Orthopedic & Muscular System: Current Research
Open Access
ISSN: 2161-0533
ISSN: 2161-0533
Case Study - (2024)Volume 13, Issue 2
Background: Total Hip Replacement (THR) is a common procedure that is performed increasingly often. Although most patients have satisfactory long-term stability, approximately 17% of prosthetic hips fail, thus requiring revision. Frequently, when hip prosthesis revision is undertaken, there is significant acetabular bone deficiency present; this clinical setting presents one of the most challenging circumstances in hip surgery. There is a variety of surgical hardware and strategies available to address this problem.
Preoperative planning is a critical aspect of any reconstructive hip surgery but is particularly important in revision surgery. The surgeon must anticipate instrument, bone graft and implant requirements for the surgery, as well as which reconstructive options may be needed, based on what may be found intraoperatively. The purpose of this study was to evaluate early functional results of hip arthroplasty with acetabular defects, pelvic bone loss revised with porous tantalum acetabular components.
Methods: 56 patients were operated during research period with different kind of acetabular defects. W.G. Paprosky classification was used to classify existing acetabular defect. From 56 patients 26 was primary hip replacement and 30-revision.
Results: Different kind of tantalum constructions were used to reconstruct acetabular defects during replacement surgery. During research period three patient had complications: Two cases of dislocation after revision replacement (3.6%) and one–after primary replacement (1.8%), one suppuration case (1.8%).
Conclusion: According research results possible to make conclusion: using tantalum augments during acetabular region reconstruction allow to avoid non-biological fixators support rings and structural grafts; tantalum augments are successfully applicable during all kinds of acetabular defects reconstruction, in primary and revision replacement; using tantalum augments during acetabular region reconstruction allow to achieve components stable primary fixation.
Acetabular defect; Hip replacement; Paprosky classification; AAOS classification; Tantalum construction
THR: Total Hip Replacement; AAOS: American Academy of Orthopaedic Surgeons
Total Hip Replacement (THR) is a common procedure that is performed increasingly often. Although most patients have satisfactory long-term stability, approximately 17% of prosthetic hips fail, thus requiring revision. Frequently, when hip prosthesis revision is undertaken, there is significant acetabular bone deficiency present; this clinical setting presents one of the most challenging circumstances in hip surgery [1]. There is a variety of surgical hardware and strategies available to address this problem.
Indications for acetabular revision include symptomatic aseptic loosening, failure of fixation, infection, wear, osteolysis and instability. Bozic and associates, using the Healthcare Cost and Utilization Project Nationwide Inpatient Sample database, recently found that the most common cause of revision hip surgery was instability or dislocation (22.5%).
Acetabular defects classification systems
AAOS classification: The American Academy of Orthopaedic Surgeons (AAOS) classification of bone defects, as described by D’Antonio and associates, identifies the pattern and location of bone loss but does not quantify the defect. This system, which was developed by evaluating AP and lateral hip radiographs and comparing results intraoperatively, is probably the most commonly used classification in the literature.
Paprosky classification: The Paprosky classification system is based on the severity of bone loss and on the ability to obtain cementless fixation for a given bone loss pattern. It was initially developed by evaluating the AP pelvis radiograph and comparing this information with intraoperative findings. Careful interpretation of the AP radiograph can predict the type of defect and can allow the surgeon to plan for the acetabular reconstruction. Four criteria are used to assess the preoperative radiograph: (1) superior migration of the hip center, (2) ischial osteolysis, (3) teardrop osteolysis and (4) position of the implant relative to Kohler’s line.
Preoperative planning: Preoperative planning is a critical aspect of any reconstructive hip surgery but is particularly important in revision surgery [2]. The surgeon must anticipate instrument, bone graft and implant requirements for the surgery, as well as which reconstructive options may be needed, based on what may be found intraoperatively.
Every patient undergoing revision surgery should be screened for infection with at least an erythrocyte sedimentation rate and Creactive protein. The erythrocyte sedimentation rate should be less than 30 mm/hr and the C-reactive protein less than 10 mg/L.
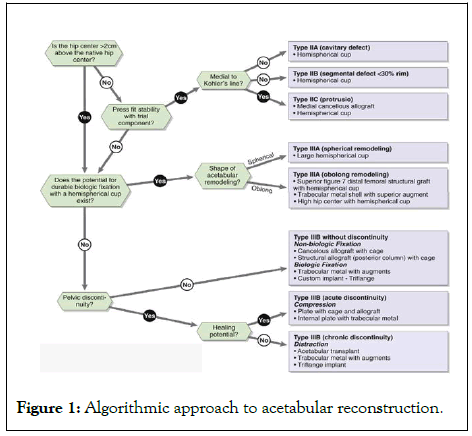
Figure 1: Algorithmic approach to acetabular reconstruction.
Treatment options for acetabular defects
Several options are available for acetabular revision. These options are divided into two major categories based on the type of fixation. Biological fixation refers to any surgical option that requires direct contact with host bone and osteointegration into the acetabular shell to provide long-term fixation [3]. Biological fixation techniques include the use of a hemispherical uncemented cup at the anatomic hip center or a high hip center (>2 cm superior to the native hip center), a jumbo cup (66 mm to 80 mm), a bilobed or oblong cup, an uncemented hemispherical cup supported by structural allograft, and a modular cementless implant system. Nonbiological fixation refers to any method of reconstruction that achieves stability of the acetabular component through a mechanical construct without the need for osteointegration between the acetabular shell and the host bone [4]. Nonbiological fixation techniques include cementing of a polyethylene cup, use of a superior structural allograft and a cemented polyethylene cup with or without an antiprotrusio cage, impaction grafting with or without an antiprotrusio cage and application of a total acetabular allograft.
Own experience for acetabular defects reconstruction
This chapter presented our own experience for acetabular defects reconstruction. 56 patients were operated during the research period: 26-primary hip replacement and 30 patients with revision hip (Figure 2). Only W.G. Paprosky classification was used to classify acetabular defects during our investigation (Table 1).
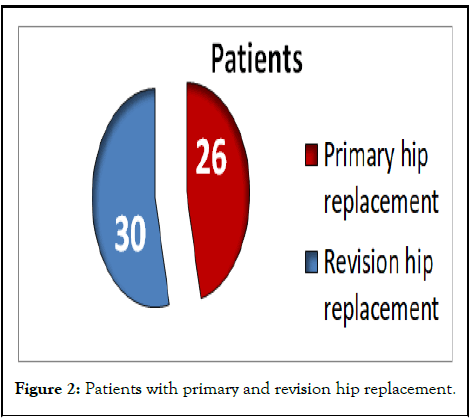
Figure 2: Patients with primary and revision hip replacement.
| Type of operation | Defect type according to W.G. Paprosky classification | Amount of patients |
|---|---|---|
| Primary hip replacement | II B | 12 |
| II C | 2 | |
| III A | 9 | |
| III B | 3 | |
| Revision hip replacement | II C | 3 |
| III A | 17 | |
| III B | 10 | |
| All operations | 56 |
Table 1: Patients’ distribution according to the type of acetabular defect.
Different kind of tantalum constructions were used to reconstruct existing acetabular defects during replacement surgery.
Porous tantalum is an alternative metal for total joint arthroplasty components that offers several unique properties. Its high volumetric porosity (70% to 80%), low modulus of elasticity (3 MPa) and high frictional characteristics make it conducive to biologic fixation. Tantalum has excellent biocompatibility and is safe to use in vivo.
The low modulus of elasticity allows for more physiologic load transfer and relative preservation of bone stock. Because of its bioactive nature and ingrowth properties, tantalum is used in primary as well as revision total hip arthroplasty components, with good to excellent early clinical results [5]. In revision arthroplasty, standard and custom augments may serve as a structural bone graft substitute. Now some patients’ X-rays will be presented before and after operation and we will try to make a conclusion according to this experience.
In the Figure 3 was presented the patient with II B acetabular defect (cavitary acetabular defect) according W.G. Paprosky-primary hip replacement. In the preoperative X-Ry and 3D picture possible to see bone deficiency in superiorlateral part of acetabulum [6]. In the postoperative X-Ry and 3D picture Figure 4 existing defect was covered with tantalum augment. Between augment and cup bone cement was used.
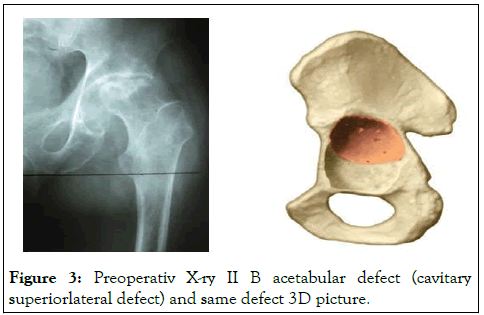
Figure 3: Preoperativ X-ry II B acetabular defect (cavitary superiorlateral defect) and same defect 3D picture.
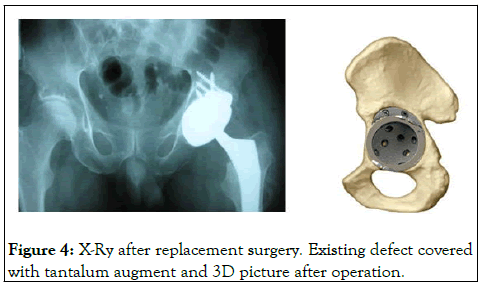
Figure 4: X-Ry after replacement surgery. Existing defect covered with tantalum augment and 3D picture after operation.
In the Figures 5 and 6 again possible to see II B defect (segmental acetabular defect) according Paprosky classification, before and after operation. This case presented revision hip replacement. In preoperative X-Ry we can see acetabular cup failure after cemented fixation.
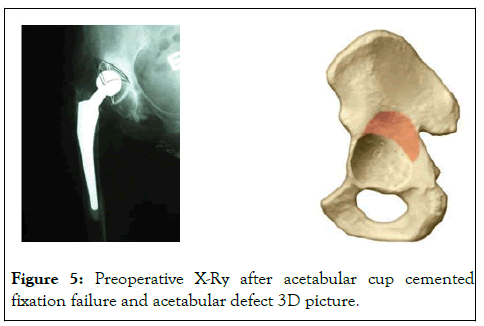
Figure 5: Preoperative X-Ry after acetabular cup cemented fixation failure and acetabular defect 3D picture.
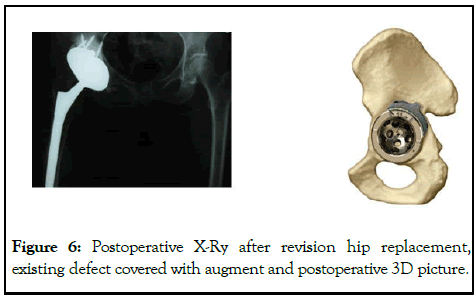
Figure 6: Postoperative X-Ry after revision hip replacement, existing defect covered with augment and postoperative 3D picture.
Next patient, Z.D.Y, 47 years old, was operated with III A defect (extensive segmental acetabular defect)-primary hip replacement [7]. In the Figures 7 and 8 possible to see preoperative and postoperative X-Rys, 3D pictures. In next case also possible to see III A acetabular defect (Figure 9). Patient had bone deficiency in the central part of acetabulum. During next three cases we want to present patients with III A and B acetabular defects with severe bone loosening.
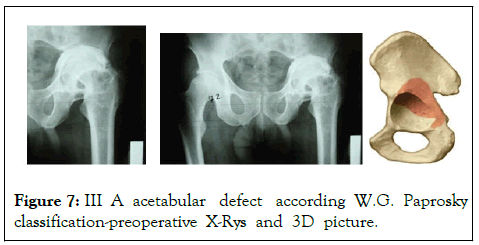
Figure 7: III A acetabular defect according W.G. Paprosky classification-preoperative X-Rys and 3D picture.
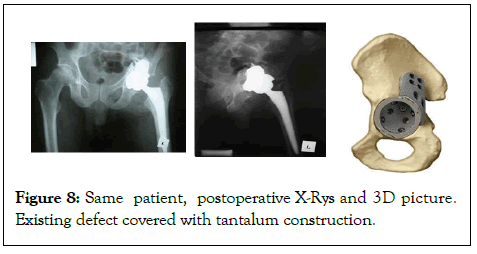
Figure 8: Same patient, postoperative X-Rys and 3D picture. Existing defect covered with tantalum construction.
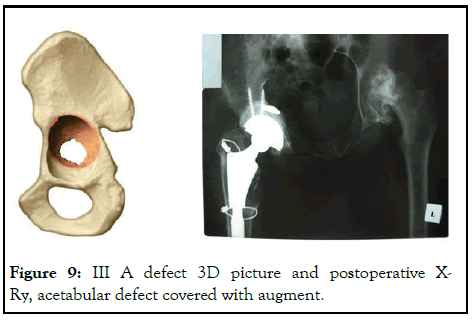
Figure 9: III A defect 3D picture and postoperative XRy, acetabular defect covered with augment.
The first patient had dislocation after replacement surgery and instability for all component of endoprosthesis. In Figure 10 we can see X-Ry before operation and after the first operation. Aim of the first operation as removing previous prosthesis and putting spacer [8]. There was huge bone defect in acetabular region, III B (Figures 10 and 11). In Figure 12 possible to see acetabular defect reconstruction with tantalum augment, during the surgery A (intraoperative pictures) and after surgery B (postoperative X-Ry).
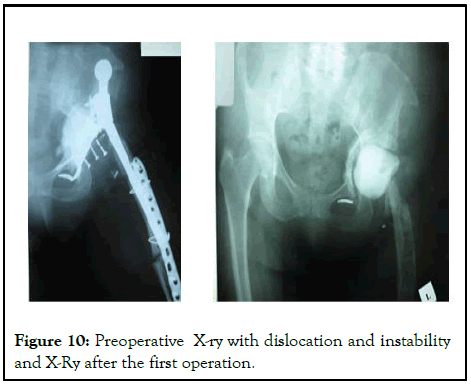
Figure 10: Preoperative X-ry with dislocation and instability and X-Ry after the first operation.
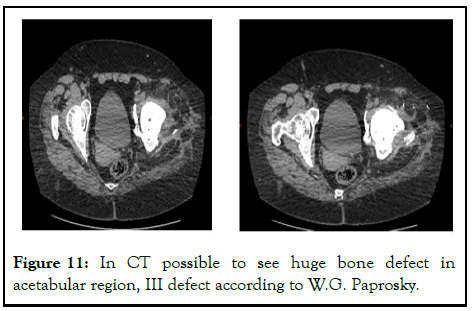
Figure 11: In CT possible to see huge bone defect in acetabular region, III defect according to W.G. Paprosky.
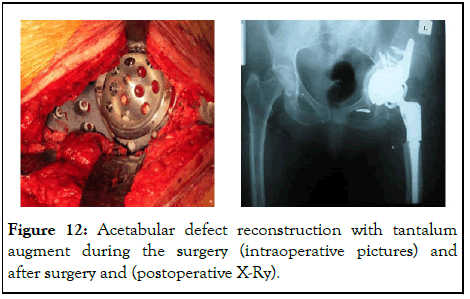
Figure 12: Acetabular defect reconstruction with tantalum augment during the surgery (intraoperative pictures) and after surgery and (postoperative X-Ry).
The second case-32 years old patient, Y.W.Z, after acetabular region plating operation. Patient had deformity in the hip joint and severe pain [9]. In Figure 13 possible to see preoperative XRys, III A defect according to W.G. Paprosky classification and in Figure 14-postoperative X-Rys, after the reconstraction surgery with tantalum construction.
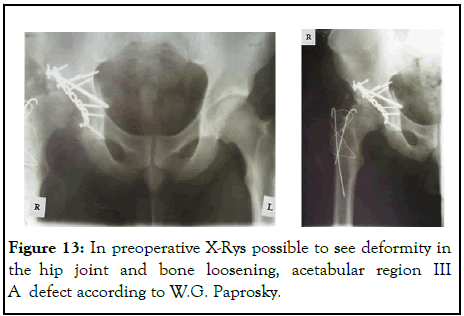
Figure 13: In preoperative X-Rys possible to see deformity in the hip joint and bone loosening, acetabular region III A defect according to W.G. Paprosky.
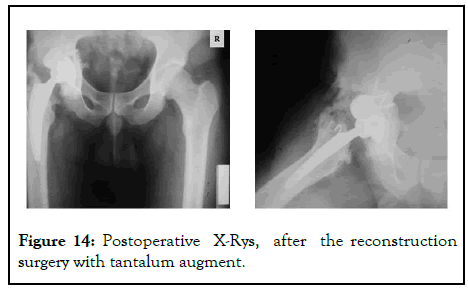
Figure 14: Postoperative X-Rys, after the reconstruction surgery with tantalum augment.
The third patient 73 years old female, H.Y.Z., after bilateral hip replacement (Figure 15). In the right side possible to see huge bone defect (III B) in the acetaular region, cup loosening and fracture, in the left side also bone defect and cup loosening. Figure 16 presented tantalum augments preparation with using bone cement [10-12]. In the Figure 17 we can see postoperative X-Rys, after the right acetabulum reconstruction with augments and in the Figure 18 possible to compare difference between using cup cage technic and tantalum augment.
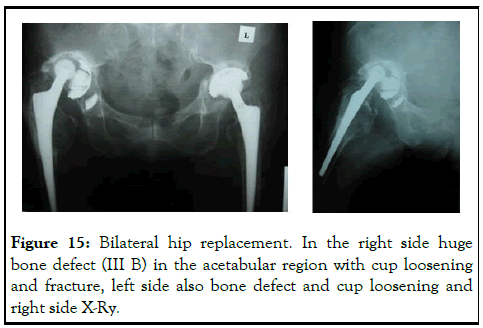
Figure 15: Bilateral hip replacement. In the right side huge bone defect (III B) in the acetabular region with cup loosening and fracture, left side also bone defect and cup loosening and right side X-Ry.
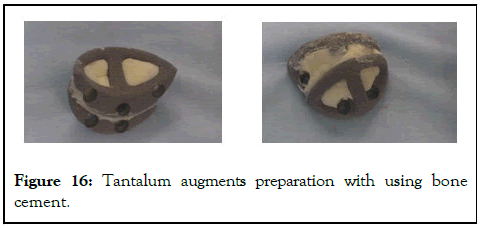
Figure 16: Tantalum augments preparation with using bone cement.
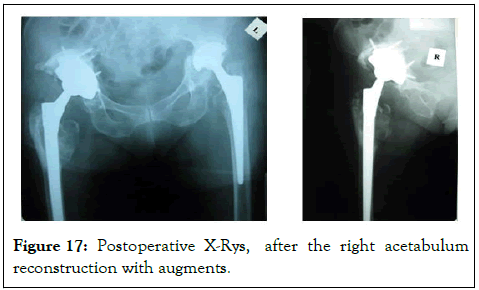
Figure 17: Postoperative X-Rys, after the right acetabulum reconstruction with augments.
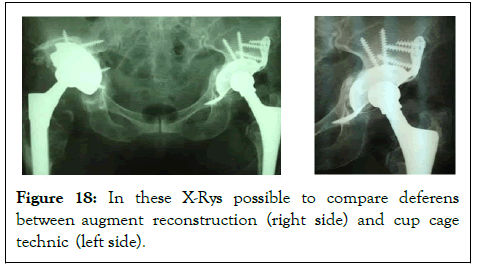
Figure 18: In these X-Rys possible to compare deferens between augment reconstruction (right side) and cup cage technic (left side).
During research period we had three patients with complications (Figure 19): Two cases of dislocation after revision replacement (3.6%) and one-after primary replacement (1.8%) (Figure 20), one suppuration case (1.8%) (Figure 19) [13-15].
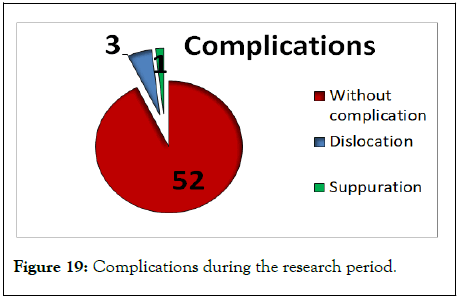
Figure 19: Complications during the research period.
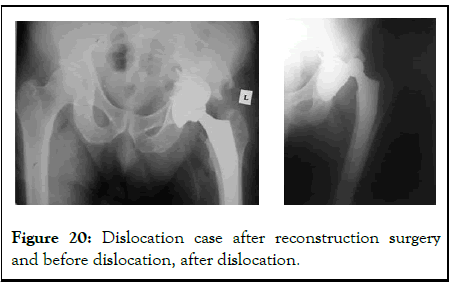
Figure 20: Dislocation case after reconstruction surgery and before dislocation, after dislocation.
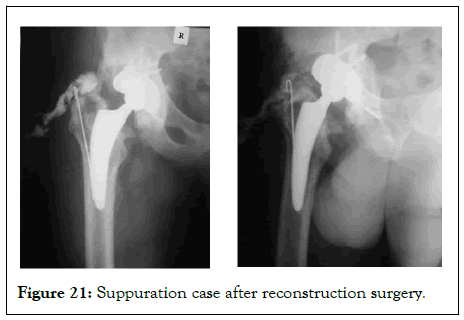
Figure 21: Suppuration case after reconstruction surgery.
Using tantalum augments during acetabular region reconstruction allow to avoid non-biological fixators-support rings and structural grafts. Augments selection is conducted according to preoperative planning, in which is necessary performing CT with 3D reconstruction. Tantalum augments are successfully applicable during all kinds of acetabular defects reconstruction, in primary and revision replacement. For augments successful osseointegration is necessary close contact between tantalum and bone. Using tantalum augments during acetabular region reconstruction allow to achieve components stable primary fixation.
Not applicable.
Not applicable.
The data that support the findings of this study are available from the second military medical university, PRC, Shanghai; Yerevan state medical university, Yerevan, Armenia; Artmed MRC, Yerevan, Armenia but restrictions apply to the availability of these data, which were used under license for the current study and so are not publicly available. Data are however available from the authors upon reasonable request and with permission of mentioned institutions. This study includes materials from master degree research has been done in the second military medical university, PRC, Shanghai from 2013 to 2015 and materials from Yerevan State Medical University, Yerevan, Armenia; Artmed MRC, Yerevan, Armenia.
The authors declare that they have no competing interests.
There aren't special sources of funding for the research. The research has been done in the second military medical university, Yerevan state medical university and Artmed MRC.
Artak S. Galstyan analyzed and interpreted the patient data, evaluated functional results of hip arthroplasty with acetabular defects, pelvic bone loss revised with porous tantalum acetabular components, performed or took part in primary or revision hip replacement surgeries. Yulin Wu and Peiliang Fu performed primary or revision hip replacement surgeries and were a major contributors in writing the manuscript. All authors read and approved the final manuscript.
Not applicable.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Galstyan AS, Wu Y, Fu P (2024) Acetabular Defects Reconstruction with Tantalum Constructions. Orthop Muscular Syst. 13:394.
Received: 08-Jul-2020, Manuscript No. OMCR-24-5342; Editor assigned: 13-Jul-2020, Pre QC No. OMCR-24-5342 (PQ); Reviewed: 27-Jul-2020, QC No. OMCR-24-5342; Revised: 15-May-2024, Manuscript No. OMCR-24-5342 (R); Published: 12-Jun-2024 , DOI: 10.35248/2161-0533.24.13.394
Copyright: © 2024 Galstyan AS, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Sources of funding : There aren't special sources of funding for the research. The research has been done in the second military medical university, Yerevan state medical university and Artmed MRC.