Journal of Clinical and Experimental Ophthalmology
Open Access
ISSN: 2155-9570
ISSN: 2155-9570
Case Report - (2024)Volume 15, Issue 6
Objective: This retrospective review of case presentation from 2023 to 2024 reports a rare case of ARPE following confirmed COVID-19 infection in a healthy young female patient.
Case presentation: A 19-year-old female with recent COVID-19 infection presented to the eye clinic with a two-week history of bilateral temporal scotomas.
Findings: Detailed review of the patients medical history was unremarkable and comprehensive diagnostic workup returned results within normal limits. Imaging tests showed characteristic features of ARPE, including fine pigment stippling and depigmented macular halo from fundus photography, increased auto fluorescence corresponding to areas of hypopigmentation and spontaneous resolution from Fundus Autofluorescence (FAF) imaging and hyporeflective attenuations in the outer retina and Retinal Pigment Epithelium (RPE) as seen from Optical Coherence Tomography (OCT).
Conclusion: This was the first case report describing the temporal relationship between COVID-19 infection and ARPE in a healthy young adult. The findings here suggest to clinicians the possibility of considering ARPE within the differential diagnoses when seeing patients, particularly young adults, who are presenting with acute visual disturbances following a viral infection.
Acute retinal pigment epitheliitis; Krill’s disease; COVID-19; Viral infection; Autofluorescence
Krill et al., described the first cases of Acute Retinal Pigment Epitheliitis (ARPE) or Krill’s disease in three male and three female patients aged between 16 to 46 years [1]. ARPE is a rare, idiopathic and self-limiting inflammatory disease of the retina affecting mostly young adults in one eye, however, cases of bilateral involvement and recurrent episodes have been published in the literature [2-7]. Functionally, the disease presents with an acute onset of mild to moderate visual disturbances, including painless central scotomas, photopsia and mild blurring that resolve spontaneously within 6-12 weeks [1,8,9]. Whereas anatomically, fundus photography can reveal retinal lesions as clusters of small, round and dark gray spots or pigment stippling, surrounded by depigmented or hypofluorescent zones in the macula [1,3,4,6].
The complete etiology and pathophysiology of ARPE remains to be fully understood due to the limited number of case reports and clinical studies, however, viral infections or viral-associated inflammatory responses have been implicated to affect the Retinal Pigment Epithelium (RPE) prior to disease onset [2,3,7,10]. Specifically, studies including a case-series of 18 patients using OCT found that the inflammation site is localized to the interdigitation zone or in contact between photoreceptors and the RPE. Although there have been case findings of ARPE following COVID-19 or seasonal influenza vaccine administration, to the best of our knowledge, there have been no reports describing new-onset ARPE following COVID-19 infection [11,12]. Herein, we present a rare case of ARPE after confirmed COVID-19 infection in a healthy young female patient.
A 19-year-old female with a recent upper respiratory tract infection later confirmed as COVID-19 through standardized testing presented to the eye clinic with a two-week history of bilateral temporal scotomas. The patient did not have any systemic vascular risk factors and did not have any ocular diseases. Her medication history included an antidepressant Trintellix and birth control pills. The patient did not receive any medical treatment during the period between infection and scotoma onset, including COVID-19 vaccination.
Clinical examination showed her best-corrected visual acuity was 20/20 in both eyes, while the anterior and posterior segments were unremarkable with no signs of inflammation or chorioretinal lesions. As posterior uveitis is a common pathology affecting all ages and a frequent reason for visiting a retina clinic, we performed a comprehensive diagnostic workup in which all tested parameters returned results within normal limits, indicating that there were no acute systemic or inflammatory processes responsible for her symptoms [13].
Imaging tests using optos fundus photography in both eyes showed characteristic fine pigment stippling and surrounding depigmented halo in the macula (Figure 1), consistent with ARPE presentation, while the FAF in both eyes showed bilateral increased autofluorescence nasal to the fovea corresponding to areas of hypopigmentation, corresponding to the temporal scotomas (Figures 1A and 1B). FAF imaging at follow up in 6 months showed a near-complete resolution of this area, consistent with ARPE’s self-limiting disease trajectory (Figure 1C). At the initial visit, OCT cross-sectional images centered at the macula revealed hyporreflective attenuations in the outer retina, including the External Limiting Membrane (ELM), Ellipsoid Zone (EZ) and Interdigitation Zone (IZ), as well as the RPE in both eyes (Figure 2A). Notably, in the left eye, the nasal quadrant showed greater parafoveal attenuations than the temporal quadrant, whereas in the right eye, the attenuations were comparable in both quadrants (Figure 2A). Large improvements were observed at follow up in 6 months in both eyes (Figure 2B). Based on the imaging results and comprehensive clinical examination ruling out other potential causes or ocular conditions, the patient was diagnosed with ARPE following COVID-19 infection (Figure 2).
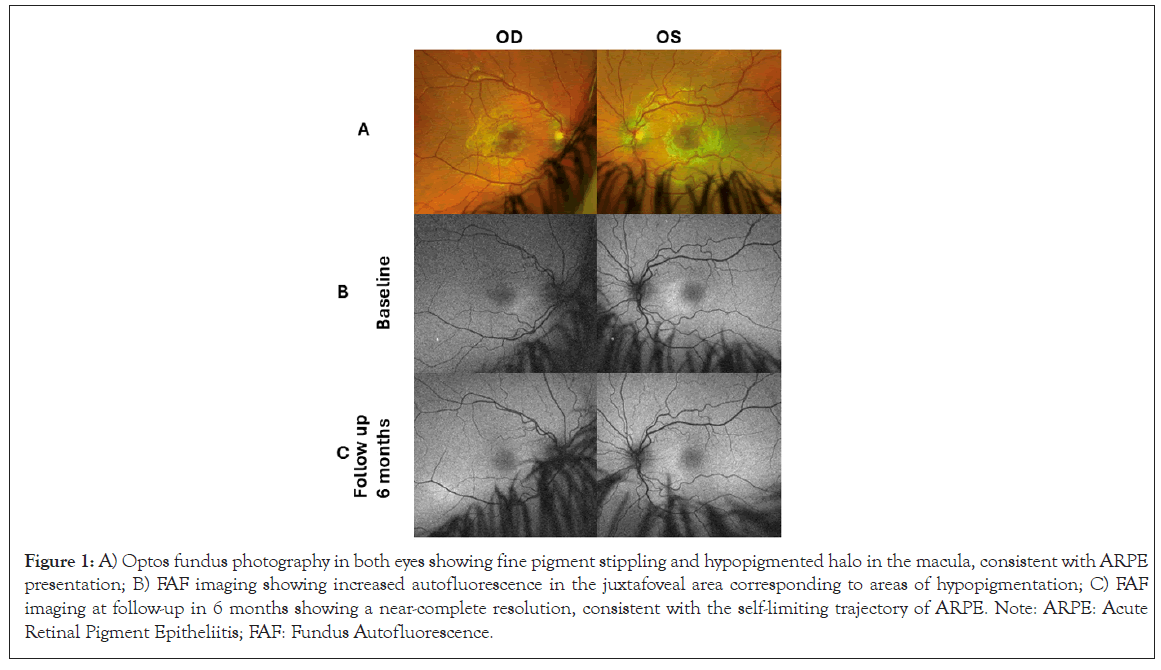
Figure 1: A) Optos fundus photography in both eyes showing fine pigment stippling and hypopigmented halo in the macula, consistent with ARPE presentation; B) FAF imaging showing increased autofluorescence in the juxtafoveal area corresponding to areas of hypopigmentation; C) FAF imaging at follow-up in 6 months showing a near-complete resolution, consistent with the self-limiting trajectory of ARPE. Note: ARPE: Acute Retinal Pigment Epitheliitis; FAF: Fundus Autofluorescence.
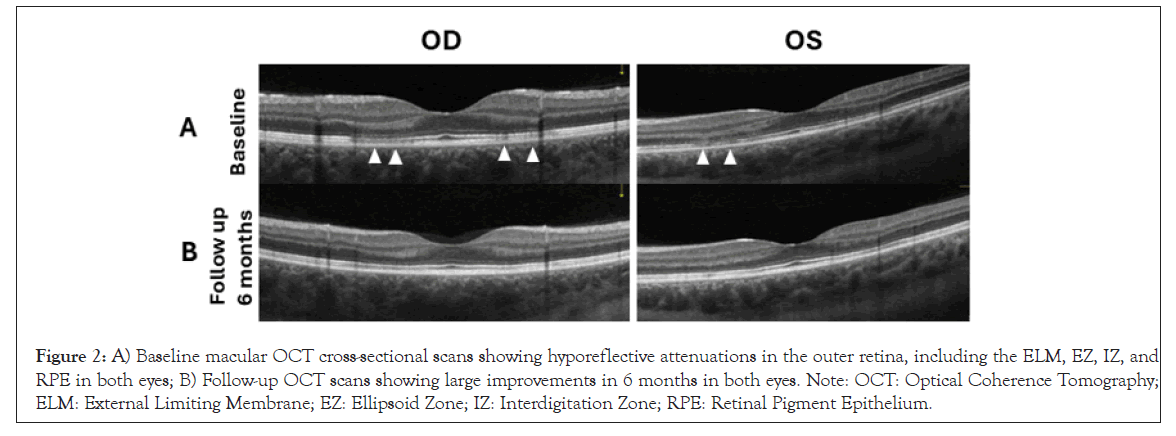
Figure 2: A) Baseline macular OCT cross-sectional scans showing hyporeflective attenuations in the outer retina, including the ELM, EZ, IZ, and RPE in both eyes; B) Follow-up OCT scans showing large improvements in 6 months in both eyes. Note: OCT: Optical Coherence Tomography; ELM: External Limiting Membrane; EZ: Ellipsoid Zone; IZ: Interdigitation Zone; RPE: Retinal Pigment Epithelium.
To our best knowledge, this is the first report to describe a case of ARPE or Krill’s disease, identified two weeks following COVID-19 infection in a healthy young adult. While its pathophysiology remains largely unproven, several studies in the literature have proposed a viral-associated inflammatory origin, given the acute occurrence of ARPE symptoms, such as scotomas and vision blurring, following flu-like symptoms [2,3,6,7,14]. Reports have documented cases of ARPE following COVID-19 vaccination in young adults who did not have viral-like illnesses or symptoms before or after administration, including an 18-year-old male from Japan and a 36-year-old male from Malaysia [11,12]. In the case of the 18-year-old, right eye central scotoma was observed following COVID-19 vaccination and post-vaccine low-grade fever for 2 consecutive days. Whereas for the 36-year-old, bilateral metamorphopsia was experienced after vaccination. Our case finding in the 19-year-old patient adds to the growing knowledge of an inflammatory ARPE origin, as the strong temporal relationship between COVID-19 infection and symptoms onset without vaccination highly suggests that the SARS-CoV-2 virus may have triggered an inflammatory mechanism in the retina, similar to those previously described.
The finding of spontaneous recovery without treatment are consistent with previous studies, which further confirms the selflimiting nature of this disease. However, the follow up imaging was performed at 6 months after the baseline visit, suggesting that we are only speculative about the time course of ARPE resolution in our patient, whereas most studies reported a recovery window between 6-12 weeks, thus this remains a study limitation [1,8,9]. Moreover, our patient demonstrated bilateral scotomas, which is consistent with some studies while most other studies have reported unilateral manifestations [1,2,7,11,12].
Consistent with many other reports, fundus imaging and FAF scans in our patient has demonstrated characteristic fine pigment stippling and surrounding hypopigmented halo with spontaneous recovery [2,11,12]. Also consistent with other studies were OCT findings of outer retina hyporreflectivity and attenuations, especially in the ELM, EZ, IZ and RPE retinal layers [12,15]. Notably, our imaging results were highly comparable to the report of the healthy 18-year-old patient following COVID-19 vaccination, which suggests that the SARS-CoV-2 virus, whether acquired through natural infection or artificially-acquired immunity, could trigger a common inflammatory pathway leading to ARPE manifestations [12]. The underlying biochemical mechanisms leading to the structural changes in ARPE may involve the RPE’s phagocytotic process of spent Photoreceptor Outer Segment (POS) fragments and the role of the Mer Tyrosine Kinase (MerTK), as the RPE is responsible for the continuous renewal and survival of the photoreceptor outer segment for rods and cones [16-19]. The hyperreflectivity in the outer retinal layers as observed from OCT scans may be attributed to spent POS accumulation and MerTK deficiency, which could be some of the downstream effects of viral-related inflammatory responses exhibited by the human immune system [15,20]. However, future studies are much needed to investigate this cellular pathway and to fully understand the pathophysiology of ARPE.
This is the first case report describing the temporal relationship between COVID-19 infection and ARPE in a healthy young adult. The successful management with only observation provides key information on the natural course of Krill’s disease in the context of COVID-19 infection. The findings here would contribute to the growing knowledge of ocular manifestations post COVID-19 infection as we propose a potential immune-mediated mechanism in ARPE pathogenesis. More importantly, this study underscores the importance for clinicians to consider Krill’s disease as a potential differential diagnosis when patients, particularly young adults, are presented with acute visual disturbances following COVID-19 infection or vaccination.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Ji PX, Koushan K, Sivachandran N (2024). Acute Retinal Pigment Epitheliitis Following COVID-19 Infection: A Case Report. J Clin Exp Ophthalmol. 15:994.
Received: 23-Oct-2024, Manuscript No. JCEO-24-34775; Editor assigned: 25-Oct-2024, Pre QC No. JCEO-24-34775 (PQ); Reviewed: 11-Nov-2024, QC No. JCEO-24-34775; Revised: 18-Nov-2024, Manuscript No. JCEO-24-34775 (R); Published: 25-Nov-2024 , DOI: 10.35248/2155-9570.24.15.994
Copyright: © 2024 Ji PX, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.