Clinical Pediatrics: Open Access
Open Access
ISSN: 2572-0775
ISSN: 2572-0775
Case Report - (2022)Volume 7, Issue 5
Background: Acute Compartment Syndrome (ACS) is a limb threatening condition that may be identified by key physical exam findings often accompanied by history of trauma. Pediatric exercise induced compartment syndrome is an uncommon presentation.
Case presentation: A 17-year-old female with a medical history of morbid obesity presented to the emergency department with severe right lower leg pain, swelling, and loss of sensation of the lateral leg and dorsum of the foot. 3 days prior to symptom onset, the patient participated in a parade as part of a marching band. No history of injury and no other relevant medical history.
Discussion: Acute compartment syndrome, while generally associated with trauma, can have variable etiologies ranging from electrical injury to overexertion. Exercised induced compartment syndrome may present insidiously with myoedema, inflammatory cascade, and elevation of compartment pressures leading to potentially devastating consequences.
Trauma; Swelling; Acute compartment syndrome; Emergency department
ACS occurs when inhibited venous outflow from the myofascial compartment impedes arterial circulatory patency. The reduction of arterial flow from increased pressure causes a failure to reach the metabolic demands of the tissue and causes swelling, inflammation, and resultant tissue ischemia. Trauma can contribute to this by impairing arteriovenous gradient dilating the arterial system and causing small vessel collapse [1]. Elevated interstitial pressures also occur due to increased vessel permeability causing extravasation. Subsequent loss of tissue oxygenation and hypoglycemia depleting ATPase activity causes myocytic swelling and cytotoxic edema [2]. Necrosis can occur due to prolonged tissue hypoxia and muscle damage (which causes elevated intracellular calcium that activates proteases) [3]. Increased pressure also acutely retards neuromuscular function; prolonged nerve compression within the myofascial compartment can lead to permanent sensory/motor impairment. Surgical myofascial compartment release (fasciotomy) reduces interstitial pressures and normalizes arteriovenous gradient in an attempt to restore prefusion. Fasciotomy wounds are routinely managed with negative pressure wound therapy during serial tissue viability exams under anesthesia. Numerous closure methods are employed including purse string sutures. In some cases, skin grafting may be required.
A 17-year-old female presented to the ED with progressively worsening right sided leg pain rated 10/10 and associated leg swelling. Three days prior, the patient experienced onset of right lower leg pain after marching over 2 miles over the course of several hours as part of a Mardi Gras marching band. The patient had failed conservative measures and expectant management which prompted presentation.
When she presented to the ED, vitals were notable for tachycardia at 137 bpm, BP 130/64, RR 18, and afebrile at 99.9 F (37.7 C) SPO2 100%, BMI 40.24 kg/m2. Patient reported numbness along lateral right lower leg and dorsolateral right foot (paresthesia in the right peroneal and common peroneal nerve distribution). Pain and swelling was maximal just anterior inferior to the right knee. Pain was exacerbated by palpation, range of motion, and ambulation. Serology with WBC >20,000 and CPK >1600 raised suspicion for rhabdomyolysis. Urinalysis was unremarkable, patient denied urinary symptoms.
On exam, anterior and lateral compartments were firm and noncompressible compared to the contralateral leg. Posterior compartments remained supple. Tibialis anterior motor function was absent. Sensation was absent at the dorsum of the first web space and over the lateral aspect of the foot. DP and PT pulses intact, strong, and regular. Capillary refill was <3 seconds.
Serology showed elevated WBC at 20.68 K/uL (4.5-11 K/uL), predominantly granulocytes at 79.3% (40-59%), low RBC at 3.89 M/uL (4.10-5.10 M/uL), borderline low hemoglobin at 11.7 g/dL (11.6-15 g/dL), borderline low hematocrit at 35.5% (35.5-44.9%), and normal serum lactate levels at 1.5 u/L. Elevated AST at 292 U/L (10-40) and ALT at 117 U/L (10-44 U/L). Creatinine and electrolytes were within normal limits.
Plain radiographs of the right tibia and fibula were without acute osseus abnormality, CT of the leg was consistent with subcutaneous and soft tissue swelling most pronounced in the lateral compartment, more prominent distally involving the lateral ankle and hindfoot. Normal muscle bulk. There were no fluid collections, ring enhancing abscesses, or soft tissue air suggesting necrotizing fasciitis (Figures 1 and 2).
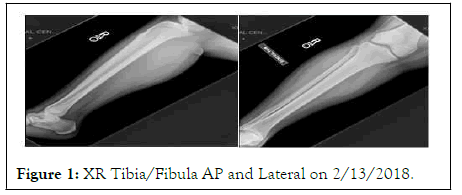
Figure 1: XR Tibia/Fibula AP and Lateral on 2/13/2018.
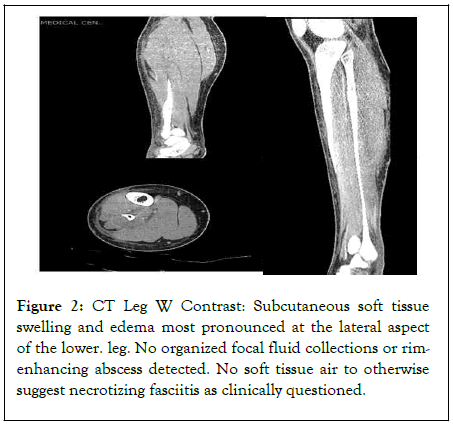
Figure 2: CT Leg W Contrast: Subcutaneous soft tissue swelling and edema most pronounced at the lateral aspect of the lower. leg. No organized focal fluid collections or rimenhancing abscess detected. No soft tissue air to otherwise suggest necrotizing fasciitis as clinically questioned.
Intra-compartmental pressure monitoring showed lateral compartment at 58 mmHg, anterior compartment at 38 mmHg, diastolic pressures prior to anesthesia were 67. Delta pressure was 9 mmHg in lateral compartment, 29 mmHg in anterior compartment, no signs of posterior compartment syndrome.
Treatment
Patient was emergently taken to the operating room for fasciotomies of the lateral and anterior compartments. The leg was prepped in a sterile fashion and a longitudinal (⁓20 cm) incision was made 1 cm anterior to the fibula. Sharp dissection was carried down to the fascial layer. The intermuscular septum was found and palpated. A transverse incision was made across both lateral and anterior compartments with immediate muscle and fat extrusion from the anterior compartment.
Using Metzenbaum scissors, the fasciotomies were extended distally and proximally in the lateral then anterior compartments. Care was taken to avoid the SPN. When compartments were completely released, electrocautery was used to stimulate the muscles. The anterior compartment muscles were pink, viable, and contracted with cautery. The lateral compartment muscles were dusky and did not respond to cautery. The wound was then irrigated with copious amounts of saline. A white sponge was applied in the wound bed. Two vessel loops were used to hold the incision tension. Good seal was obtained by covering incision with black sponge and applying sterile wound vac dressings (Figure 3).
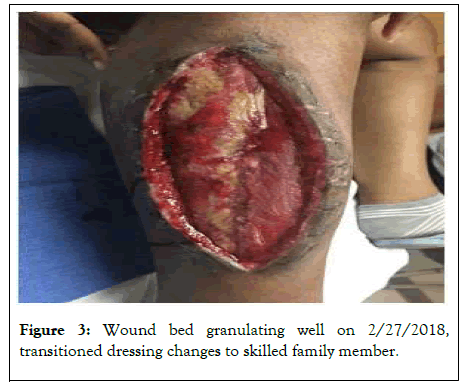
Figure 3: Wound bed granulating well on 2/27/2018, transitioned dressing changes to skilled family member.
Serial debridement under anesthesia were performed over the next 6 days (2/15, 2/17, 2/19). Anterior compartment at that time demonstrated slight duskiness but remained consistently responsive to electrical stimulation, retaining a “beefy” appearance consistent with healthy muscle tissue. Lateral compartment remained dusky and unresponsive to electrical stimulation without development of purulence or liquefaction. POD1 US Duplex Ultrasonography BLE was without evidence of DVT bilaterally. After the 4th debridement, the patient was discharged home with wound care and close orthopedic/plastic surgery FU for skin graft assessment.
Outcome/Follow up
At 1 week FU, a foot drop was noted on the RLE. Mild motor function was present in the DPN distribution. At 4-week FU where patient was deemed ready for skin grafting, the patient demonstrated persistent sensation loss along dorsum right foot and had begun experiencing new ankle pain. Ankle XR obtained showed no abnormality; patient was prescribed PT and an ankle foot orthosis.
At 5 weeks FU, the patient underwent skin grafting of the 20 × 8 cm RLE fasciotomy site. The graft site was debrided of all nonviable tissue and displayed a healthy bleeding bed. Split thickness skin graft harvested from the thigh meshed in a 1-1/2:1 fashion. There were no complications, and 100% graft take was achieved at FU 1 month later.
At 2 months FU, the patient was unable to dorsiflex the ankle and remained insensate to the dorsum of the first webspace. Gait was significant for foot drop to right ankle. Weak dorsiflexion was regained a month later and progressively improved by the 4 months FU which showed 4/5 strength dorsiflexion and eversion.
At 1-year FU, patient was able to heel walk but reported sharp anterior ankle pain with prolonged standing. PT for gait training was prescribed. At 14 mo FU, there were no complaints other than persistent numbness to the dorsal right foot.
ACS is a well-recognized potentially life-threatening medical emergency that can occur anywhere in the body that has limited capacity for tissue expansion [4]. Once tissue perfusion is compromised after reaching a critical pressure within the myofascial compartment, permanent damage may occur in as little as 6 hours [4-6].
Etiologies include trauma, compression, muscle infarction due to underlying health conditions, and exercise [4,5]. Most cases are due to trauma such as crush injuries and burns, with ⁓75% cases associated with fractures [7]. Patients who develop ACS in the absence of trauma are at higher risk for developing complications and delayed treatment [7]. Few cases of exercise induced ACS are available in the literature; all of which involve sporting events, athletes, or military recruits [5,8,9]. Our patient represents the first case of pediatric exercise induced ACS caused by prolonged ambulation in an obese but otherwise healthy person.
Tissue perfusion (delta pressure), which is compromised in all cases of ACS, is calculated by taking the difference of diastolic pressure and intra-compartmental pressure with a value of <30 mmHg being considered diagnostic. However obtaining delta pressure is unnecessary when ACS is clinically evident (pain out of proportion on exam, pain with passive flexion of toes, paresthesia…) [10]. Elevated CPK is another indicator of ACS [10]. Although physiological muscle breakdown occurs after intense exercise in healthy adults, extensive muscle damage causes release of CK and LDH. This can lead to rhabdomyolysis producing myoedema those results in ACS, even in the absence of renal impairment [3]. In our patient, CK was significantly elevated without renal impairment. Prolonged marching in a patient unaccustomed to physical exercise may have precipitated excessive muscle damage in the anterior and lateral compartments gradually elevating interstitial pressures in the myofascial compartment over the course of 3 days until reaching a delta pressure sufficient for ACS.
Management of ACS is fasciotomy to restore tissue perfusion [4]. The affected limb should not be elevated but should be kept level with the body in order to maintain arterial perfusion pressure [4]. In fasciotomy, a skin incision alone reduces compartment pressures by 5-9 mmHg. Subcutaneous release is not recommended as intact and firm overlying skin can impair the effectiveness of fascial release on compartment pressures. The anterior and lateral compartments may be accessed via a single anterolateral incision along the length of the leg [11]. Care must be taken to avoid the SPN.
ACS is a medical emergency that occurs most often in the setting of acute trauma. Exercise induced ACS is a rare cause. Clinical suspicion should be high for children/adolescents with severe pain in an extremity following exercise, especially for sedentary or physically deconditioned children. Special consideration should be taken for such population prior to participating in activities such as prolonged marching in a marching band. Laboratory studies such as CK can be useful in early identification/intervention of ACS, which is crucial in such a medical emergency.
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
Citation: Waldron S, Taylor S, Desai B, Tran L, Solan C (2022) Acute Compartment Syndrome in a Young Female After Marching in a Mardi Gras Parade. Clin Pediatr. 7:218.
Received: 22-Aug-2022, Manuscript No. CPOA-22-17991; Editor assigned: 24-Aug-2022, Pre QC No. CPOA-22-17991 (PQ); Reviewed: 07-Sep-2022, QC No. CPOA-22-17991; Revised: 13-Sep-2022, Manuscript No. CPOA-22-17675 (R); Published: 22-Sep-2022 , DOI: 10.35248/2572-0775.22.7.218
Copyright: © 2022 Waldron S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.