Journal of Leukemia
Open Access
ISSN: 2329-6917
ISSN: 2329-6917
Mini Review - (2022)Volume 10, Issue 2
Plasma Cell Leukaemia (PCL) is a plasma cell dyscrasia, or a disease characterized by the malignant degeneration of plasma cells, a type of white blood cell. It is the most advanced and dangerous stage of these dyscrasias, accounting for 2% to 4% of all instances of plasma cell malignancies. PCL can manifest as either primary plasma cell leukaemia (in patients who have never had a plasma cell dyscrasia) or secondary plasma cell dyscrasia (in patients who have previously been diagnosed with multiple myeloma). Plasma Cell Leukemia (PCL) is a rare and aggressive kind of plasma cell dyscrasia that can develop from scratch (Primary Plasma Cell Leukaemia) or evolve from multiple myeloma that has already been detected and treated (secondary PCL). As a reminder of this diagnosis, we give three clinical examples with extremely distinct appearances. The cases also indicate the length and variability of a patient's journey, which is heavily reliant on financial capability and social support. Because the higher tumour load and more proliferative tumour cells, the clinical presentation is more aggressive, with more cytopenias and organomegaly. The diagnosis is based on the presence of circulating plasma cells in at least 20% of total white blood cells and a peripheral blood absolute plasma cell count of at least 2 109/l. In those who are transplant eligible, treatment with new medications followed by autologous stem cell transplant leads to better results.
Plasma cell leukaemia; Myeloma; Diagnosis; Clinical presentation
Signs and symptoms Primary Plasma Cell Leukaemia (pPCL)
Primary PCL (pPCL) has a far more aggressive clinical presentation than a typical multiple myeloma case, with clinical features that are a combination of those seen on the multiple myeloma and acute leukaemia. [1] In 28%-56%, 4%-7%, 23%-44%, and 0%-12%, of cases, pPCL patients exhibit pathologically high amounts of monoclonal plasma cells in their bone marrow, as well as a malignant plasma cell-secreted circulating monoclonal myeloma protein, either IgG, IgA, a light chain, or none. Due to the invasion of these tissues by plasma cells and/or the deposition of their circulating monoclonal immunoglobulin in them, pPCL patients had higher frequency of splenomegaly, lymphadenopathy, hepatomegaly, kidney failure, bone marrow failure (i.e. thrombocytopenia, anemia,and/or, rarely, leukopenia), central nervous system defects, and peripheral neuropathies, similar to B cell leukaemia.
• pPCL patients have higher rates of developing hypercalcemic crisis, that is a potentially life-threatening episode of high ionic calcium (Ca2+) levels in the blood due to excess bone reabsorption and/or renal failure;
• Higher levels of serum lactate dehydrogenase and Beta-2 microglobulin;
• Lower rates of bone but higher rates of soft tissue plasma cell tumours called plasmacytomas when compared to multiple myeloma [2,3].
Signs and symptoms of Secondary Plasma Cell Leukaemia (sPCL)
Secondary PCL (sPCL) is diagnosed in 1-4 percent of patients who have been diagnosed with multiple myeloma for at least 21 months. These patients' myeloma disease is in its latter stages. Patients with sPCL usually have a lot of symptoms because they have a lot of disease, which includes malignant plasma cell infiltrations in and failures of not only the bone marrow but also other organs. They have failed or broken through one or more treatment regimens, and so as a result, they may show some of the treatment toxic effects [4].
Causes of plasma cell leukemia
PCL is caused by the development of large number of genetic abnormalities forming in plasma cells or, more particularly, their precursor B cells and plasma blasts. Gene mutations, single nucleotide polymorphisms, depletions and duplications of parts of a gene, larger portions of a chromosome, or even an entire arm of a chromosome; translocations, deletions, and duplications of entire chromosomes; and increases and decreases in the expression of intact genes due to, for example, methylation of gene promoters and various less direct effects all contribute to this genetic instability. The Wnt signaling system, cell cycle regulation, RNA metabolism, protein folding, and cadherin-related adhesion to the extracellular matrix all are affected by these genetic abnormalities.
These effects, in turn, control plasma cell proliferation, survival, apoptosis, bone marrow adhesion, genome stability, and monoclonal immunoglobulin secretion. [5] Secondary Plasma Cell Leukaemia (sPCL) is caused by the relatively slow development of genetic abnormalities in plasma cells/plasma cell precursor, which initially create a clone of cells that cause the premalignant condition of monoclonal gammopathy of clinical significance. “S” moldering multiple myeloma, overt myeloma cancer, and ultimately sPCL are produced by the development of further genetic abnormalities that create a clone (s) of plasma cells in a very small percentage of these cases [6].
In contrast to sPCL, pPCL presents with a broad range of genetic abnormalities from the beginning. For example, at the time of diagnosis, advanced methods for examining the genome, such as whole-exome sequencing and gene expression profiling, identified 166 non-silent gene variants per pPCL patient sample. These abnormalities are similar but not identical to those detected in sPCL, and the abnormalities detected in sPCL are more closely related to those detected in multiple myeloma than those detected in pPCL: The genetic data support the clinical data, suggesting that sPCL and pPCL are distinct diseases, with sPCL being more closely related to multiple myeloma than pPCL [7,8]. Examination of specific cell surface antigens, particularly cluster of differentiation, to examination of the immune phenotype of plasma cells.
CD markers on plasma cells from patients with pPCL differ from those on plasma cells from individuals with multiple myeloma or sPCL. For example, pPCL plasma cells express CD20 antigen more frequently than plasma cells from myeloma patients (50% vs. 17%); pPCL plasma cells lack CD56 antigen, which is present on the majority of plasma cells from multiple myeloma patients; and pPCL plasma cells express CD28 more frequently than sPCL plasma cells. Thus, immunophenotyping supports up the idea that multiple myeloma, sPCL, and pPCL have basic differences that might explain their differences in clinical presentations, relevant changes, and prognoses. [9,10].
Diagnosis of plasma cell leukemia
The International Myeloma Working Group has defined diagnostic criteria for plasma cell leukaemia as >2 × 109 plasma cells per liter in blood or >20% of nucleated blood cells being plasma cells. More recently, the Group has suggested that values of 0.5 × 109 or 5%, respectively, may be more therapeutic appropriate and so should be studied as a definitive criterion for the disease [1]. Multiple myeloma patients with >5% circulating plasma cells had a prognosis that was significantly worse than that of multiple myeloma patients and similar to that of plasma cell leukaemia, as shown in a recent study [2].
Flow cytometry immunophenotyping of blood cells to detect clonal morphologies of plasma cells found in multiple myeloma (e.g. the CD138+, CD38+, CD19-, CD45± phenotype) may provide a more sensitive way of counting circulating clonal plasma cells and diagnose plasma cell leukaemia (Figure 1).
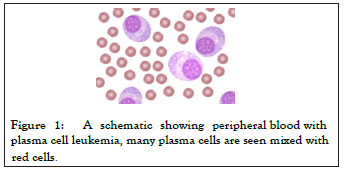
Figure 1: A schematic showing peripheral blood with plasma cell leukemia, many plasma cells are seen mixed with red cells.
Treatment
Even when treated aggressively with the VAD regimen of vincristine, doxorubicin, and dexamethasone or the VCMP regimen of Vincristine, Carmustine, Melphalan, and Prednisone alternating with vincristine, carmustine, doxorubicin, and prednisone, median survival rates for pPCL and sPCL were 8-11 months and 2-8 months respectively, prior to the use [1,5].
The use of newer ways to treat PCL patients, particularly pPCL patients, appears to have resulting in modest improvements in survival rates. Individual studies have already been limited to case reports on a small number of patients or retrospective analyses of patient records related to the rarity of these two leukemias. There have been no randomized control trials on these patients. Patient selection bias is a weakness in these procedures, in which individuals selected for treatment with a new regimen may be less ill than average patients with the disease and so have a disease that's also intrinsically less aggressive (i.e. had a longer overall survival time) [4].
Treatment of primary plasma cell leukemia: Treatment regimens that include a proteasome inhibitor drug, particularly bortezomib, and/or autologous stem-cell transplantation have improved pPCL survival, according to recent case report studies. For example, 28 patients treated a bortezomib-based induction regimen followed by autologous stem-cell transplantation and then a maintenance regimen of lenalidomide (an immunosuppressant related to thalidomide), bortezomib, and dexamethasone (a corticosteroid) had a progression-free survival rate of 66% after three years and an overall survival rate of 73 percent after four years. In one trial, patients who received intensive chemotherapy plus autologous stem-cell transplantation had a median survival of 34 months, compared to 11 months for those who receive chemotherapy alone.
Autologous stem-cell transplantation also was found to improve results in two other studies that included bortezomib in their chemotherapy regimens. Induction with a three-drug regimen such as borezomib-lenalidomide-dexamethasone, autologous stem-cell transplantation, and consolidation/maintenance with a combination of immunomodulator agents (e.g. thalidomide, lenalidomide, or pomalidomide) plus a proteasome inhibitor (bortezomib, ixazomib, or carfilzomib) plus [4,10].
Treatment of secondary plasma cell leukemia: As the end stage of multiple myeloma that has failed or broken through one or more therapeutic regimens, sPCL continues to be highly refractory to various treatment regimens (50 percent), with very short response times and poor overall survival rates (median survival of 2-8 months) [1,5]. Patients with sPCL may have shortterm responses to bortezomid-containing therapy regimens (as reported in case reports), but no established therapeutic regimens have been found to increase overall or median survival [4,10].
Plasma cell leukaemia is a rare and aggressive form of plasma cell dyscrasia that needs early diagnosis and aggressive treatment before patients develop problems. Given the poor prognosis, new medicines should be used as part of the induction regimen, followed by autologous transplantation in individuals who are transplant eligible. Despite improvement in diagnostics and treatment, patients in Sub-Saharan Africa face challenges, while the treatment options are limited by the ability to afford and access to services.
[CrossRef], [PubMed], [Google Scholar]
[CrossRef], [PubMed], [Google Scholar]
[CrossRef], [PubMed], [Google Scholar]
[CrossRef], [PubMed], [Google Scholar]
[CrossRef], [PubMed], [Google Scholar]
[CrossRef], [PubMed], [Google Scholar]
[PubMed], [Google Scholar]
[CrossRef], [PubMed], [Google Scholar]
[CrossRef], [PubMed], [Google Scholar]
Citation: Erfani S (2022) A Review on Plasma Cell Leukemia. J Leuk. 10: 291.
Received: 07-Feb-2022, Manuscript No. JLU-22-15764; Editor assigned: 09-Feb-2022, Pre QC No. JLU-22-15764(PQ); Reviewed: 23-Feb-2022, QC No. JLU-22-15746; Revised: 28-Feb-2022, Manuscript No. JLU-22-15764(R); Published: 07-Mar-2022 , DOI: 10.35248/2329-6917-22.10.291
Copyright: © 2022 Erfani S. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.