Journal of Fertilization: In Vitro - IVF-Worldwide, Reproductive Medicine, Genetics & Stem Cell Biol
Open Access
ISSN: 2375-4508
ISSN: 2375-4508
Mini Review - (2023)Volume 11, Issue 1
Delayed Puberty (DP) is practically correlated with the presence of either Constitutional Delay of Growth of Puberty (CDGP), or Congenital Hypogonadotropic Hypogonadism (CHH). Although lots of so called “red flags” are associated with CHH frequently, they usually get sidelined by most physicians. Hence assessment of various markers like Insulin like peptide 3 (INSL3) as well as Inhibin B (INB) has been done in the form of probable markers regarding discrimination of CDGP along with CHH respectively, either in basal state or subsequent to Gonadotropin Releasing Hormone a (GnRHa) stimulation. Insulin like peptide 3(INSL3) represents a product that gets liberated by Leydig cells along with is getting considered in the form of probable marker regarding discrimination of CDGP along with CHH besides the commonly used INB. It is significant to differentiate the 2 conditions as CDGP is correlated with remarkable psychosocial influence on those impacted along with their families besides inspite of tell-tale signs, clinicians fail to diagnose CHH till 18-19 years when changes become irreversible despite treatment fully possible the earlier diagnosis is made with signs of cryptorchidism or microphallus and treatment initiated early. Thus here we have tried to highlight the findings of Abbara, et al, in use of INSL3 as a biomarker in younger boys whereas in adults INB might be the ideal marker in adults. Furthermore, the role of genetic, epigenetic along with environmental factors might control the timing of puberty is getting emphasized in recent studies. Thus for optimization of fertility potential of CHH men with judicious diagnosis and treatment it is significant to increase awareness of physicians to refer a child early when seen with non-descent of testis at birth.
Delayed Puberty (DP); Constitutional Delay of Growth of Puberty (CDGP); Congenital Hypogonadotropic Hypogonadism (CHH); Insulin like peptide 3(INSL3)
Earlier we had reviewed the various roles of kisspeptins, prokineticins in human reproduction, and then comprehensively reviewed various cause of Idiopathic Hypogonadotropic Hypogonadism (IHH), inclusive of Congenital Hypogonadotropic Hypogonadism (CHH), various genetic etiologies beside show to do Differential Diagnosis (DD) of Constitutional Delay of Growth of Puberty (CDGP) from CHH [1-6], however till date this controversy has kept persisting. Puberty involves a complicated physical along with psychological process which ends in development of reproductive capacity. Pubertal conditions are frequent along with correlated with remarkable psychosocial influence on those impacted along with their families [7]. Delayed Puberty (DP) is defined as the absence of enlargement of testis in boys to attain a volume of >4 ml at an age which is 2-2.5 SD later than their population mean. Although in Europe it is the age 13 years in girls and 14 years in boys has been decided to be the guideline for the need for further examination [8].
Maximum percentage of boys (95%) presenting with Delayed Puberty (DP) would be possessing the imprecise quantities of gonadotropins (that is normal or lower regarding sex steroids quantities basically in view of total or transitory gonadotropins deficiency) [9]. Out of these the maximum of very young adolescents (60%-80%) would possess Constitutional Delay of Growth of Puberty (CDGP) along with spontaneously experience puberty, however at a time later than their counterparts [10,11]. Nevertheless, approximately 10% of young adolescents whose presentation is DP would be possessing Congenital Hypogonadotropic Hypogonadism (CHH), an incidence which probably escalates to 90% by the time they reach 18-20 years [12]. CHH represents a genetic trait, accounting for dysfunctional or hypothalamic Gonadotropin Releasing Hormone (GnRH) neuronal migration resulting in absence/deficiency of GnRH neurons or their working secondary to aberrant GnRH liberation/effect of GnRH or both [13]. Another 10%-15% possess functional etiological factors of Hypogonadotropic Hypogonadism (HH), which are accounted by acute or chronic illnesses, inadequate bioavailability of energy or inimical effects of medicines like glucocorticoids [9].
The differentiation of CDGP from CHH is a big diagnostic hurdle in boys with DP, in particular in view of overlap amongst clinical presentation in addition to akin hormonal patterns [14]. Despite, so much work in this field, notoriously the postponement of efficacious treatment of CHH takes place as late as 18-19 years, in view of usually treating clinicians find it tough to make the differential diagnosis from CDGP. The precise along with differentiation at a proper time is markedly significant. Earlier we highlighted how to utilize minipuberty for early diagnosis of CHH [5]. The reason it is so significant to differentiate the 2 conditions are correct counselling as well as conservative treatment or sex steroids therapy regarding psychosocial stress in CDGP vis a vis more emphasis on GnRH pump/gonadotropin therapy in case of CHH with regards to taking care of sexual function, bone in addition to metabolic as well as psychosocial health [3,4,15]. Despite, maximum of CHH males possess distinct phenotypic tell tale signs (like synkinesia (KAL1), dental agenesis (Fibroblast Growth Factor 8/Fibroblast Growth Factor Receptor 1), digital bony abnormalities (FGF8/ FGFR1) and hearing loss (Chromodomain helicase DNA) and these can be useful to prioritize genetic screening although renal agenesis and cleft lip and palate did not emerge as statistically significant predictors [16] anosmia, cryptorchidism, deafness, cleft palate, or other generational aberrations [17].
Leydig along with sertoli cells markers like Insulin like peptide 3 (INSL3) as well as Inhibin B (INB) assessment has been done in the form of probable markers regarding discrimination of CDGP along with CHH respectively. INB represents a member of Transforming Growth Factor beta (TGF-β) superfamily. INB is a heterodimer glycoprotein which is constituted of an Inhibin alpha subunit along with Inhibin beta subunit, that gets liberated besides is a pointer to the quantities of functional sertoli cells [18]. The peak of INB is attained transitorily at the time of mini puberty at approximately 2-4 months subsequent to birth followed by reduction till time of childhood prior to puberty along with re escalation at the time of puberty [19]. In case of male this might be realized by 9 years itself, hence occurring prior to determinable Luteinizing Hormone (LH) surge [20]. Regarding prepubertal boys INB represent basically sertoli cells mass in addition to function, whereas in case of adults it is the germ cells which dictate the alpha subunit as well as INB generation. As sequelae in case of adults INB intricately points to testicular mass inclusive of germ cells along with sertoli cells, along with hence the spermatogic capacity. This might be decreased in case of men having CHH. INB is a negative controller of Follicle Stimulating Hormone (FSH) liberation from the anterior pituitary gland like the quantities of INB are inversely associated with FSH quantities in case of adult men [18]. Maximum studies have concentrated till date on the probability of utilization of INB regarding discrimination of CDGP along with CHH, whereas occasional studies have carried out assessment of INSL3 [21]. INB reflects being a marker of mature sertoli cells [22], whereas INSL3 is a pointer of numbers, extentas well as Leydig cell differentiation [23]. INSL3 has been illustrated to depict age based dynamics from the birth to adulthood [24]. In the earlier transabdominal testicular descent fetal INSL3 possesses a key part [25]. Significantly greater quantities of INSL3 were observed that in case of serum from boys aged 3 months in contrast to older prepubertal boys that pointed to it transitorily peaking at the time of minipuberty [24]. This escalating quantities of INSL3 gets reinitiated at the time of puberty [26], along with persistence of its escalated quantities right through adult period prior to its reduction with age [27]. This Leydig cell hormone crosstalk with particular receptors, labelled as RXFP2, on Leydig cells themselves for modulation of steroidogenesis, besides on male germ cells, possibly to synergize with androgen-based sertoli cell products to aid spermatogenesis. Apart from testosterone, INSL3 is not acutely controlled by the HPG axis, but is a constitutive product of Leydig cells, which points to their number and/or differentiation status and their capability thus to generate different factors inclusive of steroids, together this is known as Leydig cell functional ability. Pathological conditions impacting Hypothalamic-Pituitary- Gonadal (HPG) axis inclusive of CHH along with primary testicular conditions like Klinefelters syndrome, cryptorchidism, along with anorchidism are correlated with lesser quantities of INSL3 [28]. Converse to T, INSL3 does not undergo incidental oscillations that is incorporated in the feedback loop of H-P-G axis [29], hence INSL3 is becoming a upcoming biomarker of conditions impacting the male H-P-G axis (Figures 1 and 2).
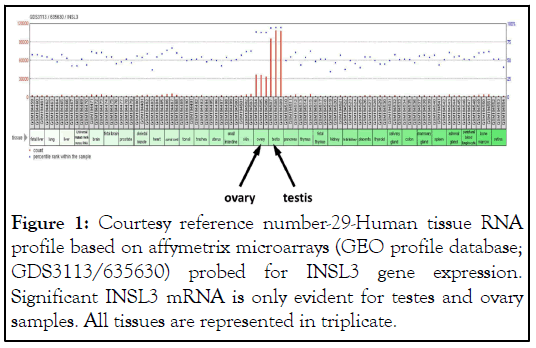
Figure 1: Courtesy reference number-29-Human tissue RNA profile based on affymetrix microarrays (GEO profile database; GDS3113/635630) probed for INSL3 gene expression. Significant INSL3 mRNA is only evident for testes and ovary samples. All tissues are represented in triplicate.
Figure 2: Courtesy reference number-29-INSL3 and HPG axis. Scheme to show the relationship between the INSL3/RXFP2 system and testosterone as endpoint effectors of the HPG axis within the testis. Arrows are directed only to cells where there are known to be specific cognate receptors.
Hence Abbar, et al., [30] conducted a retrospective cohort study inclusive of 60 boys with CDGP along with CHH in addition to 44 adult men, eugonadal or had prior CHH in whom INSL3, INB, Testosterone (T), along with gonadotropins were determined. Cohort 1 was constituted by boys with DP who were 13-17 years (51 with CDGP along with 9 with CHH) who were given GnRHa stimulation (subcutaneous triptorelin 100 mcg)) documented earlier in the context INB. Cohort 2 was constituted adult cohort of 44 men (22 eugonadal men as well as 22 CHH men) documented earlier in the context of gonadotropin reaction to kisspeptin 54 (Kp 54). The observation of Abbara A, et al. [30], were greater quantities of median INSL3 were seen in CDGP in contrast to CHH (0.35 vis a vis 0.15 ng/ml; p=0.0002). Akin to that, in case of adult men, median INSL3 were greater in eugonadal men in contrast to CHH) (1.08 vis a vis 0.05 ng/ml; p<0.0001). Nevertheless, INSL3 was more precise in distinguishing CHH in case of adult men in contrast to boys with DP (auROC with 95% CI: In adult men 100%, 100-boys with DP 86.7%:77%-95.7%). Median INSL3 was greater in boys with CDGP in contrast to CHH (182 vis a vis 59 pg/ml; p<0.0001). Akin to that, in case of adult men, median INSL3 were greater in eugonadal men in contrast to CHH) (170 vis a vis 36.5 pg/ml; p<0.0001). The performance of INB was observed to be advantageous in contrast to INSL3 in discrimination of CHH from boys with DP (AUROC with 98.5%:95.9%-100%) in contrast to adult men (AUROC 93.9%: 87.2%-100%).Thus reaching to conclusions that INSL3 is more advantageous in identification of CHH in case of adult men, whereas INB was more advantageous in identification of CHH in case of boys with DP (Figures 3 and 4) [30].
Figure 3: Courtesy reference number-30-(A) Relationship between INSL3 (ng/ml) levels over stimulated LH (IU/L) at 24 hours after GnRHa in boys with CDGP (blue circles) and boys with CHH (red triangles). Simple linear regression r2=0.26; p=0.0001 in CDGP (blue dotted line); r2=0.005; p=0.86 in CHH (red solid line). (B) Relationship between INSL3 (ng/ml) levels over stimulated testosterone (nmol/L) at 24 hours after GnRHa in boys with CDGP (blue circles) and boys with CHH (red triangles). Simple linear regression r2=0.60; p<0.0001 in CDGP (blue dotted line); r2=0.01; p=0.79 in CHH (red solid line). (C) Relationship between INSL3 (ng/ml) levels over basal FSH (IU/L) in eugonadal men (blue circles) and men with CHH (red triangles). Simple linear regression r2=0.24; p=0.02 in eugonadal men (blue dotted line); r2=0.15; p=0.10 in CHH (red solid line). (D) Relationship between INSL3 (ng/ml) levels over stimulated testosterone (nmol/L) at 4 hours after GnRH in eugonadal men (blue circles) and men with CHH (red triangles). Simple linear regression r2=0.22; p=0.03 in eugonadal men (blue dotted line); r2=0.09; p=0.19 in CHH (red solid line).
Figure 4: Courtesy reference nuber-30-(A) Relationship between INB (pg/ml) levels over basal LH (IU/L) in eugonadal men (blue circles) and men with CHH (red triangles). Simple linear regression r2=0.003; p=0.82 in eugonadal men (blue dotted line); r2=0.31; p=0.007 in men with CHH (red solid line). (B) Relationship between INB (pg/ml) levels over basal FSH (IU/L) in eugonadal men (blue circles) and men with CHH (red triangles). Simple linear regression r2=0.08; p=0.22 in eugonadal men (blue dotted line); r2=0.21; p=0.03 in men with CHH (red solid line). (C) Relationship between INB (pg/ ml) levels over stimulated LH (IU/L) 4 hours after GnRH in eugonadal men (blue circles) and men with CHH (red triangles). Simple linear regression r2=0.29; p=0.01 in eugonadal men (blue dotted line); r2=0.04; p=0.37 in men with CHH (red solid line). (D) Relationship between INB (pg/ ml) levels over stimulated FSH (IU/L) 24 hours after GnRHa in boys with CDGP (blue circles) and boys with CHH (red triangles). Simple linear regression r2=0.21; p=0.0007 in boys with CDGP (blue dotted line); r2=0.53; p=0.03 in boys with CHH (red solid line).
Furthermore, Giovaneli and Quinton in their appreciation of work of Harrington and Palmert MR, pointed that emphasis needs to be laid over Bayesian perspective, whose lesser utilization is usually attempted in biosciences, thus the total chances of observation be true or wrong gets hampered by the inimical sequelae of a false positives along with false negatives. Thus in case of teenagers the inimical sequelae of a false negative diagnosis of (of CDGP) could be there for over 10-20 years, while in case of CDGP one can not anticipate any purpose coming out from a false positive diagnosis of CHH resulting in treatment that is anyhow going to be postponed over some months/years [31].
Moreover, recent outcomes have pointed to a central part of the epigenome that in the controlling of genes present in the hypothalamus along with pituitary which might modulate how flexible is the timing of the puberty. Identifying the epigenetic controlled genes like Makorin Ring Finger 3 (MKRN3) along with Delta-like 1 homologue (DLK1) respectively that are implicated in the suppression along with activation of Pubertal generation gives further proof regarding how epigenetic differences impact timing of the puberty. Thus this is another variable needing to be accounted for in DP like DLK1 as emphasized by Faienza, et al.[32].
To summarize when a teenager/adolescent is seen by a physician who apparently has not attained puberty one has to ensure that correct discrimination is made amongst CDGP from CHH. The importance lies in not delaying the diagnosis of CHH with not much problem arising if CDGP not accurately diagnosed, but in case of CHH it might be considerably inimical from point of future fertility for the boy. Even from point of avoidance of CHH boys diagnosis getting postponed till adolescent stage one needs to pay attention in any boy having presence of micropenis and/or cryptorchidism at birth one needs to try to associate the so called red flags pointing to the particular gene deficiency along with try all possible therapies in such boys not showing evidence of minipuberty, a time when males reproductive tract formation takes place in addition to activation of GnRH axis besides rapid escalation of Testosterone (T), along with gonadotropins to again be suppressed. As outlined earlier INSL3 escalate in boys aged 3 months at mini puberty representing Leydig cells markers whereas earlier INB, a representative of sertoli cells markers was used for DD of CDGP from CHH. Now it becomes more apparent that CHH diagnosis gets delayed as late as 18-19 years so if see a boy in teenage/adolescent stage INSL3 is more appropriate for diagnosis in addition to initiation of gonadotropins/sex hormones as per age of diagnosis with it being very significant to diagnose boys with non-descent of testis as early as possible by mini puberty stage. In view of pulsatile GnRH liberation in the neonatal period seems to be of importance for the generation of male genitalia, with a long reaching effect on male reproductive phenotype along with fertility potential in adult life. Administration of recombinant Follicle Stimulating Hormone before the HCG gets introduced to avoid premature maturation of depleted pool of sertoli cells under the action of intratesticular T is important. Moreover if FSH monotherapy is used in children as well as adolescents, it aids in CHH boys gaining testicular volume besides better INB quantities.
Citation: Kaur KK, Allahbadia GNK, Singh M (2023) An Update on Factors that Enhance the Chances of Discrimination on Constitutional Delay of Growth and Puberty from Congenital Hypogonadotropic Hypogonadism: Emphasis on Role of INSL3. J Fertil In vitro IVF World w Reprod Med Genet Stem Cell Biol.11:288.
Received: 26-Dec-2022, Manuscript No. JFIV-23-21429; Editor assigned: 29-Dec-2022, Pre QC No. JFIV-23-21429 (PQ); Reviewed: 12-Jan-2023, QC No. JFIV-23-21429; Revised: 19-Jan-2023, Manuscript No. JFIV-23-21429 (R); Published: 27-Jan-2023 , DOI: 10.35248/2375-4508.23.11.288
Copyright: © 2023 Kaur KK, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.