Journal of Clinical and Experimental Ophthalmology
Open Access
ISSN: 2155-9570
ISSN: 2155-9570
Case Report - (2022)Volume 13, Issue 7
Purpose: To present a patient with unilateral sub-internal limiting membrane retinal hemorrhages and a vitreous hemorrhage following COVID-19 vaccine.
Methods: Observational case report and review of literature for pathogenesis of sub-internal limiting membrane (sub ILM) hemorrhages. Detailed fundus examination, spectral-domain optical coherence tomography (Heidelberg engineering) and fluorescein angiography.
Result: On the basis of the history taking, hematochemical and instrumental examinations, we could not identify any condition or risk factor that could determine this clinical presentation.
Conclusion: Temporal correlation to the COVID-19 vaccination administered 11 days before the onset of symptoms, may suggest a potential adverse drug reaction and must be taken into account.
COVID-19; Retinal bleeding; Retinal hemorrhages; Vitreous hemorrhages; SARS-CoV-2 vaccination
The Severe Acute Respiratory Syndrome Coronavirus 2 (SARSCov- 2) was detected in late December 2019 in Wuhan and it was declared as a global pandemic disease by the World Health Organization (WHO) on March 11, 2020 [1]. Currently for different types of COVID-19 vaccines the use has been authorized despite long-term data on side effects are still unavailable. Despite some studies have reported on signs of retinal impairment such as vein dilatation, flame shaped hemorrhages, retinal vein/artery occlusion and cotton wool spots in patients with COVID-19 [2-5], no cases of retinal involvement following SARS-CoV-2 vaccination are reported in the literature to date. We report the case of a 47-year-old woman who presented with multiple unilateral sub-internal limiting membranes (sub ILM) hemorrhages few days after the injection of the adenovirus vector vaccine Vaxzevria.
On June 2021, a 47-year-old woman referred to the ophthalmology emergency room due to blurry vision, flashes and floaters in the left eye. Patient reported good general health,no history of eye disease or trauma and no episodes of coughing, vomiting, straining or weightlifting. The patient denied alcohol abuse, smoking or use of any medications except for estroprogestinic started on December 2020 and discontinued on April 2021. She received the first dose of Vaxzevria vaccine 11 days before the onset of symptoms. The best corrected visual acuity was 20/20 in the right eye and 20/50 in the left eye. Her pupillary response, ocular motility, external and anterior segment examinations and intraocular pressure were within normal limits. Dilated fundus examination revealed in the left eye complete Posterior Vitreous Detachment (PVD), four ovals intraretinal hemorrhages localized near retinal venous vessels, particularly at the level of the infer nasal branch and upper branches and a vitreous hemorrhage above the inferior temporal vascular arcade. A choroidal nevus was highlighted supersonically to the optic disc. Right eye did not show any fundus alterations and there was no evidence of neovascularization in either eye. Spectral domain optical coherence tomography (Heidelberg Engineering) showed complete PVD, four dome-shaped lesions with a hyper-reflective band and a hypo-reflective area beneath consistent with blood, confined below the Internal Limiting Membrane (ILM) and localized at the level of the previously described venous vessels.
In proximity of the inferior temporal vascular arcade scans showed a hyper-reflective granular band located on the posterior hyaloid with partial obscuration of the underlying retinal layers referable to vitreous hemorrhage. Findings from fundus fluorescein angiography showed the blocked fluorescence from the retinal and vitreous hemorrhages without vascular filling defects or hyper fluorescent lesions. No lesions were detected in retinal venous and arterial vessels. The arterial blood pressure, blood cell count, hepatic and renal function, blood sugar and inflammatory markers were within normal ranges. Assessment of blood coagulation was within normal limits except for the levels of fibrinogen which were slightly increased in a first measurement (428 mg/dl, reference interval (180-350 mg/dl) as well as D-dimer levels (4.34 mg/dl, reference value (<0.6 mg/ dl)). After one week these values were within normal limits. In addition, the patient underwent an electrocardiogram and a brain Computerized Tomography (CT) scan that showed no abnormalities Figures 1-5.
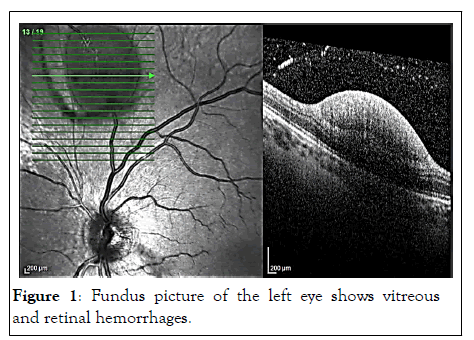
Figure 1: Fundus picture of the left eye shows vitreous and retinal hemorrhages.
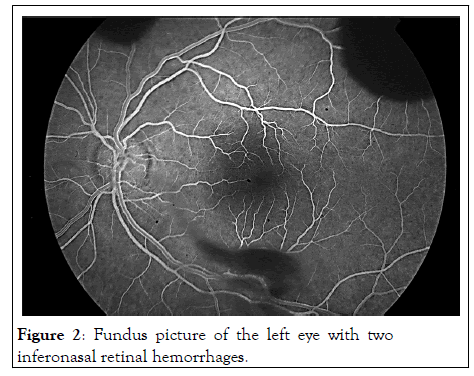
Figure 2: Fundus picture of the left eye with two inferonasal retinal hemorrhages.
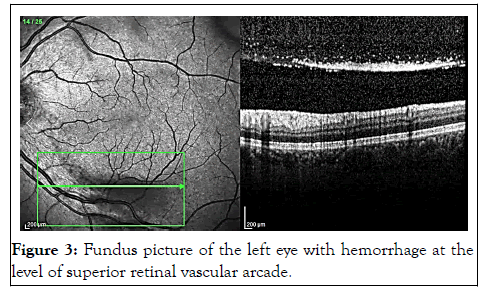
Figure 3: Fundus picture of the left eye with hemorrhage at the level of superior retinal vascular arcade.
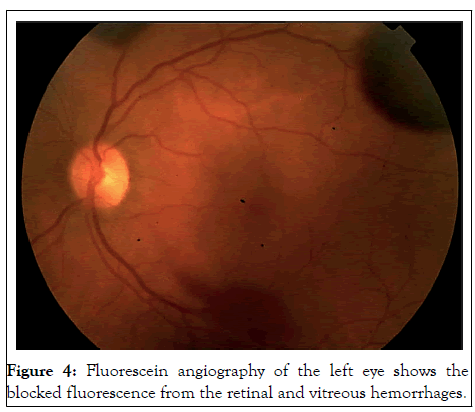
Figure 4: Fluorescein angiography of the left eye shows the blocked fluorescence from the retinal and vitreous hemorrhages.
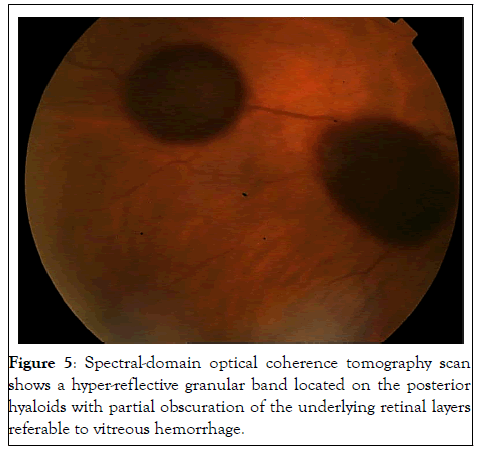
Figure 5: Spectral-domain optical coherence tomography scan shows a hyper-reflective granular band located on the posterior hyaloids with partial obscuration of the underlying retinal layers referable to vitreous hemorrhage.
Sub-ILM hemorrhages have been described in a variety of clinical settings, the most common being Valsalva retinopathy and Terson's Syndrome (TS) [6,7]. Other causes of sub‐ILM hemorrhages described in literature include blood dyspraxia, ruptured retinal macro‐aneurysms, shaken baby syndrome and blunt or penetrating ocular trauma [8-10]. In some patients, no obvious cause can be identified and the sub‐ILM hemorrhage is assumed to be idiopathic [11]. Moreover, diabetes, hypertension, anemia, leukemia, coagulopathy and head trauma can be all associated with retinal hemorrhages [12]. In some patients, no obvious cause can be identified and the sub‐ILM hemorrhage is assumed to be idiopathic [13]. Valhalla retinopathy typically presents as unilateral or bilateral sudden visual loss in an otherwise healthy individual, caused by a premacular hemorrhage secondary to a Valsalva manoeuvre [14]. The Valsalva manoeuvre causes a sharp rise of the intraocular venous pressure and ruptures of superficial retinal capillaries during activities such as coughing, vomiting, straining, or labour [15-17]. This etiology was ruled out in our patient as she denied all the above mentioned triggers. Terson’s syndrome is the presence of any intraocular hemorrhage, including vitreous, subhyaloid, intraretinal, or subretinal bleeding, in patients with subarachnoid or any intracranial hemorrhage [18]. The brain CT scan showed no sign of intracranial bleeding or any other abnormality making TS unluckily in our patient.
On the basis of the history taking, haematochemical and instrumental examinations, we could not identify any condition or risk factor that could determine this clinical presentation. Despite an idiopathic form of sub-ILM hemorrhage remains a possible conclusion; the temporal correlation to the COVID-19 vaccination administered 11 days before the onset of symptoms, may suggest a potential adverse drug reaction and must be taken into account. In support of this hypothesis, the GOV UK has reported spontaneous cases of retinal hemorrhage post-Vaxzevria COVID-19 vaccine, to date.
Consent to publish the case report was not obtained. This report does not contain any personal information that could lead to the identification of the patient.
No funding or grant support
The following authors have no financial disclosures:
• G.M.
• A.C.
• F.A.
• E.M.V
All authors attest that they meet the current ICMJE criteria for authorship
None
Citation: Mecarelli G, Calandri A, Avogaro F, Vingolo EM (2022) An Uncommon Case of Unilateral Vitreous and Sub-Internal Limiting Membrane Retinal Hemorrhages following COVID-19 Vaccine. J Cli Exp Ophthalmol. 13:937.
Received: 22-Jun-2022, Manuscript No. JCEO-22-18016; Editor assigned: 24-Jun-2022, Pre QC No. JCEO-22-18016(PQ); Reviewed: 08-Jul-2022, QC No. JCEO-22-18016; Revised: 22-Aug-2022, Manuscript No. JCEO-22-18016(R); Published: 29-Aug-2022 , DOI: 10.35248/2155-9570.22.13.937
Copyright: © 2022 Mecarelli G, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.