
Anesthesia & Clinical Research
Open Access
ISSN: 2155-6148

ISSN: 2155-6148
Research Article - (2023)Volume 14, Issue 6
Introduction: Analgesia following knee replacements has been evolving, with peripheral nerve blocks gaining precedence over central neuraxial techniques. Good surgical outcomes rely on early rehabilitation, necessitating the need for good pain relief without motor blockade. Current evidence supports regional analgesia with an adductor canal catheter, in conjunction with an iPACK block (infiltration between popliteal artery and the capsule of knee joint).
Methodology: We describe a fascial plane block between the medial head of gastrocnemius and the soleus muscles in the leg. Anatomic continuity of this plane with the space surrounding the knee joint capsule (in keeping with existing literature regarding the deep fascia of the leg) was established following a cadaveric demonstration, wherein dye injection was done under ultrasound guidance approximately 7 cm-8 cm distal to the joint line. Subsequent dissection till the popliteal fossa revealed staining over the capsule, where the genicular nerves enter the knee joint. We hypothesized that the target site of drug spread with the iPACK (i.e., the posterior capsule of the knee joint) is similar to that obtained when drug is injected in the fascial plane between the medial gastrocnemius head and soleus muscles, thus conferring equivalent analgesia with negligible risk of motor involvement and vascular puncture.
Results: A pilot study, comparing the iPACK and the gastrosoleus interfascial plane blocks, was performed in 22 patients undergoing total knee replacement surgeries. These blocks were given along with an adductor canal catheter for all patients. Postoperative pain scores and motor power were assessed at fixed intervals.
Conclusion: We observed similar posterior knee analgesia postoperatively with use of the gastrosoleus interfascial block as compared to the iPACK. Consistent drug spread towards the knee joint was observed on ultrasound following each block. No motor involvement was observed with any of the patients who received the gastrosoleus block. Catheter placement for continuous analgesia can also be done safely in this fascial plane.
Regional anasthesia; Knee replacement surgery; IPACK; Fascial plane block, Motor sparing; Cadaveric study
The knee joint, with its complex innervation, has long been a subject of interest for regional anaesthetists. Latest evidence supports the use of an adductor canal catheter with an iPACK block (for the sciatic component) for knee replacement surgeries. The trend from epidurals to femoral catheters in conjunction with sciatic nerve blocks and recently, to adductor canal catheters with the iPACK block, has evolved in order to obtain better outcomes in terms of satisfactory pain scores while ensuring early rehabilitation [1].
The iPACK block, described by Sanjay Sinha in 2012, effectively addresses posterior knee pain following arthroplasties by aiming for the articular branches of the sciatic and obturator nerves, thus sparing the main trunks. However, there have been certain case reports of foot drop following the iPACK block [2].
In this report, we describe a fascial plane block between the gastrocnemius and soleus muscles in the leg, as an alternative to the iPACK in achieving posterior knee analgesia. Our study is based on the myofascial continuity between the leg and the knee joint, thereby facilitating drug spread within the posterior aspect of the knee. We hope to provide equivalent analgesia as compared to the iPACK, along with a superior safety profile in terms of motor blockade and inadvertent vascular injury [3].
A demonstration of the gastrosoleus interfascial block was initially performed in two cadaveric leg specimens to establish the anatomical basis of this study. The cadaveric dissection was done in the department of anatomy at the Christian medical college, Vellore, India in July-August 2022.
Steps of dissection
Formalin fixed cadavers were used for dissection. The leg was placed in anatomical position. Under initial ultrasound guidance, 30 mL of methylene blue dye was injected approximately 8 cm below the popliteal crease at the medial border of the leg, between the medial head of the gastrocnemius and the soleus muscles. A 20G epidural catheter was inserted and left at a length of 10 cm into this plane using an 18G Tuohy needle [4].
After 15 minutes, the leg was approached from the posterior aspect. A horizontal incision was made at the junction of the lower and middle third of the thigh with a similar incision at the junction of the upper and middle third of the leg. An incision along the medial border connecting the upper and lower incisions enabled us to approach the popliteal fossa from the medial aspect by raising a wide flap. Superficial fascia was dissected while preserving the superficial nerves and veins. The two heads of gastrocnemius were identified [5]. The fossa was cleared of fat to visualize the neurovascular structures, specifically looking for the sciatic nerve and its branches. Dye staining was observed at the articular branches of the sciatic nerve over the posterior capsule of the knee joint. The attachment of the medial head of gastrocnemius to the femoral condyle was identified. The medial head of the gastrocnemius was cut below the level of the popliteal fossa and reflected to visualize the intermuscular plane between the gastrocnemius and soleus, where significant staining by the dye was observed [6]. The anatomic dissection has been illustrated in Figures 1 and 2.
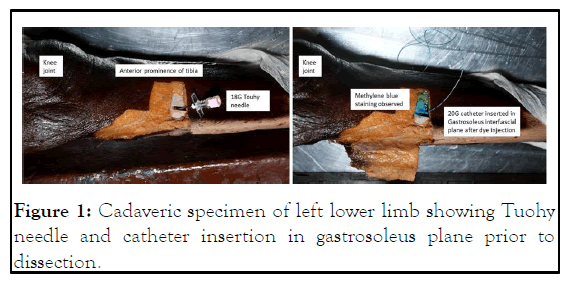
Figure 1: Cadaveric specimen of left lower limb showing Tuohy needle and catheter insertion in gastrosoleus plane prior to dissection.
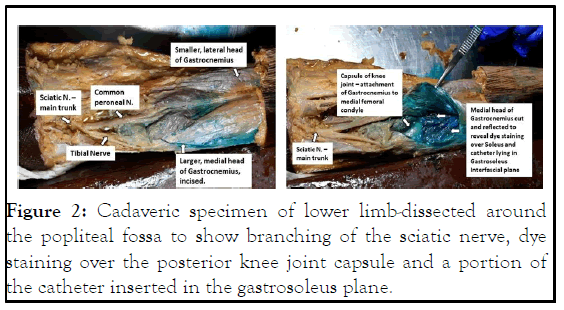
Figure 2: Cadaveric specimen of lower limb-dissected around the popliteal fossa to show branching of the sciatic nerve, dye staining over the posterior knee joint capsule and a portion of the catheter inserted in the gastrosoleus plane.
We extrapolated the findings from our cadaveric study into clinical practice, wherein we hypothesized that a volume of 30 mL of local anaesthetic injected in the fascial plane between the medial gastrocnemius head and the soleus muscles should successfully reach and block the genicular nerves entering the posterior capsule of the knee joint [7].
Patients undergoing total knee replacement surgeries, between September, 2022-May, 2023, admitted to the Christian medical college, Vellore, were assessed preoperatively and recruited for this pilot study. Written informed consent was taken for general anaesthesia during the surgery and regional analgesia for the postoperative period with a continuous adductor canal block and a posterior compartment block (Gastrosoleus or iPACK), along with an intravenous patient controlled analgesia pump. The PCA pump contained fentanyl in a concentration of 20 mcg/mL and the basal rate was set as zero, allowing only boluses to be delivered for breakthrough pain. Recruited patients belonged to ASA-PS classes 1-3 and were without coagulation abnormalities [8].
We randomized patients into two groups, 1 and 2, by coin toss method on the day of surgery. Patients in group 1 received the gastrosoleus block while those in group 2 received the iPACK block, prior to surgery. Those undergoing surgery for bilateral knees received the same block as per randomization for both sides. An adductor canal catheter was placed postoperatively for all patients. They were assessed for pain scores and localization of pain initially in the post anaesthesia care unit. They were also assessed in the ward at 8, 16 and 24 hours post-surgery by a designated anaesthesiologist among the authors who was blinded to the block performed [9]. The patient was also blinded to the block received. The type of surgery, volume and nature of local anaesthetic administered is depicted in Table 1.
| S.no | Date | Surgery | Drug given |
|---|---|---|---|
| 1 | 25/09/22 | Bilateral TKR | 30 mL 0.2% ropivacaine with 15 mcg dexmedetomidine on each side |
| 2 | 25/09/22 | Bilateral TKR | 30 ml 0.2% ropivacaine with 15 mcg dexmedetomidine on each side |
| 3 | 29/09/22 | Left TKR | 20 ml 0.2% ropivacaine with 20 mcg dexmedetomidine |
| 4 | 01/10/22 | Right TKR | 30 mL 0.2% ropivacaine with 25 mcg dexmedetomidine |
| 5 | 01/10/22 | Right TKR | 20 mL 0.2% ropivacaine with 20 mcg dexmedetomidine |
| 6 | 01/10/22 | Left TKR | 20 mL 0.2% ropivacaine with 25 mcg dexmedetomidine |
| 7 | 05/11/22 | Right TKR | 30 mL 0.2% ropivacaine with 25 mcg dexmedetomidine |
| 8 | 12/12/22 | Bilateral TKR | 20 mL 0.2% ropivacaine with 30 mcg dexmedetomidine on each side |
| 9 | 12/12/22 | Left TKR | 30 mL 0.2% ropivacaine with 25 mcg dexmedetomidine |
| 10 | 15/12/22 | Bilateral TKR | 20 mL 0.2% ropivacaine with 20 mcg dexmedetomidine on each side |
| 11 | 19/12/22 | Right TKR | 20 mL 0.2% ropivacaine with 20 mcg dexmedetomidine |
| 12 | 19/12/22 | Right TKR | 20 mL 0.2% ropivacaine with 20 mcg dexmedetomidine |
| 13 | 26/12/22 | Bilateral TKR | 20 mL 0.2% ropivacaine with 20 mcg dexmedetomidine on each side |
| 14 | 11/01/23 | Left TKR | 30 mL 0.2% ropivacaine with 25 mcg dexmedetomidine |
| 15 | 18/01/23 | Bilateral TKR | 20 mL 0.2% ropivacaine with 20 mcg dexmedetomidine on each side |
| 16 | 06/02/23 | Right TKR | 30 mL 0.2% ropivacaine with 25 mcg dexmedetomidine |
| 17 | 17/02/23 | Bilateral TKR | 30 mL 0.2% ropivacaine with 25 mcg dexmedetomidine |
| 18 | 17/02/23 | Bilateral TKR | 20 mL 0.2% ropivacaine with 20 mcg dexmedetomidine on each side |
| 19 | 20/03/23 | Right TKR | 30 mL 0.2% ropivacaine with 25 mcg dexmedetomidine |
| 20 | 27/04/23 | Left TKR | 30 mL 0.2% ropivacaine with 25 mcg dexmedetomidine |
| 21 | 04/05/23 | Right TKR | 30 mL 0.2% ropivacaine with 25 mcg dexmedetomidine |
| 22 | 04/05/23 | Left TKR | 30 mL 0.2% ropivacaine with 25 mcg dexmedetomidine |
Table 1: Details of surgery and drug given.
Description of technique
The posterior compartment block (Gastrosoleus interfascial, or iPACK) was administered prior to surgery for each patient. For both blocks, the patients were supine, with the limb to be blocked kept slightly flexed at the knee and externally rotated at the hip. An initial scout scanning, using a high frequency (6 MHz-15 MHz) linear probe, at the popliteal fossa was done for all patients to obtain a primary image. Both blocks were administered using the same probe [10]. Ideal ergonomics would have the anaesthesiologist at the side of the leg to be blocked, facing the ultrasound machine (Sonosite) placed at the opposite side of the bed. Time taken for performance of each block was noted.
For patients randomized to group 1, the transducer was placed along the medial border of the leg in long axis, 7 cm-8 cm below the popliteal crease. Muscle bellies of the medial gastrocnemius head and the soleus were identified in this view [11]. A trilaminar fascial plane between these muscles was determined as the site of drug injection (Figure 3).
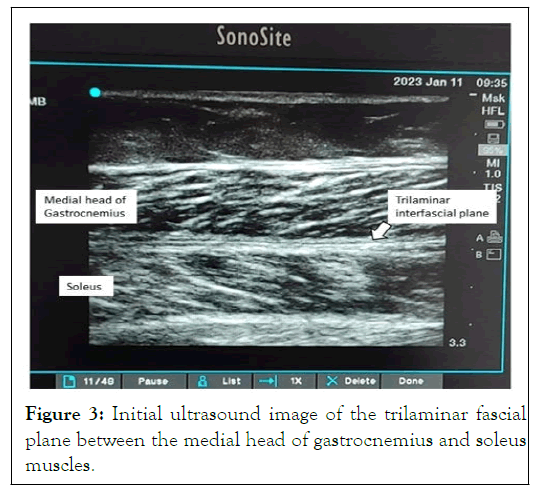
Figure 3: Initial ultrasound image of the trilaminar fascial plane between the medial head of gastrocnemius and soleus muscles.
The block was performed using a 22G stimuplex block needle, advanced from the end of the probe distal to the knee. Upon piercing the trilaminar fascia with a distinct loss of resistance, tip placement was confirmed using saline [12]. Once drug spread within the fascial plane was confirmed, 30 mL of 0.2% ropivacaine with 0.5 mcg/kg dexmedetomidine (as an additive) was injected after negative aspiration. During injection, the transducer probe was moved cranially in the same orientation to observe the limit of drug spread (Figure 4). At the end of drug administration, the ultrasound probe was placed in a transverse orientation at the popliteal crease and drug spread over the capsule of the knee joint was confirmed (Figure 5).
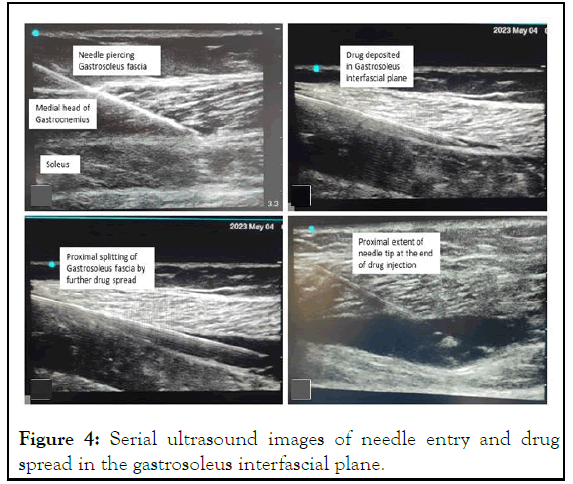
Figure 4: Serial ultrasound images of needle entry and drug spread in the gastrosoleus interfascial plane.
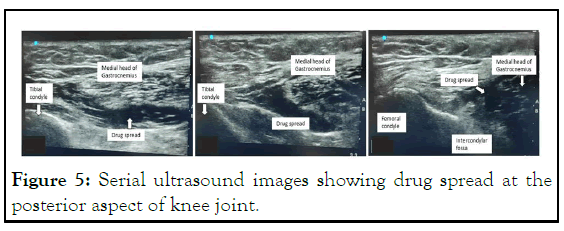
Figure 5: Serial ultrasound images showing drug spread at the posterior aspect of knee joint.
Patients randomized to group 2 received the iPACK block prior to surgery. The transducer probe was kept in a transverse orientation at the popliteal crease at the level of the femoral condyles. We performed a distal iPACK block, wherein the drug was injected between the popliteal artery and capsule of knee joint at the level of the intercondylar fossa. 20 mL of 0.2% ropivacaine with 0.5 mcg/kg of dexmedetomidine was injected from the medial aspect of the popliteal fossa [13].
All patients received general anaesthesia for the surgery. To minimise bias, the operating orthopaedic surgeons were requested not to perform periarticular infiltration into the posterior joint capsule of the knee intraoperatively. A 20G catheter was placed in the adductor canal under ultrasound guidance after surgery. In the post anaesthesia care unit, all patients were assessed for pain scores. They were examined for motor involvement (foot drop) to rule out blockade of the common peroneal nerve [14]. At the end of each surgery, a 20 mL bolus of 0.2% ropivacaine was given through the adductor canal catheter and continued 8th hourly. Assessment of pain scores and motor blockade was continued through postoperative day 1 and at the beginning of ambulation. The adductor canal catheters were kept in situ for 3-5 days postoperatively [15].
We performed the pilot study on a total of 22 patients undergoing total knee arthroplasty surgeries, among whom 8 patients had the surgery on both knees in the same sitting. Overall, the gastrosoleus block was administered to 12 patients, 3 of whom had bilateral surgery and the iPACK block was administered to 10 patients, 5 of whom had bilateral procedures. Assessment of pain in the PACU once the patient was fully awake was documented as pain score at 0 hour, following which the pain scores were recorded at 8, 16 and 24 hours in the ward [16].
We observed no significant difference in the mean pain scores among both groups at all intervals. The maximum mean pain score was 1.43 in the gastrosoleus group (at 16 hours) and 1.80 in the iPACK group (at 24 hours). No patient in either group reported a pain score of more than 4 at any point during their postoperative stay. 2 out of 10 patients who received the iPACK block had a foot drop that recovered within 24 hours. All patients were ambulated on their first postoperative day successfully. There were no incidences of vascular puncture or haematoma formation in any of the patients [17]. Mean pain scores at various intervals are depicted in Figure 6. The average time taken for performance of this block was 6 minutes.
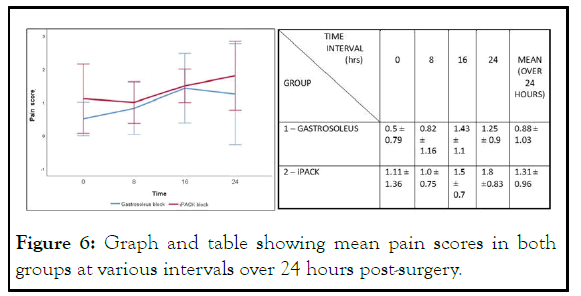
Figure 6: Graph and table showing mean pain scores in both groups at various intervals over 24 hours post-surgery.
A recent narrative review by the prospect group for pain management following total knee arthroplasty, recommends multimodal analgesia using a single dose adductor canal block preoperatively and intraoperative periarticular infiltration along with intravenous dexamethasone, paracetamol and nonsteroidal anti-inflammatory drugs. Opioids were to be reserved for rescue analgesia. The lack of mention of a continuous adductor canal block and the iPACK for posterior knee analgesia is due to a paucity of studies that meet the prospect methodology requirements.
Other regional analgesic techniques for knee arthroplasty include ultrasound guided genicular nerve blocks. However, they may not be visualised accurately and can result in inconsistent analgesia with use of low drug volumes. The popliteal plexus block and selective tibial nerve blocks have been employed with varying results. In our institute, continuous catheter analgesia through the adductor canal has been the protocol for pain management following knee replacement surgeries with good results. A single dose sciatic nerve block (using a low concentration, 0.05% ropivacaine) and more recently, the iPACK block, was added to address the posterior component of postoperative knee pain in the absence of periarticular infiltration.
The iPACK, a muscle-sparing technique, aims at blocking the articular branches of the sciatic and posterior division of the obturator nerve, supplying the posterior aspect of the knee. Its implementation in clinical practice has been seen to provide good postoperative pain scores with satisfactory recovery. A randomized controlled trial in 2018 inferred that the iPACK block when given proximally (level of injection at the distal femoral shaft, approximately one to two finger breadths above the patellar base) resulted in some of the injected drug spreading towards the main trunk of the common peroneal nerve, causing a foot drop. In contrast, a distal iPACK involves injection at the level of the upper part of the femoral condyles, with drug deposition in the intercondylar fossa between the popliteal artery and femoral condyles. Here, the common peroneal nerve has branched out completely and is superficial, lying away from the posterior capsule.
The need for an alternative to the iPACK block arose as a consequence of a few incidences of foot drop observed in patients undergoing knee arthroplasty surgeries at our institute. The proximity of the approaching needle to the popliteal vessels during administration of the iPACK block also raises a possibility of vascular puncture, although no instances of hematoma formation have been reported. We proposed to offer equivalent analgesia with a fascial plane block between the gastrocnemius and soleus muscles in the leg, distal to the knee joint, keeping in mind the anatomical feasibility of the same
Anatomy of the musculofascial compartment in the leg
The gastrocnemius muscle is comprised of a larger medial and smaller lateral belly at its origin from the respective femoral condyles. They converge distally to limit the lower triangle of the popliteal fossa. Both muscle bellies are in contact with the posterior capsule of the knee. At mid-calf level, the gastrocnemius aponeurotic fascia joins the deep fibres of the soleus to form the calcaneal tendon. The trilaminar appearance of this fascia on ultrasound is because of the thin tendon of the plantaris muscle that passes through it as it goes on to combine with the achilles tendon distally in the leg.
This anatomy enabled us to develop the gastrosoleus interfascial plane block with an expected target drug spread similar to that of the iPACK. As it is a fascial plane block, we used a higher volume of local anaesthetic (30 mL) as compared to 20 mL in the iPACK, wherein drug is deposited directly at the effect site. The plane between the medial gastrocnemius head and the soleus was considered ideal due to its relative prominence with respect to the less important lateral head and also to avoid drug spread towards the common peroneal nerve at the lateral end of the popliteal fossa. The point of needle insertion, i.e., 7 cm-8 cm distal to the popliteal crease on the medial border of the leg, was fixed as such owing to the formation of the Achille’s tendon by the triceps surae muscles approximately halfway down the leg.
The nearly identical pain scores obtained from both groups suggest that the gastrosoleus plane block is non-inferior to the iPACK in terms of analgesia, an expected outcome since the final effect site of local anaesthetic action, i.e., posterior capsule of the knee where the genicular nerves enter the joint, is believed to be the same for both. Although ambulation for all patients was satisfactory, the absence of foot drop among any of the patients who received the gastrosoleus block offers a superior safety profile. The intermuscular fascial plane forms a good seat for catheter placement in patients with fixed flexion deformities of the knee who have undergone significant posterior release requiring prolonged posterior analgesia.
We observed good analgesia with the gastrosoleus plane block. None of the patients reported a foot drop. Needle entry being away from the surgical site gained this block favour among the surgeons. The avascular nature of this fascial plane rules out vessel injury, rendering it safer for patients on anticoagulants. The relatively simple anatomy makes this block easier to reproduce among regional anaesthesia practitioners. It also offers the possibility of secure catheter placement. A randomised clinical trial comparing the efficacy and safety of this approach to the iPACK has been initiated in our institute to further establish the relevance of introducing this block in current practise.
I thank the department of anaesthesia, Christian medical college, Vellore, for their help and support in the completion of this research study. I am grateful for the encouragement by the head of the department of anaesthesia throughout the course of this study. I acknowledge the contribution of the anaesthesia consultants who were involved in the administration of regional nerve blocks. Special gratitude to the departments of orthopaedics, anatomy and biostatistics at the Christian medical college, Vellore, for their contribution and participation in this study.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Abraham RS, Pillai R, Cherian NE, George SP, Oommen AT, Charles AS (2023) Concept of a Novel Gastrosoleus Interfascial Plane Block and Comparison with the iPACK Block for Posterior Knee Pain Following Knee Replacement Surgeries-A Cadaveric Demonstration and Pilot Study. J Anesth Clin Res. 14:1122
Received: 26-Jun-2023, Manuscript No. JACR-23-25293; Editor assigned: 29-Jun-2023, Pre QC No. JACR-23-25293 (PQ); Reviewed: 13-Jul-2023, QC No. JACR-23-25293; Revised: 18-Aug-2023, Manuscript No. JACR-23-25293 (R); Published: 28-Dec-2023 , DOI: 10.35248/2155-6148.23.14.1122
Copyright: © 2023 Abraham RS, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use distribution, and reproduction in any medium, provided the original author and source are credited