Medical & Surgical Urology
Open Access
ISSN: 2168-9857
ISSN: 2168-9857
Research Article - (2020)Volume 9, Issue 4
Objective: To assess the efficacy of Amikacin as the anti-biotic of least recorded resistance locally in preventing urinary infective episodes following ESWL (Extracorporeal Shock Wave Lithotripsy) in patients with DJ stents in-situ.
Materials and methods: A retrospective review of a cohort of 60 adult patients with upper urinary tract calculi and DJ stent in-situ, who received one dose of Amikacin intravenously immediately before ESWL was carried out. All patients had a documented negative urine culture prior to ESWL. The incidence rate of post ESWL bacteriuria was calculated and compared to the published incidence rates of bacteruria patients who did not receive any prophylaxis.
Results: A total number of 60 adult patients with DJ stent in-situ, who received Amikacin prophylaxis, underwent ESWL between the 1st of January 2017 and the 31st of December 2017. All of the 60 patients had a documented negative urine culture pre-ESL. Two patients were found to have positive urine culture post ESWL with an incidence rate of 3.33. This was not statistically different to the published percentage of patients who received no prophylaxis in the compared studies that showed incidence rates of 3.08 and 2.17 respectively (Chi-square=0.704, p=0.703).
Conclusion: Intravenous Amikacin prophylaxis was not efficacious in reducing UTI and urinary sepsis following ESWL in patients with DJ stents in-situ, despite being the antibiotic of least resistance locally.
Extracorporeal Shock Wave Lithotripsy (ESWL); Prophylaxis; Antibiotics in ESWL; Amikacin pre ESWL; ESWL with DJ stent
Urinary Tract Infections (UTI) and urinary sepsis are recognized complications of ESWL treatment. The reported UTI rate following ESWL is widely variable in the published literature ranging between 0% and 28% [1-6]. There was no clear distinction in most of the studies between asymptomatic bacteruria and UTI. The severity of post ESWL infective episodes can be very variable. In this regard, few authors reported occasional life threatening infective complications following ESWL leading to systemic, brain and cardiac sepsis with patients ended up being admitted to ITU following this outpatient procedure [7-9]. Nevertheless, these case reports have not tipped the balance towards the routine use of antibiotic prophylaxis.
As a means of avoiding or at least limiting UTI and urinary sepsis, anti-biotic prophylaxis was suggested by many authors [6,9-11]. There was a clear heterogeneity between the studies in terms of the anti-biotic agents used as well as the regimens and durations that ranged between a single dose to a full week’s course [12].
The presence of an indwelling ureteric stent is regarded as being more indicative of using pre-ESWL anti-biotic prophylaxis [13,14]. This can be attributed to the increased likelihood of bacterial colonization and biofilm formation on the surface of DJ stents.
Guided by our own local hospital anti-biogram, it was our practice to give one dose of Amikacin 500 mg intravenously immediately before ESWL sessions for those patients with indwelling ureteric (DJ) stents. Amikacin was reported to be the anti-biotic of least resistance when used for UTI in our hospital with efficacy rate of around 91%. In terms of cost, Amikacin was cheaper compared to Ciprofloxacin and Levofloxacin which were the nearest in terms of efficacy.
This study aimed at assessing the efficacy of Amikacin as the anti-biotic of least recorded resistance locally in preventing urinary infective episodes following ESWL
A retrospective review of a cohort of 60 adult patients with DJ stent in-situ was done between the 1st of January and the 31st of December 2017. All patients received one dose of Amikacin intravenously immediately before ESWL was carried out. All patients had a recorded negative urine culture prior to the ESWL session. All medical records of the included patients were reviewed including laboratory and imaging reports. 36 patients (60%) underwent ESWL for renal stones, while 24 patients (40%) for upper ureteric stones. 22 patients (36.7%) received a different treatment modality prior to ESWL (eg. PCNL or ureteroscopy). All patients were admitted to the day care unit on the morning of ESWL. An agreed analgesia protocol consisted of 1 g intravenous Paracetamol in addition to 100 mg of Diclofenac suppository for all patients unless there was a contraindication. An intravenous dose of 500 mg Amikacin was given to all patients as there was no contra-indication such as allergy or inadequate renal function reserve. The dose was administered as slow infusion over 30 min in 100 mL of normal Saline. The incidence rate of bacteruria post ESWL was calculated and compared to the incidence rates in the published literature of patients who did not receive any prophylaxis and found to have bacteruria [15].
A total number of 60 adult patients with DJ stent in-situ, who received Amikacin prophylaxis, underwent ESWL between the 1st of January 2017 and the 31st of December 2017, with an age range of (20 to 85 years). 43 patients (72%) were males, while 17 patients (28%) were females. Out of the total number, two patients (3.3%) were found to have positive bacterial growth in their first recorded urine culture after ESWL; both of these patients were asymptomatic. None of these two patients with positive bacterial growth had a co-morbidity that predisposes to UTI such as immuno-compromized state or Diabetes. Compared to a large prospective study that enrolled 389 patients showing a bacteruria incidence rate of 3.08 among patients who received no prophylaxis, as well as another study of 413 patients with a bacteruria rate of 2.17, our reported bacteruria rate of (3.3) was not statistically different, with a Chi-square of 0.74 and P value of 0.73 (Figure 1), below illustrates the post ESWL bacteruria incidence among the three studies.
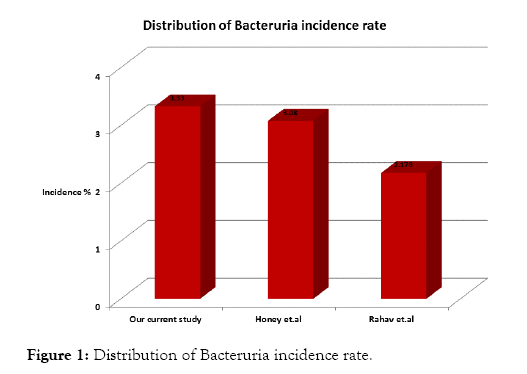
Figure 1: Distribution of Bacteruria incidence rate.
There is currently no controversy about the clinical principle of having a documented negative urine culture prior to any stone clearance procedure as per the major guidelines [12,13].
Similarly, there is a largely shared expert opinion of giving pre- ESWL anti-biotic prophylaxis to patients with stones that are thought to be of infective aetiology (e.g. stag horn), as well as patients who have any form of drainage catheters such as nephrostomies and DJ stents. On the other hand, the opinion is divided regarding the use of prophylaxis in the cases that are neither infective stones, nor stent or nephrostomy bearing. The new generations of ESWL machines are more patientfriendly in terms of analgesia requirements. Moreover, most of the new generations can now be used even in patients with pace makers. Another factor that made ESWL more attractive option is the fact that it eliminates the anaesthetic risk in patients with co-morbidities [15].
In an attempt to limit the number of variables in the equation, we designed this study to specifically include patients with DJ stents who are in general believed to be at higher risk of infection. To ensure the best prophylactic effect, we used the anti-biotic of least recorded local resistance as per the hospital’s antibiogram, which was Amikacin.
In terms of results comparison, we identified two previous studies, both of which had a good sample size of 389 and 413 respectively [4,5]. These studies represented the control arm to our study, as none of the participants in both studies received prophylaxis. Table 1 below summarizes the features of these studies. Another large meta-anlysis of eight randomized controlled studies with a total of 885 patients, and six clinical series (non-randomized) of 597 patients, showed a median probability of UTI of 2.1% among patients who received a large variety of anti-biotics with different spectra of actions [6]. The results from this meta-analysis concur favourably with our study in terms of UTI incidence, considering the difference in the population number. The shared concepts between our study and both other studies in comparison [4,5] were the documentation of negative pre- ESWL culture and the assessment of post ESWL UTI bacteruria. These factors, made the comparison of results justified and meaningful.
| Study | Current study | Honey, et al. | Rahav, et al. |
|---|---|---|---|
| Type | Retrospective | Prospective | Retrospective |
| Number of participants | 60 | 526 | 413 |
| Prophylaxis agent | Amikacin (locally agreed) | None | None |
| Bacteruria incidence rate | 3.33 | 3.08 | 2.179 |
Chi-square =0.704, p=0.703
Table 1: Main features of studies.
Our study carried some novelty in applying the principle of using the most efficient anti-biotic locally rather than empirical agents, however it has the limitations of having a relatively small sample size as well as lacking another arm of stented patients in whom no prophylaxis was used.
Our results appear to concur with the major guidelines’ (EAU and AUA after 2012 amendment) advice against the empirical use of pre-ESWL anti-biotic prophylaxis to all patients. Moreover, our study goes further to confirm that no prophylaxis is required even for patients with DJ stents.
Citation: Ebrahim Rafie MAM, Alnaib Z, Aljuboori Z, Osman E (2019) Amikacin as the Most Potent Antibiotic Locally, is it Required Prior to Extracorporeal Shock Wave Lithotripsy (ESWL) in Patients with Double J Stents?. Med Sur Urol 8:215. doi: 10.35248/2168-9857.19.8.215
Received: 06-Aug-2020 Accepted: 18-Sep-2020 Published: 25-Sep-2020 , DOI: 10.35248/2168-9857.20.9.215
Copyright: © 2019 Ebrahim Rafie MAM, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.