Journal of Clinical and Experimental Ophthalmology
Open Access
ISSN: 2155-9570
ISSN: 2155-9570
Case Report - (2020)Volume 11, Issue 1
Rare idiopathic clinical entity, described by Chang et al. in 1995 for the first time, then in 2007 Samuel et al. published a classification according to the progressive stages of the disease. It is a condition which generally affects young women aged 30 to 40. Its evolution is variable and can be serious. Several therapeutic modalities are possible.
Atypical idiopathic retinal vasculitis; Neuroretinitis; Aneurysms
Herein, we report the case of a 45-year-old woman, with no notable general pathological or ophthalmological history, who consults for myodesopsia and visual blurring in the right eye, with rapid progression over 1 month.
The corrected visual acuity on admission was 8/10 OD and 10/10 OG.
The oculomotor examination including photomotor reflexe is normal.
The slit lamp examination (the anterior segment is normal with no signs of uveitis, no iridis rubeosis, normal eye pressure and a clear crystalline lens).
Examination of the anterior vitreous reveals a bilateral hematic Tyndall.
In the fundus examination, an intra vitreal and retrohyalohydian hemorrhage, spot hemorrhages and a vascular tortuosity, as well as the presence of uninhabited vessels and a typical peripheral fibrosis with a normal appearance of the macula and papilla in OD (Figure 1).
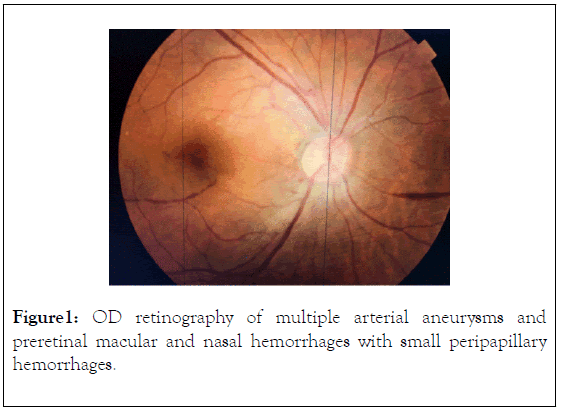
Figure 1. OD retinography of multiple arterial aneurysms and preretinal macular and nasal hemorrhages with small peripapillary hemorrhages.
In OS, we note the presence of intravitreal hemorrhage and fibrovascular traction with spot hemorrhages and normal appearance of the macula and papilla in OS (Figure 2).
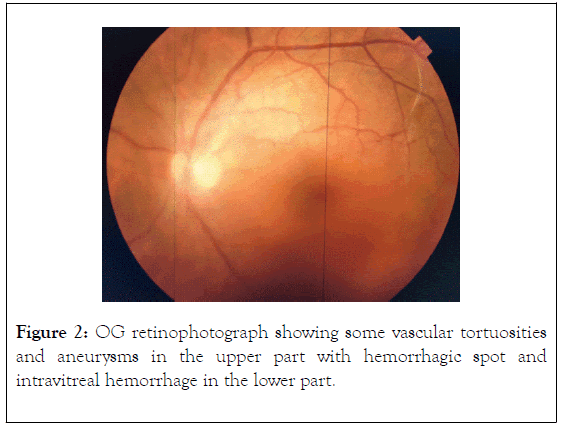
Figure 2. OG retinophotograph showing some vascular tortuosities and aneurysms in the upper part with hemorrhagic spot and intravitreal hemorrhage in the lower part.
Biological and radiological explorations have been carried out as part of the etiological diagnosis of a bilateral peripheral retinal ischemia complicated by neovascularization, tractional fibrosis and associated with vascular anomalies.
Nevertheless, the retinal photocoagulation treatment was carried out first (Figure 3).
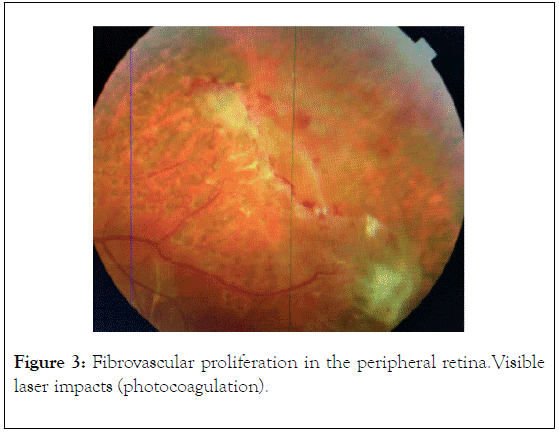
Figure 3. Fibrovascular proliferation in the peripheral retina.Visible laser impacts (photocoagulation).
Fluorescein angiography shows multiple vascular anomalies of arterial aneurysm at bifurcations with peripheral retinal ischemia and neovascularization with the aspect of sea fan and capillary and arteriolar leaks (Figures 4-9).
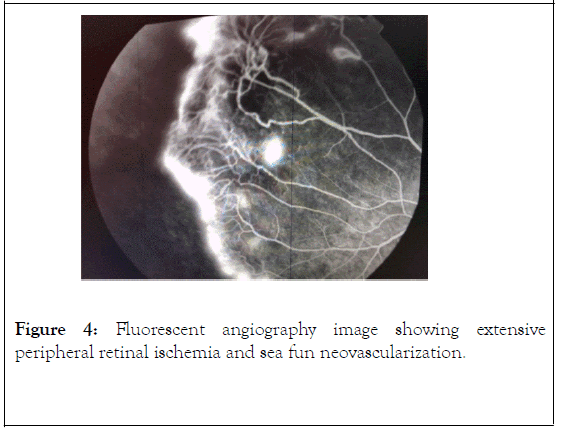
Figure 4. Fluorescent angiography image showing extensive peripheral retinal ischemia and sea fun neovascularization.
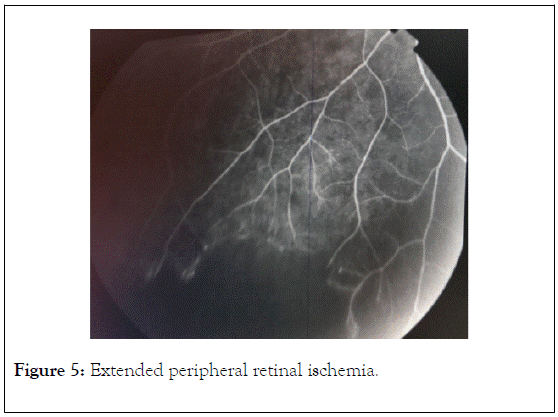
Figure 5. Extended peripheral retinal ischemia.
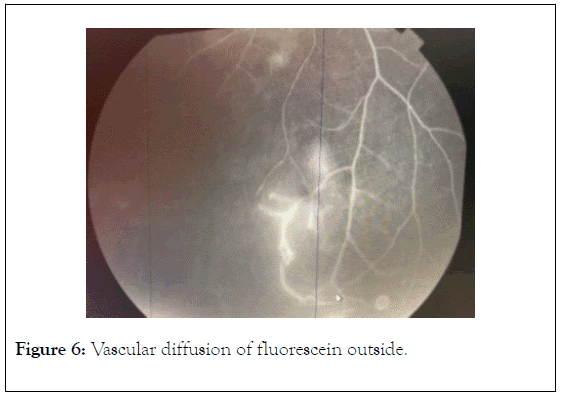
Figure 6. Vascular diffusion of fluorescein outside.
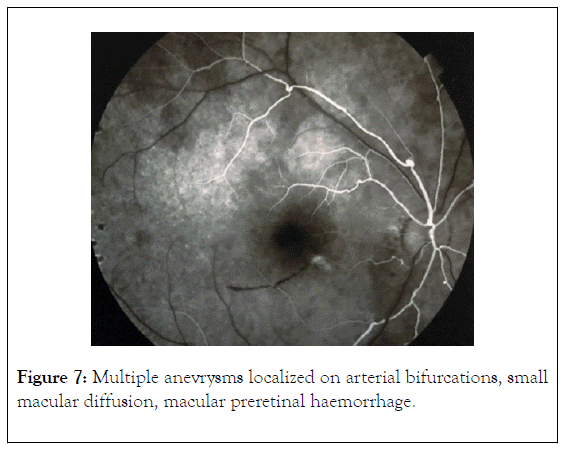
Figure 7. Multiple anevrysms localized on arterial bifurcations, small macular diffusion, macular preretinal haemorrhage.
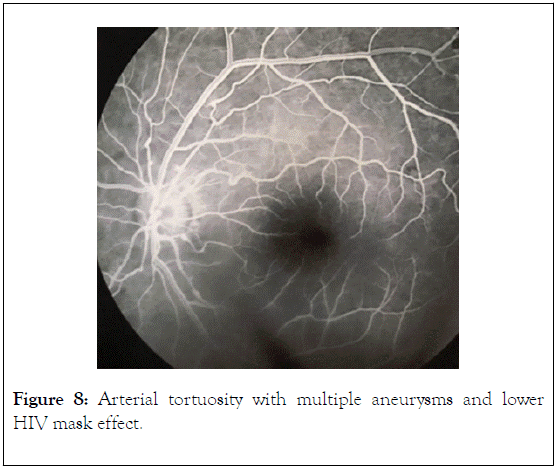
Figure 8. Arterial tortuosity with multiple aneurysms and lower HIV mask effect.
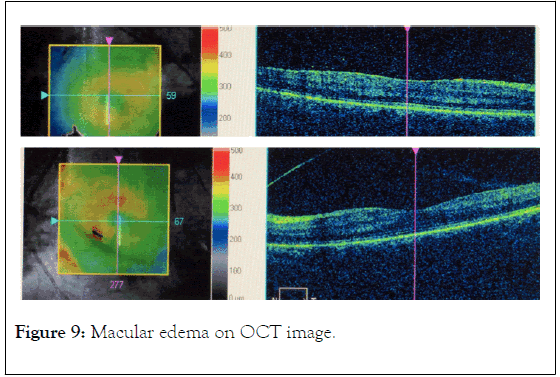
Figure 9. Macular edema on OCT image.
The biological assessment (inflammatory: sedimentation rate- CRP, infectious: blood count-serologies-quantiferon, blood smear-HB electrophoresis-Blood test-ECA-phosphocalcic and immune) did not reveal any anomaly.
Orbitocerebral angio MRI was also performed and returned to normal and Neck vessels Doppler did not show any abnormalities.
Given these result, the diagnosis retained in view of the clinical lesions found in the fundus examination, arterial aneurysmal vascular anomalies, neovascularization and complicated peripheral ischemia, age and sex of the patient, absence of history, is IRVAN Syndrome with two major criteria (arterial aneurysm and idiopathic vasculitis in a 45-year-old young woman with no history after ruling out other possible etiologies: uveitis, infectious vasculitis, inflammatory, autoimmune diseases, etc.)
After having performed the pan retinal photocoagulation in this patient, the follow-up was performed every 15 days at the beginning then progressively spacing out the duration while controlling the fundus examination every time, which was improving with regression of intravitreal hemorrhage, disappearance of spot and retrohyaloid hemorrhages and improvement of visual acuity (Figure 10).
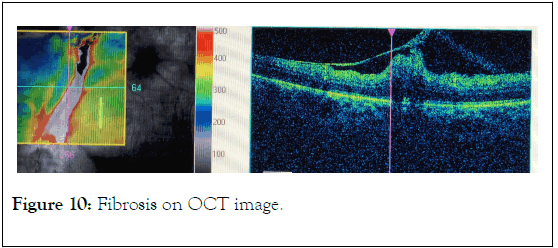
Figure 10. Fibrosis on OCT image.
As described by Chang et al. [1] and redefined by Samuel et al. who came up with the acronym IRVAN and the evolution in five stages [2] it is a rare pathology which occurs in young women without any systemic association (idiopathic) its physiopathological mechanism is not known yet. (Chawla proposes a congenital origin of aneurysms and Bailey reports a case having no aneurysms initially that still developped an IRVAN.
The clinical characteristics are divided into major criteria (retinal vasculitis, aneurysmal dilation at the bifurcations, neuroretinitis) and minor criteria (peripheral retinal ischemia, retinal neovascularization, macular exudations) [1,2] the evolution is variable, which can in some cases lead to decrease in the visual and anatomical prognosis of the eye despite the different therapeutic modalities that are reported [2-5] There is a classification that was developed to stage the progression of the disease (Table 1) [2].
| Stage ocular findings | Suggested therapy |
|---|---|
| Macroaneurysms, exudation, neuroretinitis, retinal vasculitis | High dose prednisolone, photocogulation, local steroid injections |
| Capillary nonperfusion (angiographic evidence) | High dose prednisolone, photocogulation, local steroid injections |
| Posterior segment neovascularization of disc or elswhere and/or vitreous hemorrhage | High dose prednisolone, local steroid injections, photocoagulation, anti-VEGF agents, cryotherapy |
| Anterior segment neovascularization (rubeosis iridis) | Surgery, anti- VEGF agents, cryotherapy |
| Neovascular glaucoma | Surgery and treatment of glaucoma |
Table 1: Stages of IRVAN syndrome.
Imaging makes it possible to follow up and get accurate information on the evolution [6], fluorescence angiography makes it possible to detect aneurysmal vascular anomalies, retinal neovascularizations, peripheral capillary ischemia. The OCT detects macular anomalies such as exudations and epimacular membranes [7].
There is no common therapeutic consensus to date, multiple therapeutic options have been reported: from simple observation [5,8] to pan retinal photocoagulation which is one of the most effective treatments for controlling macroanurysms and ischemia [2,17], corticosteroid therapy in the form of a dexamethasone implant to combat macular edema with a significant reduction in thickness, thus improving vision, intravitreal injection of anti VEGF [4,9,10-15], administration of the Infliximab immunomodulator to treat exudation [9,10] surgery comes last for treatment of advanced stages with vitrectomy and traditional detachment surgery or epimacular membrane peeling
Our case illustrates an incomplete case of IRVAN syndrome with no obvious exudative retinopathy, which improved significantly with PRP treatment alone given the predominance of the ischemic component.
We also observe in this case the severity of the disease which can progress silently given the visual acuity which has not been much affected despite the extensive ischemic retinal complications
IRVAN syndrome can display several forms depending on the dominant component (exudative or ischemic)
In our case, given the complicated major ischemic attack, the urgent photocoagulation treatment was sufficient to prevent complications in the anterior segment and to improve visual acuity without needing further therapeutic modalities.
Citation: Zaoui K, Tarib I, Messaoudi R, Reda K (2020) An Atypical Idiopathic Retinal Vasculitis, Aneurysms and Neuroretinitis IRVAN: Case Report. J Clin Exp Ophthal. 11:824. DOI: 10.35248/2155-9570.20.11.824
Received: 23-Jan-2020 Accepted: 07-Feb-2020 Published: 14-Feb-2020 , DOI: 10.35248/2155-9570.20.11.824
Copyright: © 2020 Zaoui K, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.