Journal of Clinical and Experimental Ophthalmology
Open Access
ISSN: 2155-9570
ISSN: 2155-9570
Research Article - (2022)Volume 13, Issue 7
Background: CSCR is a sporadic disorder of the outer blood retinal barrier, characterized by a localized detachment of sensory retina usually affecting one eye in young males. Usually, a self-limiting disease various treatment have been investigated in recent times.
Aim: To evaluate the final visual outcome, recurrence rate and possible complications in patients of CSCR treated with observation, oral Acetazolamide, oral Eplerenone and double frequency ND-YAG laser photocoagulation.
Methods and materials: A prospective interventional study was done on patients newly diagnosed with CSCR. The study comprised of 76 patients who were divided into four groups namely Group A on observation, Group B on oral Acetazolamide Group C on oral eplerenone and Group D on Nd-YAG Laser. Visual recovery, recurrence rate and possible complications of these therapies were compared.
Results: Group D patients showed fastest improvement in visual acuity at 2 weeks. At 12 weeks all groups had comparable improvement. 3 patients in group A, 1 each in group B and D and 2 in group C showed recurrence. Paraesthesia, numbness and gastric upset related to acetazolamide were noted in 5 patients of group B. 16.7% cases in group A, 10.5% in group B, 5.3% in group C and 5% in group D showed leakage on FFA after 12 weeks.
Conclusion: In acute CSCR eplerenone seems to be efficient with least side effects and early resolution. In chronic cases ND-YAG Laser seems to give better result. Early treatment should be given for better visual recovery of patients.
Chorioretinopathy; Paraesthesia; Numbness
CSCR is a sporadic disorder of the outer blood retinal barrier, characterized by a localized detachment of sensory retina at the macula secondary to focal Retinal Pigment Epithelial (RPE) defects, usually affecting one eye [1]. It is usually a self-limiting disease typically affecting young or middle-aged men [2]. This disease was first recognized by Albrecht von grief in 1866, who termed the condition “central recurrent retinitis” [3]. The current term of central serous retinopathy or chorio retinopathia centralis serosa” was coined by Donald Grass in late 1960’s [4]. Key features are one or more focal areas of sub-retinal fluid at the macula and one or more focal leaks at the level of RPE [5].
It is the fourth most common retinopathy after age related macular degeneration, diabetic retinopathy and branch retinal vein occlusion [6]. The male to female ratio is 8:1. People of Hispanic Asian and Caucasian descent seem to be more susceptible to CSCR [7].
Common reported risk factors and associations with CSCR are Type A personality disorder, stress, systemic hypertension, pregnancy, corticosteroids, psychopharmacologic medications, antacids and anti-reflux medications [8].
Different theories have been put fourth for the understanding of CSCR. The widely accepted theory states that there is derangement in tissue hydrostatic pressure and osmotic pressure. Under physiological conditions balance between hydrostatic pressure and osmotic pressure is responsible for driving the fluid from sub retinal space to choroid but increase in choroid vascular permeability causes flow in reverse direction [9].
Another theory is that of abnormal polarity of some RPE cells leading to fluid being pumped from choroid to retina. This concept has some weakness as it fails to explain the occurrence of Pigment Epithelium Defect (PED) [10]. However, all patients of CSCR do not develop PED.
Recent investigations strongly support the hypothesis that CSCR is primarily characterized by vascular deregulation in the choroid. In fact, choroid hyper permeability changes have been clearly shown using Fluorescein Angiography (FA) and Indocyanine Green Angiography (ICGA), [11,12] and increased choroid thickness has been demonstrated in both the affected and contralateral eyes when measured with Optical Coherence Tomography (OCT) [13,14].
The carbonic anhydrase inhibitors like acetazolamide act on RPE and helps in the resorption of the sub retinal fluid. In the specific case of CSCR, in which a deficiency of choroid blood flow has been described, carbonic anhydrase inhibitors could be effective and can increase choroid blood flow [15]. Acetazolamide given in a tapering dose for 6 weeks has been shown to reduce the time for subjective and objective CSCR resolution, but it had no effect on final Visual Acuity (VA) or recurrence rate and some had side effects as par aesthesia, nervousness, and gastric upset [16].
Laser treatment had decreased recurrence rate in CSCR [17,18]. However treatment with continuous-wave laser or Argon laser can cause tissue damage resulting in central visual field loss, loss of contrast sensitivity, and other visual issues if it is delivered in close proximity to foveal area [19]. Potential complications include thermal rupture of Bruch's membrane with haemorrhage, secondary choroid neovascularization and misplaced laser spots.
New insights into the pathogenesis of CSCR have revealed that glucocorticoid and mineralocorticoid dysfunction is also present [20,21]. In animal models, the activation of choroid mineralocorticoid receptors was shown to cause choroid vasodilation and leakage; this phenomenon was inhibited by Mineralocorticoid Receptor (MR) antagonism [22]. Based on these findings, researchers investigated the role of mineralocorticoid antagonists in the treatment of CSCR, reporting positive preliminary results [23-25]. Spironolactone and eplerenone are both oral-specific MR antagonists approved for several systemic disorders, and are commonly used for treating hypertension and congestive heart failure. However, spironolactone, although effective, is associated with various unwanted progestational and antiandrogenic side effects, such as gynecomastia, impotence and abnormal menstrual cycles, which can limit its use. Eplerenone has a lower affinity for steroid receptors (e.g., progesterone and androgen), leading to higher tolerability and specificity.
Various studies have investigated the role of these therapies individually or in combination of two for the resolution of CSCR [26-31]. However, to the best of our knowledge, no study has compared the efficacy and adverse effects of observation, oral Acetazolamide, oral Eplerenone and double frequency NDYAG laser photocoagulation for treatment of CSCR.
Hence present study was conducted to compare the efficacy and adverse effects of observation, acetazolamide, eplerenone and laser in CSCR. The study was undertaken to evaluate visual recovery, final visual outcome, recurrence rate and possible complications of these therapies.
Prospective cross-sectional interventional study was conducted on newly diagnosed patients of CSCR with clear ocular media and willing to undergo study were selected.
Methods
The study comprised of 82 patients of CSCR fulfilling the inclusion criteria out of which 6 patients were lost to follow-up, detailed history and examination was performed. Visual acuity was assessed by Snellen’s Chart, residual metamorphopsia by Amsler’s Grid, Fundus evaluation by Indirect Ophthalmoscope and 20 D lens. The study was approved by Institute Research and Ethics Committee. Informed consent was taken orally from all the subjects.
Investigations
82 patients were selected for the study. The selected patients were randomly divided into four groups. Group A comprised 20 patients was closely followed up with observation. Group B comprised 22 patients who were administered oral acetazolamide 250 mg three times a day (TDS) for 4 weeks, followed by 125 mg TDS for 4 weeks and then 125 mg twice a day for 4 weeks. Oral Eplerenone was given to Group C patients (18 patients) in dosage of 50 mg once a day for 12 weeks. Group D patients (22 patients) were treated with laser photocoagulation. 2-3 focal laser burns of 80 mW-100 mW power were applied with 200-micron spot size and for 0.1 second duration.
In all the groups FFA was done at baseline, 2 weeks, 6 weeks and at 12 weeks to see for any remaining leakage and Amsler’s Grid was used to check for any residual metamorphopsia at 12 weeks. Two patients in Group A, 3 patients in Group B and 2 Patients from Group D were lost to follow-up, hence were not included in statistical analysis.
Stastical methods
Visual acuity readings in all the 4 groups were converted into their corresponding Log Mar values for application of statistical test. Student unpaired t test was used for assessing the significance in intra and inter group observation. P value<0.05 was considered to be significant.
The most common age group of presentation was found to be 31-35 years. 40 patients out of 76 (52.6%) belonged to this age group. Male preponderance was observed with 57 males and 19 females.
Visual acuity improved in all the groups with time by the end of 12 weeks which was greater in group C and D. Moreover, there was very significant improvement in Group C and D at two weeks. Fastest improvement was seen in group D patients where vision improved in most patients within 2 weeks (Table 1 and Figure 1).
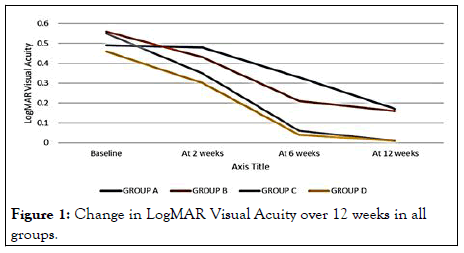
Figure 1: Change in LogMAR Visual Acuity over 12 weeks in all groups.
| AGE (yrs.) | A | B | C | D |
|---|---|---|---|---|
| <30 | 1 | 4 | 3 | 2 |
| 31-35 | 10 | 12 | 10 | 9 |
| 36-40 | 4 | 2 | 4 | 5 |
| >40 | 3 | 1 | 2 | 4 |
Table 1: Age distribution.
The most common age group of presentation was found to be 31-35 years (Table 1).
At 12 weeks 5 patients in group A and 2 patients in group B& C and 1 patient in Group D had some residual metamorphopsia (Table 2).
| Sex distribution | A | B | C | D |
|---|---|---|---|---|
| Male | 15 | 14 | 14 | 14 |
| Female | 3 | 5 | 5 | 6 |
Table 2: Sex distribution.
Out of 76 patients 57 were males and 19 were females (Table 2).
At baseline 76 patients in all the 4 groups showed leakage on FFA. At 2 weeks 12 patients in group A, 10 patients in group B, 4 patients in group C and 1 patient in group D showed leakage which reduced at 6 weeks in all the groups.
At the end of 12 weeks, 3 patients in group A, 2 patients in group B and C and 1 patient in Group D showed some leakage (Table 3).
| Group A | Group B | Group C | Group D | |
|---|---|---|---|---|
| Baseline | 0.49 ± 0.21 | 0.56 ± 0.18 | 0.55 ± 0.26 | 0.46 ± 0.22 |
| At 2 weeks | 0.48 ± 0.20 | 0.43 ± 0.13 | 0.35 ± 0.27 | 0.30 ± 0.21 |
| At 6 weeks | 0.33 ± 0.12 | 0.21 ± 0.06 | 0.06 ± 0.09 | 0.04 ± 0.11 |
| At 12 weeks | 0.17 ± 0.06 | 0.16 ± 0.06 | 0.01 ± 0.05 | 0.01 ± 0.02 |
Table 3: Changes in visual acuity in all groups at 2 weeks, 6 weeks and 12 weeks.
Visual acuity improved in all the groups with time by the end of 12 weeks which was greater in group C and D. Moreover, there was very significant improvement in Group C and D at two weeks. Fastest improvement was seen in group D patients where vision improved in most patients within 2 weeks (Table 3) and (Figure 1).
In group a recurrence rate was 16.6%, while it was 5.3% in group B and C, recurrence rate of 5% was observed in group D.
In group B 5 patients (26.3%) had parenthesis, numbness, gastric upset related to acetazolamide drug while none of the patients in group A, C and D showed any complications (Table 4 and Figure 2).
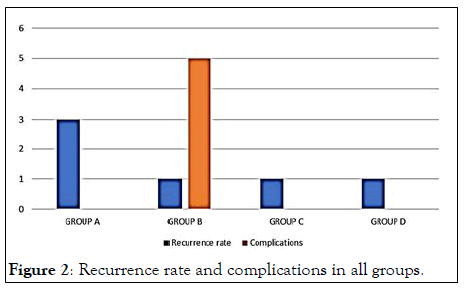
Figure 2: Recurrence rate and complications in all groups.
| Group A | Group B | Group C | Group D | |
|---|---|---|---|---|
| Baseline | 18 | 19 | 19 | 20 |
| At 2 weeks | 14 | 11 | 3 | 2 |
| At 6 weeks | 7 | 4 | 2 | 1 |
| At 12 weeks | 5 | 2 | 2 | 1 |
Table 4: No. of patients with metamorphopsia.
At 12 weeks 5 patients in group A and 2 patients in group B, C and 1 patient in Group D had some residual metamorphopsia (Table 5).
| Group A | Group B | Group C | Group D | |
|---|---|---|---|---|
| Baseline | 18 | 19 | 19 | 20 |
| At 2 weeks | 12 | 10 | 4 | 1 |
| At 6 weeks | 6 | 2 | 2 | 1 |
| At 12 weeks | 3 | 2 | 2 | 1 |
Table 5: No. of patients with leakage on FFA.
At baseline 76 patients in all the 4 groups showed leakage on FFA. At 2 weeks 12 patients in group A, 10 patients in group B, 4 patients in group C and 1 patient in group D showed leakage which reduced at 6 weeks in all the groups. At the end of 12 weeks, 3 patients in group A, 2 patients in group B and C and 1 patient in Group D showed some leakage (Table 6).
| A | B | C | D | |
|---|---|---|---|---|
| Total no. of pts | 18 | 19 | 19 | 20 |
| No. of recurrences | 3 | 1 | 2 | 1 |
| Complications | 0 | 5 | 0 | 0 |
Table 6: Recurrence rate and complications.
In group A and B recurrence rate were 16.6% and 5.3% respectively.10.5% in group C and 5% in group D showed recurrence.
In group B 5 pts (26.3%) had paresthesia, numbness, gastric upset related to acetazolamide drug while none of the pts in group C and D showed any complications related to eplerenone or laser (Figures 2-4).
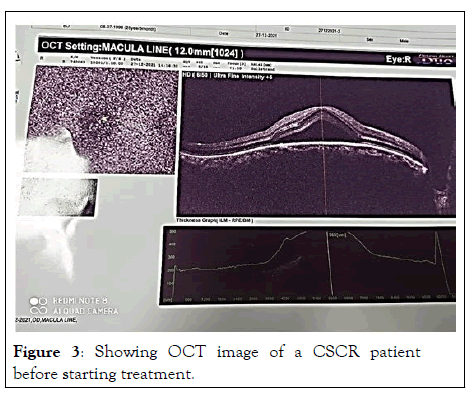
Figure 3: Showing OCT image of a CSCR patient before starting treatment.
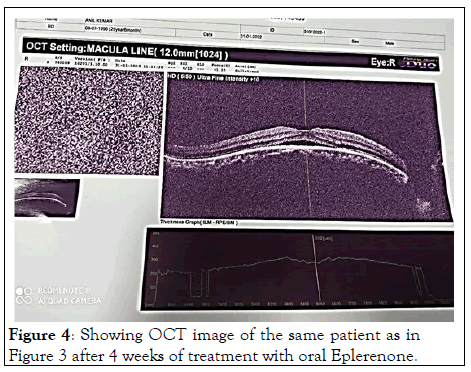
Figure 4: Showing OCT image of the same patient as in Figure 3 after 4 weeks of treatment with oral Eplerenone.
CSCR typically affects individuals in 20-45 age groups with male preponderance that constitutes major part of work force population. Since the vast majority of cases of CSCR resolve over 3-6 months hence, most often the initial treatment of choice is observation, but it leads to loss of work hours and wages. Early visual rehabilitation is the need of hour. Various treatment modalities available include medical management, laser photocoagulation and photodynamic therapy.
Group A (observation), group B (oral acetazolamide) and group C (Oral Eplerenone) did not show significant visual improvement at 2 weeks but significant improvement was observed in group B and C (p<0.01) at 6 weeks in comparison to group A.
Group D patients (laser photocoagulation) showed significant improvement in visual acuity (p<0.05) at 2 weeks, which further improved at 6 weeks.
At 12 weeks all groups had comparable improvement.
3 patients in group A, 1 each in group B and D and 2 patients in group C showed recurrence (Table 3).
Paresthesia, numbness and gastric upset related to drug acetazolamide was noted in 5 patients (26.3%) of group B (Table 3).
66.6% cases of group A, 52.6% group B, 21% in group C and 5% cases in group D showed leakage at 2 weeks, while 16.7% in group A, 10.5% group B, 5.3% in group C and 5% in group D showed leakage on FFA after 12 weeks
Our result was in concordance with similar previous studies. Resolution was greater in Group D than Group C. The time taken for disappearance of leakage on FFA was consistent with time taken for improvement in VA.
Hence CSCR patients can be treated with observation alone for the leak to resolve spontaneously or can be offered treatment with oral acetazolamide or oral eplerenone and laser. But, waiting for a period of 3-4 months for visual recovery can lead to loss of daily wages; hence early resolution is demanded by patients.
Laser photocoagulation requires precision, expertise and expensive infrastructure whereas acetazolamide and eplerenone is cost effective and can be initiated by general ophthalmologists clearly demonstrates the effect of eplerenone within one month on OCT. Laser may lead to scotoma formation and laser is not recommended if leakage is within foveal avascular zone, foveal burn can occur.
More complications were seen with oral acetazolamide and recovery was also slower than eplerenone. Based on the current literature, eplerenone seems to be efficient, especially at the acute stage of the disease. Since the results on patients with widespread RPE changes are limited and non-significant, further research is needed to determine which patients are most likely to benefit from eplerenone and their imaging characteristics, while potential combination with other treatment modalities can be also considered.
Citation: Pandey J (2022) A Study on Visual Outcome in Central Serous Chorioretinopathy (CSCR) with Different Treatment Modalities. J Clin Exp Ophthalmol. 13:926.
Received: 03-May-2022, Manuscript No. JCEO-22-17324; Editor assigned: 05-May-2022, Pre QC No. JCEO-22-17324(PQ); Reviewed: 19-May-2022, QC No. JCEO-22-17324; Revised: 04-Jul-2022, Manuscript No. JCEO-22-17324(R); Published: 11-Jul-2022 , DOI: DOI: 10.35248/2155-9570.22.13.926
Copyright: © 2022 Pandey J. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.