Journal of Clinical & Experimental Dermatology Research
Open Access
ISSN: 2155-9554
ISSN: 2155-9554
Case Report - (2019)Volume 10, Issue 3
Sensitive skin syndrome (SSS) is a prevalent skin condition reported globally in most ethnic groups which may occur in any skin location. The cause and pathogenesis of SSS is still unresolved and controversial. Albeit the head and neck region including the face and scalp are reported as the commonest sites of SSS, the lips as the only region of the face affected has been rarely reported in the literature. We report a case of a 30 years old Chinese women with a positive family history of nasopharyngeal carcinoma who reported to have significant neurological, nociceptive and pruritoceptive symptoms solely over the lips lasting for more than one year complicated by psychological and sleep disturbances after dental procedure. She was followed up and monitored by the validated 10-items Sensitive Skin Scale questionnaire (SS–10) in the clinic setting, treated and managed by topical tacrolimus ointment, emollients, counselling, education and psychological supports.
Sensitive skin syndrome over lips; Topical tacrolimus ointment; Sensitive skin scale questionnaire (SS-10); Family history; Nasopharyngeal carcinoma in Chinese
Sensitive skin syndrome (SSS) is a prevalent, chronic complex difficult to manage skin condition reported in all ethnicity [1,2]. Till now, SSS remains a clinical diagnosis without definitive reliable confirmatory tests but exclusion of other cutaneous diseases [3]. Its exact pathogenesis is still inconclusive [4,5]. Its management and therapeutic management have not difficult and not been standardized. We reported a case of a 30 years old Chinese woman who reported to have significant nociceptive and pruritoceptive symptoms solely over the lips lasting for more than one year complicated by cognitive and sleep disturbances after dental procedure.
A 30 years old lady visited our dermatology clinic on December 6, 2018 complained of severe, recurrent, sudden onset of numbness, burning, tingling, painful, itchy and tightening sensations over the upper and lower lips with swelling particularly worse during the night. The paroxysmal, sharp, knife like sensation over her lip region was severe to an extent to make her awake during sleep at night. According to her, the subjective sensations and feelings occurred only over her lip’s region. She denied these subjective sensations in other parts of the body. She could not specify any particular triggering factors. As quoted by the patient, even drinking plain water on occasions had exacerbated the distressing feelings. She also reported to experience these sensory symptoms after exposure to hot food, chilly wind, cosmetic lip balm and stress.
On November 2016, she received a dental cosmetic procedure to correct her teeth protrusions. According to the dental records, this involved application a chemical substance of 37% phosphoric acid and pull back of the dentures through applying a stainless steels material consisted of 20% chromium, 10% nickel and 70% iron. She started developing the neurological symptoms on November 2017. While she sought advices from her dentists; the dental consultation reported the symptoms were not an adverse reaction to the commonly practiced dental procedure. This was affirmed subsequently by a second opinion from another dentist. The metallic dental frame was removed after her complaints started. She visited at least five doctors including dermatologists during November 2017 to December 2018 and had been prescribed and treated with various types of topical emollients, steroids, oral painkillers and antihistamines with no avail.
Her condition worsened at end of December 2018 which was in the midst of winter of the year locally in Hong Kong. She felt desperate as the tingling and the distressing sensations over her lips significantly incapacitated her daily activities including job and social life. She woke up every night because of the paroxysmal tingling and tightening sensation of the lip during sleep.
She visited my dermatology clinic on December 6 2018. On further enquiry, she had not been diagnosed to suffer from any significant allergic skin diseases like atopic dermatitis, urticaria or psoriasis. She did not report any allergic drug history or taking any regular medication including herbal medicines. She had a history of thyroidectomy and maintained on thyroxine 100 micrograms daily started ten years ago. She had a complicated family history and is followed in the hospital internal medicine, Ear Nose and Throat (ENT) and gynecology department. There is a strong positive history of nasopharyngeal carcinoma (NPC) and hepatocellular carcinoma in the family. (Figure 1) She is closely followed up by the hospital ENT Department and Gastroenterology Department. Till now, follow up screening did not reveal any occurrence and signs of cancers.
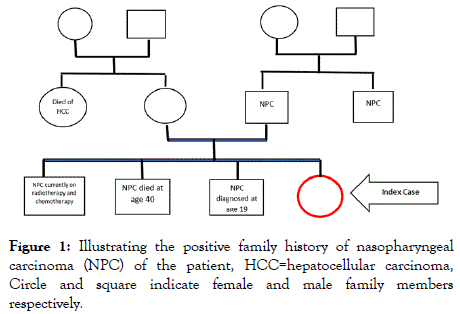
Figure 1: Illustrating the positive family history of nasopharyngeal carcinoma (NPC) of the patient, HCC=hepatocellular carcinoma, Circle and square indicate female and male family members respectively.
Good aesthetic and functional evolution was noticed in our patients, without recurrence after 18 months follow-up.
On physical examination, her lips revealed no signs of skin diseases especially there is absence of cracks, fissures, scales, blisters or swellings but she reported during acute flare, her lips may be swollen which subsided within hours. She did not complain of any difficulty in breathing, swallowing or swellings of eyelids. She had signs of erythematous, telangiectatic rosacea which she denied any symptoms apart from dry eye (Figure 2).
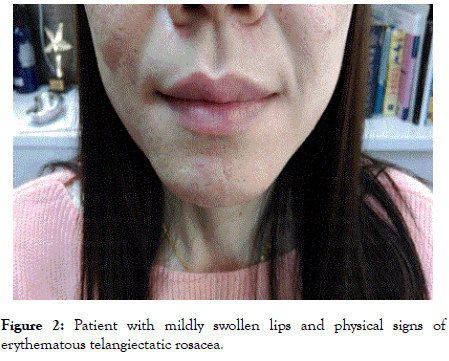
Figure 2: Patient with mildly swollen lips and physical signs of erythematous telangiectatic rosacea.
Good aesthetic and functional evolution was noticed in our patients, without recurrence after 18 months follow-up.
All up to date blood investigations including hepatitis B status, α-fetoprotein-protein, NPC tumour markers, MRI scanning and PECT scanning were all negative. Prick skin test, patch testing, anti-nuclear factor, complete blood picture, C3 and C4 were all negative. In view of the subjective atypical clinical presentation of sensory dysfunction of skin without any evident physical signs during presentation in clinical setting, a diagnosis of sensitive skin syndrome over the lips was suspected on clinical grounds. The differential clinical diagnosis at this juncture was acquired angioedema, allergic contact dermatitis of the lip, chelitis, perioral dermatitis and burning mouth syndrome. As there is no family history of angioedema, hereditary angioedema was excluded. A negative C3 and C4 ruled out acquired angioedema. Subsequent patch testing, the absences of physical signs of the lips, predominance of tingling sensation clinically made an inflammatory dermatitis unlikely. She was referred to a dental specialist for an opinion of any abnormality of the oral cavity and possible missing out of oral mucosal pathology but the report was unfruitful. No evidence of burning mouth syndrome was reported and in fact; no diagnosis can be reached by our dental colleague. A capsaicin test was performed with the patient’s consent with a gross intolerance and swelling of the affected region; i.e. the lip. Lactic acid test and skin biopsy were strongly refused by the patient after careful explanation and counseling.
In sum, a 30 years old Chinese woman who suffered from significant aberrant subjective perceptive sensations over the lips without any physical signs complicated by psychological and sleep disorders after a dental procedure was reported. A clinical diagnosis of sensitive skin syndrome over the lips was tentatively made.
The patient was counseled, fully explained and carefully monitored weekly as for the initial management of the condition. With the patient agreement, co-operation and assistance, the 10 items version of the Sensitive Scale Questionnaire (SS-10) was used to assess, monitor and manage the patient progress especially during therapeutic intervention in the clinical setting. The translated Chinese version of SS-10 was used (Figures 3a and 3b). The SS-10 is a well validated, pertinent and convenient self-reported assessment tool to monitor SSS. It was quick and easy to complete by the patients in clinic setting. It has a good correlation with Dermatology Quality of Life Index (DLQI) [6,7]. During her initial visit, the patient reported a score of 46/100 using the SS-10. The mean initial scores reported in the literature of sensitive skin was 37/100 [6]. A quality of life questionnaire was also used to assess her general health condition which revealed an unsatisfactory status of her personal health. Her main psychological complaints were emotional upsets, unhappiness, sleep disturbance and dis-satisfaction of the management of her skin condition.
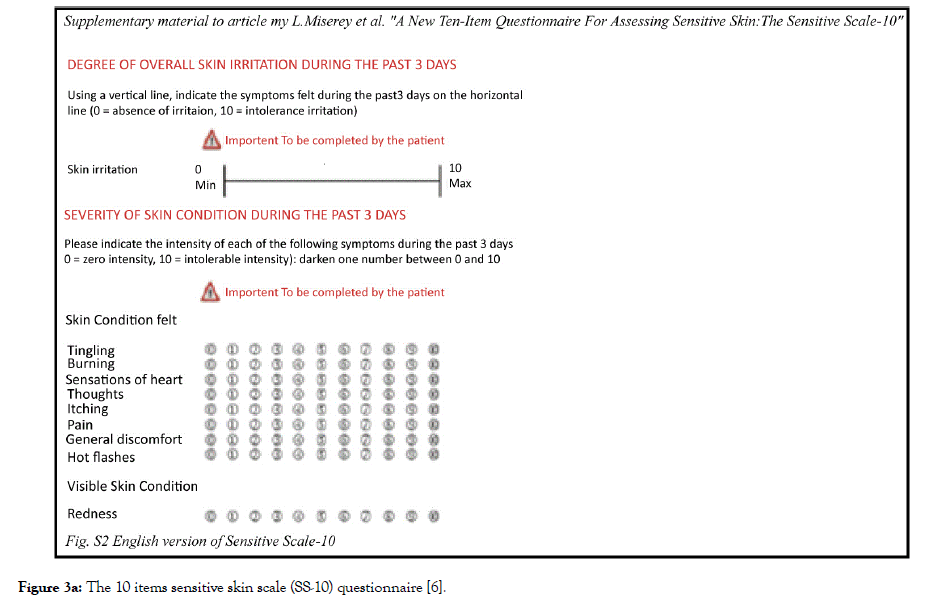
Figure 3a: The 10 items sensitive skin scale (SS-10) questionnaire [6].
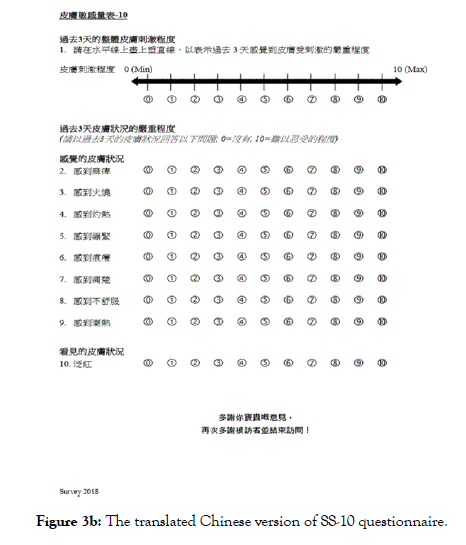
Figure 3b: The translated Chinese version of SS-10 questionnaire.
Good aesthetic and functional evolution was noticed in our patients, without recurrence after 18 months follow-up.
The patient was prescribed topical 0.03% topical tacrolimus on December 27, 2018 over the lips twice daily together with an emollient consisted of plain Vaseline. She was warned about the initial stinging sensation, pain, itchiness and possible worsening of the condition. She was instructed to avoid this down time by storing the tacrolimus ointment in a place with a low temperature and by applying a small quantity to prevent initial flare. On January 3 2019, her SS-10 was reported to be 29/100. However, on the subsequent weekly clinic follow up, a rebound of symptoms was noted and a score of 47/100 was recorded. Fortunately, with the patient’s perseverance, and continue application of the topical tacrolimus, her subsequent neurological symptoms improved as evident by a decline of the SS-10 score decreased to below 30/100 with diminution of nociceptive and pruritoceptive symptoms (Figure 4). Her quality of sleep improved. No awakening during nocturnal sleep secondary to feeling neurological discomfort was recorded. The concentration of topical tacrolimus was increased to 0.1% on February 18, 2019. She then went for a planned holidays trip to visit Egypt on March 20 2019 She reported to have a resurgence of the distressing, unpleasant neurological sensations over the lips especially during chilly night and after food. The SS-10 score during her after trip clinic visit on March 27 2019 was 48/100 and on April 3 2019 42/100 respectively. She denied of stop applying the topical tacrolimus during the holiday period. On 10 April 2019, she reported to have the symptoms improved while she increased the dosage amount of topical tacrolimus 0.1% ointment. Her SS-10 score decrease to 29/100 on 10 April 2019. She was followed up continuously in due course.
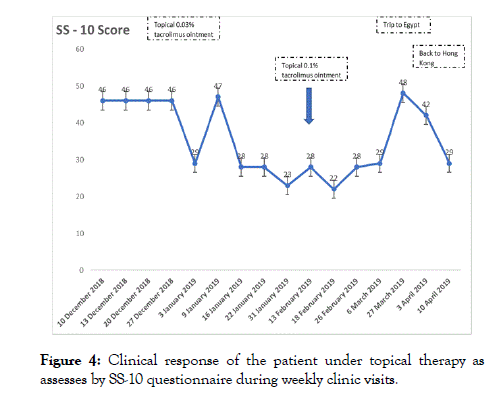
Figure 4: Clinical response of the patient under topical therapy as assesses by SS-10 questionnaire during weekly clinic visits.
Good aesthetic and functional evolution was noticed in our patients, without recurrence after 18 months follow-up.
SSS is a complex neurological skin condition which has been reported on almost every anatomical site of the skin except solely over the lips. Most notable location of sensitive skin is the face and scalp but can happen in any parts of the skin of the body includes hands, scalp, arms, genital areas, perianal region, scrotum and the trunk [8-10]. 70% reported extra facial presentations; hands (58%), scalp (36%), feet (34%), neck (27%), torso (23%), back (21%) [1,8,9]. As previously reported, the most sensitive subregions of the face are nasolabial fold, followed by the malar eminence, chin, forehead and the least upper lip based on sensitive provocation test [10,11]. The regional difference is suggested to be due to the variations in degree of innervation and abundance of blood supply. Thus, the lips should be the least likely sensitive and mere sensitive lips with pronounced neurological symptoms without affecting the face or other parts of the face are unusual. Our case is the first reported SSS occurred on the patient’s lips region only uninvolved other parts of the face and body. Although SSS happened in the genital region was not infrequent, SSS solely affecting the lips are rare. The epidermis and thin stratum corneum of the genitalia resemble the lip epidermis. The thin epidermis made up of only a few layers of stratum corneum over the lip, oral, genitalia and anal mucosae may have increased the possibility of occurrence of SSS in patients who are genetically or innately susceptible to this distressing miserable skin condition.
SSS is a syndrome defined by the occurrence of unpleasant sensations (stinging, burning, pain, pruritus, and tingling sensations) in response to stimuli that normally should not provoke such sensations [12]. These unpleasant sensations cannot be explained by lesions attributable to any skin disease. The skin can appear normal or be accompanied by erythema or swelling [12]. As discussed, sensitive skin can affect all body locations especially the face and scalp. Although the lip has been reported to be the least sensitive area of the face; its function as the first defensive barrier to foreign invasions including noxious chemicals, foods, pH, acidity, pathogens and trauma. The unique function and anatomy of the lip aggravated the distressing symptoms of SSS especially in a social setting which aesthetically further perplexed and complicated the patient emotion and psychology. The ontological evolutionary tucking in of the superficial skin of the face to the inner gut interposed through the lip may suggest the shared functional, morphological and pathological similarity between the two distinct but related systems of the body. Recently, SSS has been postulated to be associated with gut irritability like irritable bowel syndrome [13]. In short, clinical symptoms and neurological pathology of the lips may be translated and integrated to cognitive, psychological and emotional domains of our gut and brain; in turn viciously affect our behaviour, social and quality of life.
Currently, no definitive diagnostic test exists for the confirmation of SSS. The predominance of neurological symptoms of our reported case with clinical and laboratory exclusions of other possible differential diagnosis like angioedema, contact dermatitis, chelitis and perioral dermatitis lead us the clinical diagnosis our patient suffered from SSS over the lips. The conservative control of the neurological symptoms by transient receptor potential receptor modulator (TRPV); tacrolimus provides additional support that the underlying pathology of this case is mediated neurologically through TRP channelopathy [14-18]. Currently, there is no strong medical evidence; double blinded study; to investigate the effectiveness of topical tacrolimus ointment or equivalents in the effective treatment of the skin condition. Isolated case report using topical pimecrolimus cream in treating effectively SSS has been documented possibly by down regulating the TRPV receptors [19]. Topical tacrolimus especially ointment may also improve the overall skin thickness of the epidermis which have been reported to be one of the causative aetiologies of SSS [20]. The ointment if well tolerated may also prevent transwater epidermal loss (TWEL) which pathologically associated with SSS [20]. Liberal applications of plain emollients are also sensible therapeutic measures to reduce TWEL and increase epidermal thickness. Other treatments documented in the literatures like TRPV 1 antagonist 4-tbutylcyclohexanol and licochalcone, low level energy device like laser and intense pulse light, cosmetic products and ingestion of probiotics may not be applicable due to the inaccessibility and inapplicability of these therapeutic measures in our specific case [21-24]. The DLQI on the last clinic visit on 10 April 2019 showed a patient self-reported improvement of health, emotion, anxiety and happiness status. This is in agreement with the improved SS-10 assessment score. The willingness of the patient to return for repeat follow up in a weekly basis also reflected a strengthened doctor-patient relationship and rapport.
The SS-10 questionnaires has fulfilled and served as a very useful, effective, convenient and patient friendly assessment tool in the management of SSS. By definition, SSS is essentially a subjective neurosensory dysfunctional skin condition. A selfreported questionnaire is a cost-effective and harmless management tool compared with other chemical or invasive diagnostic procedures. Non-invasive imaging and neurophysiological test hopefully may be developed in the future in the diagnosis of SSS. SS-10 in our case has been used as a continuous assessment method not only to the therapeutic response of the treatment but also any changes of the life or social circumstances of the patients which may negatively affecting the patient suffered from SSS. This is evident in our case; our patient reported a high SS-10 score with relapse of SSS during an exotic holiday trip in Egypt where extreme climatic conditions and environments prevail. This information is pivotal in managing SSS patients especially during education, counseling and prevention in a skin condition like SSS which exact clinical status, pathogenesis, course and management is still undefined.
Finally, it is interesting to note that there are two significant salient features of our patient’s history; signs of rosacea and a strong positive history of nasopharyngeal carcinoma. Rosacea has been reported to have a possible association with SSS and in fact, most neurological symptoms of rosacea like burning, stinging, pruritus and erythema of skin coincided with SSS. TRPV aberrancy has also been hypothesized to be one of the molecular pathophysiological mechanism of rosacea; hence; TRPV down regulator like topical tacrolimus has also been recommended in rosacea. Nevertheless, rosacea has not been reported to have neurological symptoms over the lips and the clinical variant of rosacea; perioral dermatitis is predominantly characterized by grouped, erythematous papules, papulovesicles, or papulopustules in a predominantly perioral distribution which is absent in our case. The relationship between rosacea and SSS worth further observation and investigation. SSS has never been reported as a paraneoplastic condition. Our patient has been under strict scrutiny for development of NPC in view of the strong family history and southern Chinese ethnic background. Whether, genetic predisposition, dietary practices and body immunity play a role in SSS like NPC still remain speculative but worth following up.
In conclusion, a case of a 30 years old Chinese lady with a positive family history of NPC and rosacea suffered from SSS only over the lip region after a dental procedure was reported. She was conservatively and effectively controlled with topical tacrolimus and emollients. Careful counseling and timely followed up are mandatory as the prognosis of her skin condition is unknown. This is the first and only case documented in the medical literature of a female patient suffered from SSS solely on the lips controlled with topical tacrolimus ointment, emollients, counseling, explanation and education on prevention.
Citation: Chan KTM (2019) An Unusual Presentation of Sensitive Skin Syndrome over the Lips of a Female Chinese Patient after Dental Procedure Managed and Improved with 0.03% and 0.1% Topical Tacrolimus Ointment Application as Assessed by the SS-10 Questionnaire. J Clin Exp Dermatol Res. 10:496. doi: 10.35248/2155-9554.10.496
Received: 15-Apr-2019 Accepted: 19-Apr-2019 Published: 26-Apr-2019 , DOI: 10.35248/2155-9554.10.496
Copyright: © 2019 Chan KTM. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.