggs | 1 | 5 | Yes | 8 | 5 |
| US | 2019 | No single source | 2 | 22 | No | 24 | 13 |
| US | 2019 | Deli-sliced meats and cheeses | 1 | 10 | Yes | 10 | 5 |
| US | 2018 | RTE Pork products | 0 | 4 | Yes | 4 | 4 |
| US | 2018 | Deli Ham | 1 | 4 | Yes | 4 | 2 |
| US | 2017 | Raw milk cheeses | 2 | 8 | Yes | 8 | 4 |
| US | 2016 | Frozen vegetables | 3 | 9 | Yes | 9 | 4 |
| US | 2016 | Raw milk | 1 | 2 | Yes | 2 | 2 |
| US | 2016 | Packaged salads | 1 | 19 | Yes | 19 | 9 |
| US | 2015 | Soft Cheeses | 3 | 28 | Yes | 30 | 10 |
| US | 2015 | Ice cream | 3 | 10 | Yes | 10 | 4 |
| US | 2014 | Caramel Apples | 7 | 34 | Yes | 35 | 12 |
| US | 2014 | Bean sprouts | 2 | 5 | Yes | 5 | 2 |
| US | 2014 | Cheese | 1 | 4 | Yes | 5 | 4 |
| US | 2014 | Dairy products | 1 | 7 | Yes | 8 | 2 |
| US | 2013 | Cheese | 1 | 6 | Yes | 6 | 5 |
| US | 2012 | Cheese | 4 | 20 | Yes | 22 | 14 |
Table 3: Selected multistate cases of listeria monocytogenes outbreaks in USA from (2011-2021).
Foodborne illness complaint history
Many food health departments receive foodborne illness complaints from food retail outlet patrons that may not or often result in a follow up inspection with a food establishment’s. Food health regulators have standardized foodborne ill ness forms that review the patron’s symptoms and history to determine the likelihood that food establishment caused the illness and an outbreak investigation should be recommended to be conducted especially when two cases from different consumers of same food share the exposure. However several foodborne illnesses are not reported by consumers and therefore, the illnesses often passes uninvestigated, undetected or unnoticed. In the USA the Environmental Health Specialists Network (EHS-Net) designed a foodborne illness complaint form for state and local environmental health specialists working in food safety programs to use to capture information from consumers about their foodborne illness complaints as an effective tool for surveillance. The information obtained from this form could be helpful to decide whether a consumer with a foodborne infection complaint should be looked into as potentially connected or related to a foodborne illness outbreak. Foodborne illness complaint systems are an effective surveillance tool for detecting foodborne listeriosis illnesses. Collecting complaints of suspected foodborne illness allows public health agencies to detect potential outbreaks sooner and implement control and education measures to prevent more people from getting sick. Commonly collected data include name and contact information of the complainant, demographics, information about their illness, suspected food product or establishment, names and contact information for other members of the dining party, and non- foodborne exposures, such as swimming [16-20].
Foods more likely to be contaminated with L. monocytogenes
Foods that are usually implicated or contaminated with L. monocytogenes include Ready To Eat (RTE) processed meat products, dairy products especially those that are not heat treated, raw foods of plant origin, seafood, a variety of prepared salads and food from vendors. Adequate standard heat treatment of foods and most disinfectants commercially available destroys L. monocytogenes, but however, contamination may occur post production before packaging particularly in some (RTE) processed foods that are usually consumed without further pre-heating such as deli meats, burgers, hot dogs, meat pies and freshly prepared fruit salads. Some of these products can be safely consumed after a thorough reheating until steaming hot. According to the Food Safety and Inspection Service (FSIS) in the United States department of agriculture, a zero tolerance policy is maintained for occurrences of L. monocytogenes in (RTE) processed meat products with recommendations and programs to strengthen the reduction or elimination of the foodborne pathogen from all (RTE) products. However in most developing countries particularly in Sub- Saharan regions such policies are rather silent and there is a lack of available literature of surveillance documented reported cases. As a result L. monocytogenes incidences may occur in these nations and pass without documentation or investigation, but consumers continue to be exposed due to consumption of contaminated food stuffs. The human health afflictions as a result of this pathogenic organism have a remarkable economic loss and public health impact for society and food manufacturers. Incidences of L. monocytogenes and cases of food recalls from retail establishments are indicators of the presence of this pathogen in these outlets and elimination or total control of this organism from these facilities after outbreaks and recalls is questionable. Detection of L. monocytogenes in food outlet facilities is always used as an indicator to confirm the presence of the conditions necessary for presence, proliferation and persistence of this important human foodborne pathogen L. monocytogenes can hide in many foods and most outbreaks were primarily linked (in the 1990’s) to deli meats and hot dogs. However nowadays L. monocytogenes cases are often linked to RTE products, dairy products and fresh produce such as cold meat processed, cheeses, ice creams sprouts etc. Sometimes no single sources or specific food items, shops, food retail establishment facilities are single out as the sole source of contamination during outbreaks. Thus L. monocytogenes is now associated with several foods which were traditionally not linked to it.
People who are most targets of L. monocytogenes
Foodborne listeriosis is a serious life threatening but treatable and preventable infection. Pregnant women, newborns, people with 65 years and older and anyone with compromised immunity systems (such as those with a weakened immune system due to conditions like HIV/AIDS, renal failure, cancer or any chronic health condition) as well as new born babies are at high risk of inhospitable effects of listeriosis and should keep away from consumption of high risks implicated food products. Listeria infections are particularly dangerous for pregnant women and it’s possible for unborn babies to catch the infection from their mothers. Pregnant women are also 10 times trusted source more likely to get a Listeria infection than non-pregnant women or men and this type of infection usually develops within a several days after eating contaminated food. In pregnant women, it can take much longer. Others often have symptoms of: headaches, confusion, loss of balance, seizures, fever, fatigue, muscle aches. Symptoms during pregnancy include fever, muscle aches, and fatigue and complications include miscarriage, stillbirth, premature birth, and infection in a newborn. L. monocytogenes are ubiquitous in the soil, vegetation, water, waste droppings of some animals and can easily contaminate foods at any point in the farm to folk production chain. Consumption of implicated contaminated foods with high counts of this pathogen is the main route of transmission of in infections and foodborne outbreaks due to L. monocytogenes occur in all countries although most case seems to pass unreported or unnoticed in several nations (Figure 1).
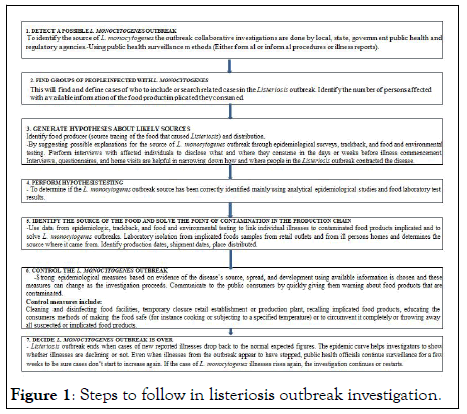
Figure 1: Steps to follow in listeriosis outbreak investigation.
Listeria monocytogenes outbreak subtypes are isolated from samples from equipment, production establishment facilities such as packing facility in the retail establishments involve and public health in areas or places where incidences of illnesses recorded to determine the cause of contamination linked to the outbreak.
Post foodborne listeriosis outbreak
Those retailers and food traders unaware of the listeriosis outbreak or recall could continue to sell, eat or serve contaminated foods to consumers. When an outbreak investigation is declared to be over, humankind could continue to be infected with L. monocytogenes because recalled food products may still be in homes, shops, restaurants or retail locations. In Zimbabwe after the United Nations World Health Organization called the (2017-2018) South Africa listeriosis outbreak the largest ever recorded globally, the government through the health and child care ministry has temporarily banned the importation of all polony, Vienna and Russian sausages and other implicated RTE processed meat products imported from this country in a bid to curb the spread of the deadly disease (Ministry of Health, 2018). However most people in their homes or retail establishments were not aware of the situation on the ground or public health official’s measures and continued with distribution and consumption of contaminated food products. Facilities where surveillance will be taking place to confiscate, destruct or quarantining implicated food products such as border posts (for imported products) usually have no capacity to specify whether the food products or holding facilities are certified free from infection. This poses serious risk of continual spreading of the pathogen even if the specified food production establishment is certified to be free from the infection. Overall steps to totally eliminate L. monocytogenes in homes and retail establishments are very difficult to follow and there are usually no laboratory or qualified certified food scientists to test the presents or absence of L. monocytogenes in the shops, home or vendors. Thus why L. monocytogenes is a serious foodborne pathogen of public health and food safety concern which remain very difficult to eradicate in all retail establishments. Usually public health officials make announcements through national broadcasting channels, but the message is only received with those with access to the information the majority continue to transmit the pathogen through distribution or consumption of contaminated products. Those in remote areas can continue distributing and consuming L. monocytogenes contaminated products. Most consumers may fail to supply evidence of what they ate and usually do not keep food receipts from stores or restaurants and will not voluntarily approach healthcare provider about whether they should be tested for a foodborne disease. As a result most incidences of listeriosis pass unnoticed, not reported to health care providers or undetected and the pathogen remains in the environment living with people. Consumers can purchase some recalled contaminated foods unknowingly instead of not eating them or throwing away and continue to be exposed to the risk of contracting the disease. When no statistical association between a food and illness is found, it does not mean the illness or outbreak was not foodborne. It means only that the source could not be determined. If the outbreak has ended and the source of the outbreak is declared unknown, people may still continue to get sick so investigators must keep gathering information and studying results to find the food that is causing the illnesses.
Guidance for L. monocytogenes prevention among persons at risk
Eating food contaminated with the bacterium L. monocytogenes can cause a potentially life-threatening, invasive disease called listeriosis. Women who are pregnant, adults with age above 65 years, and individuals with compromised immune systems as a result chronic medical illnesses or treatment are more vulnerable to listeriosis infection. The symptoms include fever, headache, stiff neck, confusion, loss of balance, and convulsions. Pregnant women might experience only mild illness; however, listeriosis during pregnancy can lead to miscarriage or stillbirth, premature delivery, or life-threatening infection of the newborn. Centers for Diseases Control and Prevention (CDC), the U.S. Department of Agriculture (USDA) Food Safety and Inspection Service (FSIS), and Food and Drug Administration (FDA) recommend that risk persons and those who prepare meals for risk persons adhere to food safety principles. The general guidelines recommended for the prevention of listeriosis are similar to those used to help prevent other foodborne illnesses, such as Salmonellosis. Consumers should pay attention to high risk foods and they should not consume foods like hot dogs, lunch meats, cold cuts, other deli meats (e.g., bologna), or fermented or dry sausage, unless they are reheated to 74℃ or until steaming hot just before serving. Refrigerated smoked seafood, pate or meat spreads from a deli or meat counter or from a refrigerated section of the retail outlet should not be consumed. Foods that do not need refrigeration, such as canned or shelf-stable pate and meat spreads should be refrigerated after opening (W. Consumers should not consume raw (unpasteurized) milk, foods that have unpasteurized milk in them, soft cheeses unless made from pasteurized milk. Raw foods from animal sources (such as beef, pork, or poultry) should be thoroughly cooked, raw or fresh vegetables produce should be thoroughly washed before consumption and uncooked meats should kept separate from vegetables, cooked foods or RTE foods. Hands, knives, and cutting boards must be cleaned after handling uncooked foods. Persons at high risk, such as pregnant women and persons with weakened immune systems should more careful and selective on the type of foods to consume. When consumers follow these steps to minimize contamination of food by the Listeria bacterium, listeriosis cases can be greatly reduced. When a processed food is implicated to be contaminated with L. monocytogenes bacteria, food monitoring and establishment facilities inspection are intensified, and if necessary, the implicated food is recalled. Early detection and reporting of outbreaks of foodborne listeriosis to local and state health departments can help identify sources of infection and prevent more cases of the disease.
Deepening laboratory analysis of foodborne L. monocytogenes
Food producers, processors, and distributors should increasingly use rapid microbial laboratory methods to get rapid results to mesh with their just in time supply. To meet this demand, food processing organizations and retail establishments should embrace developed and marketing simple, user friendly developed tests that can be rapidly performed at the processing facilities or in the field by relatively untrained personal primed and ready to replace conventional culture and novel molecular screening methods, biosensor based analyses using specific biomarkers such as nucleic acids, proteins, antigens, and metabolic products are the third wave of microbial detection systems. These kits and biosensor formats target the food industry’s goal of quickly and inexpensively monitoring safety and quality, then moving the product out the door. But before the food establishments slash testing budgets, stakeholders should consider a reversion change in food safety and agricultural research where foodborne L. monocytogenes testing should go not only faster but deeper. Deep means including sequencing. Conventional methods currently widely used especially in developing nations for food safety tests, unfortunately, have significant drawbacks for identifying all the individual species in a microbiological community. Not all microbes will grow in a lab environment, and some damaged or stressed organisms may be viable but not cultivable. Colony counting methods cannot reliably enumerate or identify microbial cells such as spores, which tend to aggregate and clump when plated. Different food matrices are challenging for culture methods, and spices, herbs, chocolate, and vitamin and mineral premixes are known to inhibit microbial growth and confound the reading of culture. Deep L. monocytogenes laboratory analysis by sequencing circumvents conventional cultural methods limitations by going directly to nucleic acids such as DNA and RNA for identification. Discovering and cataloging the diversity of L. Monocytogenes pathogenic servers and strains, micro biomes, biofilms, and other microbial communities may help prevent recalls, mitigate outbreaks, assist in the discovery of antimicrobial resistant microbes, and point to contaminants, formulation, or environmental changes. Sequencing technologies has also become more affordable and are readily available in many parts of the world where they can be very useful to understand more about L. monocytogenes strains genetics and foodborne outbreaks surveillance. High-through sequencing of total DNA and total RNA is leaving the realm of academics and moving into use in food industry. In addition, novel technologies such as CRISPR-SeroSeq provide deeper information.
Over view of whole genome sequencing as a tool for foodborne pathogen identification
Whole genome sequencing is a process that uses laboratory methods to determine the complete DNA sequence of an organism’s genome. It is a new nucleic acid technology used by research and public health laboratories to generate DNA fingerprints of bacteria causing illness. When bacteria have nearly identical DNA fingerprints, they are considered genetically closely relate. Illnesses caused by bacteria that are genetically closely related are more likely to have come from a common source, such as contaminated food. An outbreak is an event in which a group of people get similar illnesses from a common source. Disease detectives investigate outbreaks to find out what is making people sick. WGS an advance technology is now used to find, stop outbreaks and combat drug resistant microbes, providing detailed genetic information about pathogens. Regulatory authorities and researchers use this information to improve efforts to find, investigate and prevent illnesses caused by pathogens. This is very important especially when looking for the source of an outbreak or predicting drug resistance in the pathogens. Through use of WGS highly detailed and timely information that helps in the protection of public health can be provided which results in improvements of detection and investigation of foodborne outbreaks. With WGS, L. monocytogenes outbreaks can be detected when as few as two individuals have gotten sick. Determining that the same strain of L. monocytogenes is making people sick is an indication that these illnesses may have come from the same source for example, the same contaminated food or the same contaminated food processing facility. Thus, WGS can help disease investigators solve outbreaks. By combining WGS with data from patients about the foods they consumed and data about L. monocytogenes in implicated food products, public health officials can detect more clusters (possible outbreaks) of listeriosis infections, link cases to a likely source, identify unrecognized sources of the pathogen and be able stop foodborne outbreaks while they are still small microbial nucleic acids sequencing need to be harnessed by food processing establishments as technology for the future food microbial analysis. As powerful technologies such as sequencing become affordable for routine use, more food producers, processors and distributors will take advantage of the deep and predictive capabilities of these molecular detection methods. Partnered with bioinformatics ices, DNA and RNA sequencing can provide more complete microbial profiles and coherent histories. These data are not only predictive but diagnostic, allowing the food production chain-from farm to table to uncover hidden problems.
Control measures for L. monocytogenes foodborne outbreaks in retail establishments
The control of L. monocytogenes is required at all stages in the food chain and an integrated approach is needed to prevent the multiplication of these bacteria in the final food product. The challenges for controlling L. monocytogenes are considerable given its ubiquity us nature, high resistance to common preservative methods, such as the use of salt, smoke or acidic condition in the food, and its ability to survive and grow at refrigeration temperatures. All sectors of the food chain should Implement Good Hygienic Practices (GHP) and Good Manufacturing Practices (GMP) as well as implement a food safety management system based on the principles of Hazard Analysis Critical Control Points (HACCP). There are numerous risk factors that contribute to the contamination, growth, and spread of L. monocytogenes in retail establishments. Therefore, an integrated approach for control of the pathogen should be applied along the whole food chain continuum, including up to retail. Well-designed control measures should be synergistically applied at multiple points in the whole food production chain, that is, preproduction, production, and post- production including retail to eliminate, prevent, and/or reducing the introduction or occurrence of L. monocytogenes. In addition, selection and implementation of anti-listeria control measures should be based on scientific evidence, for example, literature, validation studies, predictive microbiology (statistically designed surveys and/or mathematical modeling) and these studies should provide scientific proof that anti-listeria control measure can effectively reduce the number of L. monocytogenes in environment/food contact surfaces and RTE products. The specific control measures should be applied to effectively prevent and/or minimizes the presence of L. monocytogenes in retail establishments. The three essential measures for control of L. monocytogenes are (a) Prevent cross-contamination, (b) Practice proper sanitation or good hygiene practices, and (c) Control time and temperature. Routine inspection by health authorities takes place in Europe facilities where samples are collected for laboratory analysis but, documentation reports of routine inspection in African food production are not readily available for consumers. Inspections will usually only be done after an alarm of an outbreak and some foodborne outbreaks can go unnoticed. Sanitary conditions of production facilities need to be observed frequently by regulatory authorities. It will be imperative to suspend the food facility registration. So that the implicated company cannot continue to distribute any contaminated food products to reach consumers. Food safety regulatory authorities should work closely with implicated food producers to review the firm’s corrective actions before the firm is authorized to resume product production. All foreign food traders implicated should be reported, published and put on import alert. This means the products will be denied admission into the country until the importer shows or certifies that the product is no longer contaminated. The food organization should issue an expanded recall of all lots and production codes, a market withdrawal of all products received that were produced by the exporter. In retail shops wash and sanitize any food contact surfaces and containers that may have come in contact with the recalled products because L. monocytogenes can survive in refrigeration temperatures and can easily spread to other foods and surfaces, this increases chances of cross contamination. Wash surfaces with hot soapy water or in the dishwasher, wash containers with hot soapy water, use a solution of 1 table spoon of liquid bleach in 1 gallon of water after cleaning with hot water to sanitize surfaces and containers.
It is recommended that food processors, retailers and restaurants who received implicated food products, should use extra vigilance in cleaning and sanitizing any surfaces and containers that may have come in contact with these products to reduce the risk of cross contamination. Swabs from all cleaned food contact surfaces or containers should do for laboratory confirmation that the facilities are free from L. monocytogenes. Without laboratory confirmation, L. monocytogenes can continue to survive in the food retail establishment facilities and consumers continue to be exposed to the risk of listeriosis illness. The world health organization promotes the strengthening of food safety systems, good manufacturing practices and educating retailers and consumers on appropriate food handling and to avoid cross contamination. Educating consumers, especially those in high risk groups, and training of food handlers in safe food handling are among the most critical means to prevent foodborne illnesses including listeriosis. Investigations have found a variety of causes for these outbreaks, yet many never have a food vehicle identified or determine how the food became contaminated.
Listeria monocytogenes is a foodborne pathogen which is very difficult to control in food services establishments. It is very difficult to ascertain absents of this foodborne pathogen after a foodborne outbreak or food recall since most retail food establishments lacks laboratory facilities for confirmatory. Listeria monocytogenes has been associated with a number of foodborne illness outbreaks and has been rated to be amongst the leading cause of death from food poisoning. Foodborne illness outbreaks are investigated to control them, so that more people do not get affected in the outbreak, and to learn how to prevent similar outbreaks from happening in the future (WHO, 2008). Consumption of food contaminated with these dangerous foodborne bacteria will usually cause illness within 1 to 4 weeks of ingesting the contaminated food. However, it can take up to 70 days after exposure for sickness to manifest or symptoms of L. monocytogenes infection to be evident. This pathogen has proven to be very challenging to control and has a higher mortality rate when people become ill than other pathogens. Bacterial communities of mo. L. Monocytogenes are complex and constantly evolving due to changes in the environment, available growth matrices, and growth factors such as pH, water activity and temperature. Over time, certain strains tend to predominate becoming more abundant or resilient than others. Although most people will recover from a foodborne illness within a short period of time, some can develop chronic, severe, or even life-threatening health problems and foodborne illness can sometimes be confused with other illnesses that have similar symptoms. Those retailers and food traders unaware of the listeriosis outbreak or food recalls could continue to sell eat or serve contaminated foods to consumers even if the investigation is declared to be over and humankind could continue to be infected with L. monocytogenes because recalled food products may still be in homes, shops, restaurants or retail locations. Customers and vendors may carry microorganisms on their shoes, clothing, and hands and can transfer them to shopping baskets, trollies and foods during their shopping visits. Therefore, an integrated approach should be applied along the whole food production and distribution chain for the effective control of L. monocytogenes at retail. Listeria monocytogenes is ubiquitous, can survive in thriving environments that are unfavorable for other pathogens to proliferate (such as vacuum packaged products), refrigerated temperatures and can easily cross contaminate to spread to other food products and food contact surfaces. The actual incubation period has not been determined for the foodborne illness caused L. monocytogenes. Healthy people may not have symptoms or may only have mild symptoms when exposed to this pathogen. However consumers at higher risk (pregnant women, newborn, elderly people and those immune-compromised), if they become ill from Listeria monocytogenes, are at greater risk of more severe symptoms, hospitalization or death. Consumers at higher risk for listeriosis illness should be aware that although pasteurization of food products kills L. monocytogenes, pasteurized products can still become contaminated and cause listeriosis outbreaks. Therefore individuals at higher risk of contracting this foodborne illness should take extra precautions such as avoiding foods that have been mostly implicated in listeriosis outbreaks (WHO Africa, 2018). To reduce the potential spread of L. monocytogenes additional control measures may be required for persons associated with high-risk activities or settings such as food handlers, childcare facility personnel, and health care workers. Because of the long incubation period, anyone who has eaten any of the implicated food products should monitor themselves in the coming weeks for signs of infection. Food contaminated with L. monocytogenes may not look or smell spoiled but can still cause serious and sometimes life-threatening infections. Anyone who consumed any recalled product and developed symptoms of Listeria infection should seek medical treatment and tell their doctors about the possible L. monocytogenes exposure [18]. However several consumers do not register or publicize foodborne illnesses and therefore, most cases often pass uninvestigated, not reported, undetected or unnoticed. In most African countries, reports with similar information similar to these foodborne outbreaks are usually not readily available to the public which makes consumers not well informed, vulnerable and at risk of contracting these diseases. An integrated approach for control of L. monocytogenes should be applied along the whole food chain continuum, including up to retail. Well-designed control measures should be synergistically applied at multiple points in the food chain, that is, pre-harvest (on farm, transportation), harvest (slaughter, dairy plant), and post-harvest (food processing, retail) to eliminate, prevent, and/or minimize the introduction and occurrence of L. Monocytogenes. Food processing organizations and retail establishments should embrace developed and marketing simple, user-friendly developed tests that can be rapidly performed at the processing facilities or in the field by relatively untrained personnel. As powerful technologies such as sequencing become affordable for routine use, more food producers, processors and distributors will take advantage of the deep and predictive capabilities of these molecular detection methods. Partnered with bioinformatics, DNA and RNA sequencing can provide more complete microbial profiles and coherent histories. These data are not only predictive but diagnostic, allowing the food production chain-from farm to table to uncover hidden problems. Listeria monocytogenes should be considered a serious food hazard in retail establishments. To protect customers and to protect the business, operators of retail establishments should implement a program to control Listeria monocytogenes. Understanding the sources of the pathogen and factors that contribute to the risk of contamination, growth and spread of the pathogen are important building blocks to an effective control program. The implementation of proper prevention and control measures, verification and monitoring procedures, and a maintenance program will help to ensure that L. monocytogenes does not contaminate your product. An effective control program is the best defense against this foodborne pathogen [19]. Diagnosis of foodborne listeriosis can only be confirmed if the etiological agent is isolated and identified from ill individuals and this is particularly important when the clinical diagnosis is difficult to make because signs and symptoms are nonspecific, as is the case with many foodborne diseases [20].
Material is in this manuscript partially based upon work supported by US CDC and FDA as well as unrestricted information from available literature.
This review paper does not contain any research studies with animals or human participants conducted by the authors.
Conceptualization and writing of original draft preparation were done by Francis Manjengwa. Writing and visualization were done by Francis Manjengwa, Dr L Nyanga, Dr E Guchu and Dr S Mambo (Authors). All authors contributed to the manuscript, validation investigation, resources, data creation, writing, review and editing. All the authors have read, approved the final document and agreed to publish the typescript.
This research received no external funding but the work reported in this manuscript is supported by Centres for Disease Control and Prevention (CDC), National Centre for Emerging and Zoonotic Infectious Diseases (NCEZID), Division of Foodborne, Waterborne, and Environmental Diseases (DFWED) and available literature from unrestricted sources. Any point of view, discovery, conclusions or suggestions and submissions expressed in this proclamation are views of the authors
The author declares no conflict of interest. The writing of the manuscript and the decision to publish, or interpretation facts are independent of supporting institutions.
[Crossref]
Citation: Manjengwa F (2022) A Review of Listeria monocytogenes Foodborne Outbreaks: In Retail Food Facilities after Foodborne Outbreaks Product Recalls. Food Microbial Saf Hyg. 7:183.
Received: 16-Jun-2022, Manuscript No. Jfmsh-22-17958; Editor assigned: 20-Jun-2022, Pre QC No. Jfmsh-22-17958(PQ); Reviewed: 04-Jul-2022, QC No. Jfmsh-22-17958; Revised: 16-Aug-2022, Manuscript No. Jfmsh-22-17958(R); Published: 23-Aug-2022 , DOI: 10.35248/2476-2059.22.7.183
Copyright: © 2022 Manjengwa F. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.