Gynecology & Obstetrics
Open Access
ISSN: 2161-0932
ISSN: 2161-0932
Research - (2020)Volume 10, Issue 2
Title: Alcohol Consumption and the Development of High-Grade Cervical Dysplasia.
Objective: To investigate the association between alcohol consumption and the prevalence of high grade cervical intraepithelial neoplasia in Duke University cervix clinic patients.
Methods: Patients presenting to Duke University Cervix Clinic between the ages of 21 and 65 meeting inclusion criteria were identified and approached to participate in the study. Once consented, patients completed the Alcohol Use Disorders Identification Test (AUDIT) validated survey. The primary outcome was defined based on colposcopically directed biopsy results. Patients with no Cervical Dysplasia or low-grade dysplasia (CIN 1) were placed in one group and those with high-grade dysplasia (CIN 2-3) were placed in the other. Demographic information including age, ethnicity, BMI, smoking history, and several sexual partners were collected. Demographics and patients with harmful alcohol use (AUDIT score of 8 or higher) were compared between the two groups.
Results: Forty-four patients met eligibility criteria and completed the electronic AUDIT survey. Due to a programming error in the RedCap AUDIT questionnaire, 9 surveys were excluded from further analysis. Among 35 patients included in the analysis, 20 patients (57.1%) patients had low grade or no cervical dysplasia and 15 (42.9%) had high-grade dysplasia. The proportion of patients with hazardous and harmful alcohol use among those with mild or no cervical dysplasia was 5% (n=1) compared to 6.7% (n=1) among those with high-grade cervical dysplasia. There was no significant association between alcohol use and Cervical Dysplasia (p=1.00). There was a significant association between race and high-grade cervical dysplasia (p=0.001).
Conclusion: In this small pilot study, no statistically significant association was noted between alcohol use per patient’s AUDIT scores and cervical dysplasia. Larger studies are needed to look at this modifiable behavior in decreasing the prevalence of high-grade cervical dysplasia and cervical cancer.
Alcohol; Cervical dysplasia; Cancer; AUDIT
Cervical cancer is the third most common gynecologic cancer diagnosis and cause of death among gynecologic cancers in the United States. Approximately 13, 000 new cases of cervical cancer are diagnosed yearly in the United States with over 400 deaths per year. Cervical Intraepithelial Neoplasia (CIN), also known as cervical dysplasia, typically precedes the development of invasive cervical cancer. Infection with the oncogenic subtype(s) of the Human Papilloma Virus (HPV) is one of the most notable risk factors for the development of precancerous cervical intraepithelial neoplasia and/or invasive cervical cancer. Additional risk factors include multiple sexual partners, unprotected intercourse, and cigarette smoking. Alcohol use is associated with the development of multiple cancers through the mechanism of DNA damage caused by acetaldehyde, alcohol derived metabolite. Acetaldehyde, in turn, causes doublestranded DNA breaks that can lead to chromosome rearrangements and ultimately, cancer [1]. Specifically, excessive alcohol use has been shown to increase rates of other HPV related cancers, such as Oropharyngeal cancer. Interestingly, the relationship between alcohol use and cervical dysplasia has not yet been studied extensively among diverse patient populations. One Korean study published in 2013 found that alcohol consumption was associated with an increased risk of CIN 1. No association was noted between alcohol consumption and CIN 2, CIN 3, or cervical cancer [1-8].
According to the National Institute of Alcohol Abuse and Alcoholism, approximately 5.3 million American women drink in a way that threatens their “health, safety, and general wellbeing”. Thus, the goal of this pilot study was to investigate the association between alcohol consumption and high grade cervical intraepithelial neoplasia in Duke University cervix clinic patients.
This study was approved by the Duke University Hospital Institutional Review Board on November 15, 2018. Patients who met inclusion criteria were approached before or after their scheduled outpatient appointments in the Duke University Cervix Clinic. To be eligible for the study, patients had to be at least 21 years of age and less than 65 years of age and have the ability to read and understand English. New patients presenting for colposcopy in the setting of an abnormal Pap or HPV test result and return patients with a documented colposcopy biopsy result within 12 months from the recruitment date were eligible for study participation. Patients were excluded if they could not give legal consent. Colposcopy biopsy results could be no cervical dysplasia, CIN-1 CIN-2, or CIN-3. Once patients were deemed to meet inclusion criteria, they were approached by a medical care provider or a member of the study team regarding the study. Once informed consent was obtained, the participants were asked to complete the Alcohol Use Disorders Identification Test (AUDIT), a World Health Organization validated alcohol use screening questionnaire6.The AUDIT questionnaire contains 10 questions that represent three different domains: alcohol consumption (questions 1-3), alcohol dependence (questions 4-6), and alcohol-related consequences (questions 7-10). Scores can range from 0 to a maximum of 40. Total scores of 8 or more were considered an indication of “ hazardous and harmful ” alcohol use, per the questionnaire developers. The questionnaire was administered in the form of an electronic REDCap survey on a secure password-protected, encrypted tablet. Demographic data including age, diagnosis, race/ethnicity, smoking status/history, and several sexual partners was obtained from a review of the electronic medical record and entered into a REDCap database. There was no financial cost to the participants for study participation and they were not compensated financially for their participation.
Statistical analysis
A total of 44 participants were recruited between November 2018 and March 2019. Due to a programming error in the electronic AUDIT questionnaire, 9 entries were excluded from statistical analysis, leaving a total of 35 participants for analysis. The primary outcome was high-grade cervical dysplasia (CIN 2-3) versus low-grade cervical dysplasia (CIN-1 or no dysplasia). The patient characteristics including age, race, BMI, smoking status, and several sexual partners were summarized using the median with Interquartile Range (IQR) or the frequency with percentage. Wilcoxon rank-sum tests were used to assess the association between the continuous variables (age and BMI) and the primary outcome. Fisher’s exact test was used to assess the association between the categorical variables (race, smoking status, and several sexual partners) and the primary outcome. The primary analysis to investigate the association between hazardous or harmful alcohol use (AUDIT score ≥ 8) and the primary outcome included Fisher’s exact test. Furthermore, we explored the association between AUDIT questionnaire scores as a discrete variable and the primary outcome using the Wilcoxon rank-sum test. All statistical analyses were performed using R 3.5.07.
Of the 35 patients included in this preliminary analysis, 9 patients had no cervical dysplasia, 11 patients had mild cervical dysplasia CIN-1, 8 had moderate cervical dysplasia CIN-2, and 7 patients had severe cervical dysplasia CIN-3 Thus, approximately 57.1% (20 patients) were in the low-grade dysplasia group and 42.9% (15 patients) were in the high-grade dysplasia group.
The median age of the cohort was 30 (IQR 28, 44) with a similar median age between the two groups (p=0.84). The median BMI and proportion of smokers were also similar between the two groups.
Approximately 55% identified as White in the low-grade dysplasia group and 86.7% of patients identified as Black in the high-grade dysplasia group. There was a statistically significant association between race and high-grade cervical dysplasia (p=0.001). Table 1 below demonstrates the differences in the above mentioned patient characteristics in each group.
| Characteristics | Low-grade cervical dysplasia | High-grade cervical dysplasia | Total | p-value |
|---|---|---|---|---|
| (n=20) | (n=15) | (n=35) | ||
| Age, median (IQR) | 30.5 (27.5, 49) | 29 (28, 44) | 30 (28, 44) | 0.84 |
| Race | 0.001 | |||
| White | 11 (55%) | 0 (0%) | 11 (31.4%) | |
| Black | 7 (35%) | 13 (86.7%) | 20 (57.1%) | |
| Other* | 2 (10%) | 2 (13.3%) | 4 (11.4%) | |
| BMI, median (IQR) | 27.8 (23, 33.5) | 30 (21.8, 33) | 29 (23, 33) | 0.84 |
| Smoker (past or present) | 10 (50%) | 9 (60%) | 19 (54.3%) | 0.73 |
| Number of sexual partners | 0.05 | |||
| 0-5 | 14 (70%) | 6 (40%) | 20 (57.1%) | |
| 6-10 | 2 (10%) | 7 (46.7%) | 9 (25.7%) | |
| >10 | 4 (20%) | 2 (13.3%) | 6 (17.1%) | |
*included Asian, Native American/Alaska Native, Hispanic, American Indian/Caucasian
Table 1: Patient characteristics by Cervical Dysplasia.
The proportion of patients with hazardous and harmful alcohol use among those with low-grade dysplasia was 5% (n=1) and 6.7% (n=1) among those with high-grade dysplasia.
There was no statistically significant association between hazardous and harmful alcohol use and cervical dysplasia (p=1.00) as shown in Table 2.
| Low-Grade Cervical Dysplasia | High-Grade Cervical dysplasia | p-value | |
|---|---|---|---|
| (n=20) | (n=15) | ||
| Hazardous and harmful alcohol use | 1 (5%) | 1 (6.7%) | 1 |
| AUDIT total score, median (IQR) | 1 (0.8, 2.2) | 1 (0, 2) | 0.37 |
Table 2: Association between alcohol use and cervical dysplasia.
The median AUDIT score was 1 (IQR 0.8, 2.2) in the low-grade dysplasia group compared to the median of 1 (IQR 0, 2) in the high-grade dysplasia group.
There was no statistically significant association between AUDIT total score and cervical dysplasia (p=0.37). This information is displayed in Figure 1.
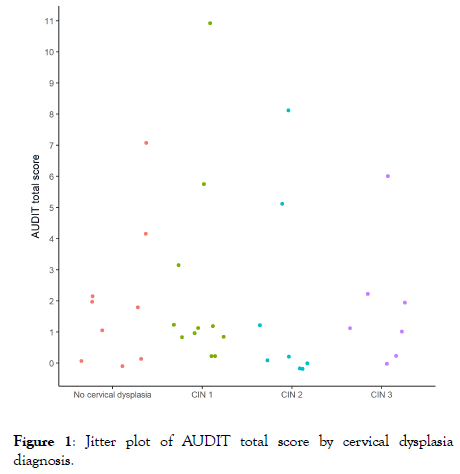
Figure 1: Jitter plot of AUDIT total score by cervical dysplasia diagnosis.
In this pilot study of 35 patients, no statistically significant association was noted between AUDIT scores and high-grade cervical dysplasia. There was a statistically significant association between race and high-grade dysplasia (p=0.001) with approximately 86.7% of the high-grade cervical dysplasia group identifying as black. While this study did not show any statistical significance concerning the primary outcome, there were multiple limitations. First, we are underpowered to detect any significant association that does exist between alcohol use and cervical dysplasia with a small sample size of 35 participants. Second, it is possible that few participants not have accurately answered the AUDIT questionnaire surveys due to fear of judgment given the perceived stigma associated with alcohol use. Some studies suggest underreporting of alcohol consumption can be a result of multiple factors. For example, one study based on registry data suggests that heavy drinkers are less likely to participate in alcohol use surveys altogether. Another potential contributor to the underreporting of alcohol consumption in surveys is inaccurate responses due to recall bias. Stockwell et al. demonstrated that survey questions asking respondents for measures of alcohol consumption over shorter time intervals provided more accurate objective measures of consumption than those asking respondents to summarize drinking patterns over 12 months.
Given the small sample size of 35 participants in this pilot study, we will continue to recruit participants for a maximum of 100 participants. Multiple small scale studies have been conducted that demonstrate some degree of association between alcohol consumption and cervical intraepithelial neoplasia such as the earlier cited Korean study demonstrating an increased risk of CIN 1 with alcohol use. KOrywal et al. found in their 43 patient, 2016 study increased alcohol dehydrogenase levels (ADH) and aldehyde dehydrogenase levels (ADLH) in cervical cancer patients, suggesting a potential role of ADH 1 as a marker for cervical cancer. In conclusion, the conduction of larger studies is needed to more closely evaluate alcohol consumption in decreasing the incidence of high-grade cervical dysplasia and cervical cancer.
Citation: Abdalla AE, Truong T, Gallagher J, Schmitt JW (2020) Alcohol Consumption and the Development of High-Grade Cervical Dysplasia. Gynecol Obstet (Sunnyvale) 10:519. doi: 10.35248/2161-10932.20.10.519
Received: 03-Feb-2020 Accepted: 10-Feb-2020 Published: 17-Feb-2020 , DOI: 10.35248/2161-10932.20.10.519
Copyright: © 2020 Abdalla AE, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.