Journal of Clinical & Experimental Dermatology Research
Open Access
ISSN: 2155-9554
ISSN: 2155-9554
Short Communication - (2019)Volume 10, Issue 2
Acquired acral fibrokeratoma is a benign fibrous tumor of hypothetical pathophysiology. It is rarely localized on the nail and exceptionally simulates supernumerary digit. We report three rare and original cases of acquired ungual fibrokeratoma, in which dermoscopy showed two parts of distinct dermoscopic features suggesting supernumerary digit. The explanation of such a differentiation remains to be determined, opening the discussion on a possible new pathophysiological hypothesis.
Acquired ungual fibrokeratoma; Supernumerary digit; Dermoscopic analysis
AUFK: Acquired Ungual Fibrokeratoma; AAFK: Acquired Acral Fibrokeratoma
Acquired ungual fibrokeratoma (AUFK) is a benign and rare fibrous tumor, of uncertain aetiology. We report three rare and original cases of AUFK simulating supernumerary digits with description of clinical aspect and dermoscopic characteristics.
We report cases of two men and one woman, whose mean age was 32 years old, with no significant past medical history apart from a trauma in one of them. They consulted for lesions on the thumb; the big toe; and the small toe respectively, in the periungual area for two patients and intraungual for the third one. The lesions were asymptomatic but gradually increasing in size.
Clinical examination showed filiformis and infracentimetric lesions of firm consistency, with a hard and keratosis end. Dermoscopic examination showed two parts, the first proximal one, which was pinkish with some punctiform and linear vessels; and the distal one, which was keratotic with a yellow brown keratin appearance. The hole simulating a supernumerary digit (Figure1). The rest of somatic examination was normal without any associated signs compatible with tuberous sclerosis like adenoma sebaceum, shagreen patches, or ash leaf macules.
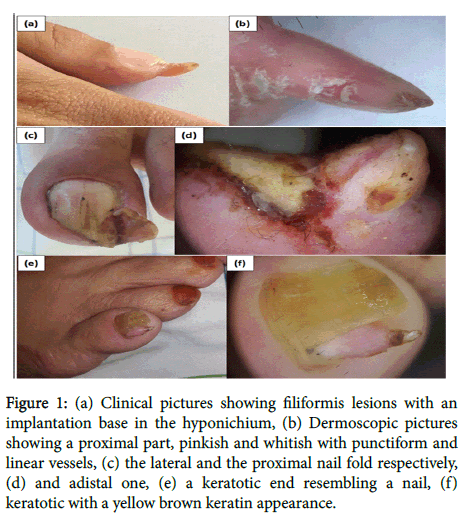
Figure 1: (a) Clinical pictures showing filiformis lesions with an implantation base in the hyponichium, (b) Dermoscopic pictures showing a proximal part, pinkish and whitish with punctiform and linear vessels, (c) the lateral and the proximal nail fold respectively, (d) and adistal one, (e) a keratotic end resembling a nail, (f) keratotic with a yellow brown keratin appearance.
Total excision of the lesions under local anesthesia was performed in the three patients. Histological study revealed epidermal hyperkeratosis and acanthosis with dermal fibroblasts and collagen bundles parallel to the longitudinal axis of the lesions, evoking AUFK (Figure 2).
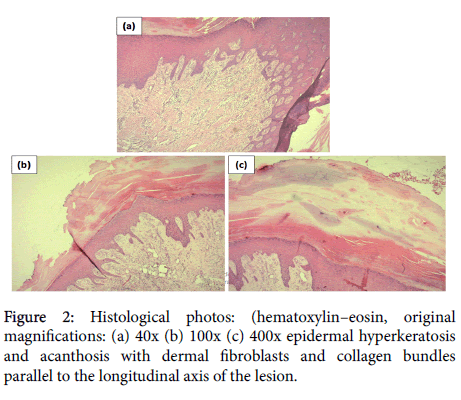
Figure 2: Histological photos: (hematoxylin–eosin, original magnifications: (a) 40x (b) 100x (c) 400x epidermal hyperkeratosis and acanthosis with dermal fibroblasts and collagen bundles parallel to the longitudinal axis of the lesion.
Good aesthetic and functional evolution was noticed in our patients, without recurrence after 18 months follow-up.
Acquired acral fibrokeratoma (AAFK) was first isolated in 1968 by Bart et al. [1]. In its typical form, AUFK affects the middle-aged adult with a slight male predominance [2]. It clinically appears as an asymptomatic and solitary outgrowth, measuring 3 to 5 mm, it can be pediculate and the surface might appear keratotic [3,4].
In most reported cases, AAFK is located in fingers and toes. Nail location remains rare [3-7]. According to Hwang S et al. AUFK is more often localized on toenails rather than on fingernails, mostly in periungual, rarely in intraungual and exceptionally in subungual area [7]. The main clinical differential diagnoses of AUFK are: Koenen tumors (or periungual fibroma) in tuberous sclerosis, onychomatricoma, wart, cutaneous horn and supernumerary digit. In our cases, the two main differential diagnoses were: Koenen tumors (or periungual fibroma) and supernumerary digit. Our results are then consistent with those reported in the literature, but to our knowledge, only two cases of AUFK simulating a supernumerary digit have been described [2,8].
To date, only two articles have described dermoscopic features of AAFK [9,10]. The first one was characterized by a homogeneous light yellowish core fringed by keratotic white scaly collars, furthermore, red spherical vessels externally encircled the whole tumor mass [9]. In the second one, dermoscopic findings revealed the presence of clumps of homogenous red lacunae divided by a white meshwork-like septal wall with telangiectasia on the adjacent skin [10]. Due to the diverse degree of vascular formations and collagen fiber accumulation, dermoscopic features may differ among AAFK cases [9]. In our patients, dermoscopy showed two parts of distinct dermoscopic features suggesting supernumerary digit.
Kint et al. described 3 types of AAFK by their clinical and histopathologic features [11]. Type I is a dome-shaped lesion that contains fibroblasts between collagen bundles, fine elastic fibres and numerous capillaries in the dermis. Type II is typically tall and is a hyperkeratotic lesion that contains many more fibroblasts and less elastic fibres than type I. Type III is a flat to dome-shaped lesion characterized by poorly cellular and edematous structures and no elastic fibres. The tumors in our cases had the typical histopathologic findings of type II AAFK. Histological study allowed the distinction with the two main differential diagnoses already mentioned. Supernumerary digit which is a congenital digital anomaly containing neural bundles in the dermis; and Koenen tumors, which typically present with multiple periungual fibromas in approximately 50% of tuberous sclerosis cases, and usually occur during puberty. The presence of conspicuous, atypical, and stellate myofibroblasts within the fibrous core of Koenen tumors is distinct from the histopathologic features of AAFK.
AUFK does not regress spontaneously and treatment of choice is surgical resection. The tumor must be excised carefully so as not to damage the matrix, which can lead to permanent nail dystrophy [3-6]. Recurrence of the tumor is possible in 3% of cases according to Hwang et al. [7].
The aetiology of AAFK is unknown and its pathophysiology remains hypothetical [2]. Traumatic origin was invoked but remains invalid. The role of factor XIIIa was also reported and a possible infectious origin suggested. In our patients, we indentified three specific AUFK with two parts of distinct clinical and dermoscopic characteristics. The explanation of such a differentiation remains to be determined, opening the discussion on a possible new pathophysiological hypothesis which should be confirmed on larger samples.
Citation: Salim S, El Meknassi I, Znati K, Meziane M (2019) Acquired Ungual Fibrokeratoma Simulating Supernumerary Digit: Dermoscopic Analysis of Three Cases. J Clin Exp Dermatol Res 10: 493. doi:10.4172/2155-9554.1000493
Received: 27-Jan-2019 Accepted: 04-Mar-2019 Published: 11-Mar-2019
Copyright: © 2019 Salim S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.