Journal of Antivirals & Antiretrovirals
Open Access
ISSN: 1948-5964
ISSN: 1948-5964
Review Article - (2021)Volume 13, Issue 1
To-date humans suffered from a different pandemic disease which causes great loss. At the end of 2019, a few cases of high contagious flu were reported in the Wuhan, China. The death ratio is very high. Some common high-risk patients are cardiovascular disease patients, cancer patients, pregnant women, and foetuses. Ultra-Care is necessary for those pregnant women who are admitted for caesarean section surgery. Society of Obstetric Anesthesia and Perinatology revealed that in elective caesarean surgery the pregnant women should be a screen for the symptoms of COVID-19 before the procedure. During surgery along with other management, anaesthetic drugs are a key priority element. Among pregnant women, the safest anesthesia for caesarean with COVID-19 is Combine Spinal Epidural Anesthesia (CSEA). In emergency, caesarean surgery of COVID-19 patient general anesthesia with rapid sequence induction and the endotracheal tube is administered. It is recommended that pregnant women should be properly examined for symptoms of COVID-19 before surgery. The healthcare staff should wear proper PPE to avoid the spread of the virus. It is concluded that patient with other disease has increased the morbidity rate up to three-fold. The spinal and epidural anesthesia are safe for elective surgery of pregnant women.
SARS-CoV-2; COVID-19; Caesarean delivery; Anesthesia; Parturient
Human being comes across with various pandemics throughout the history where some of them were more catastrophe than other. Human suffering from a very tough time once again fighting with an invisible enemy; the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) [1]. Initially, COVID-19 was observed in Wuhan, Hubei Province, China after a few weeks of infection spread throughout China and elsewhere in the world and become worldwide public health concern [2]. In humans, mammals and birds enveloped RNA viruses are responsible for respiratory, hepatic, enteric, and neurological diseases [3]. Among six coronavirus species, two pathogens severe acute respiratory syndrome (SARS) and the Middle East Respiratory Syndrome (MERS) can develop fatal respiratory diseases in humans [4]. In 2002 and 2003 SARS-CoV was a causal agent responsible for severe acute respiratory syndrome outbreak in Guangdong Province, China [5,6]. In the Middle East 2012, MERS-CoV was the causal agent responsible for severe respiratory disease outbreak [7]. At 11th February 2020 World Health Organization, (WHO) named (Covid-19), the disease caused by the virus because it does not refer to a geographical location, animal, person, or group of people [8].
Etiology
Bats have been recognized as a major natural source of viruses. In 2002, SARS a coronavirus that transmits from bats to civets, then to humans. Scientists identified coronavirus in pangolins which have 96% genetic match to SARS-CoV-2 [9]. Previous studies revealed that this virus shares a very high percentage of genome sequences resemble with bat derived 2002 SARS Coronaviruses [10]. At 11th February 2020, International Committee of Taxonomy of Viruses, on basis of taxonomy and phylogeny Coronavirus Group was officially categorized it as severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) [11].
Epidemiology
In late December 2019, a cluster of pneumonia cases of unknown origin was reported in Wuhan China. On 31st December 2020, the Chinese Centre for Disease Control and Prevention (China CDC) respond to alert issued by Wuhan Municipal Health Commission and a notification was sent to the World Health Organization [12]. In late January 2020, WHO reported over 10,000 of cases infected with (COVID-19) across China. For the clinical confirmation of infection, the National Health Commission of China recommends a chest CT scan in its diagnosis and treatment (fifth trial version) [13]. As of June 3, 2020, a total of 6,368,272 confirmed cases were reported all over the world along with 3,803,83 deaths. Total confirmed cases, death, and recovered are shown in Figure 1.
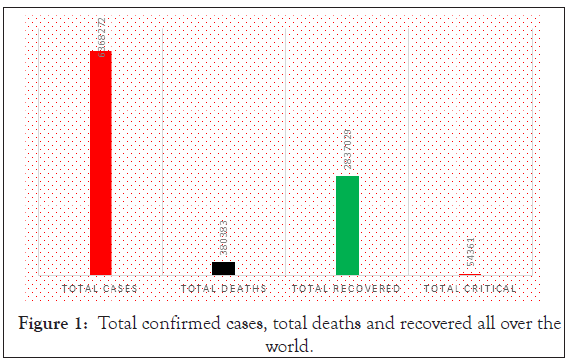
Figure 1: Total confirmed cases, total deaths and recovered all over the world.
Mortality rate
On Wednesday, January 2020 World Health Organization estimated the mortality rate of COVID-19 about 2% in a press conference and again on 10 February 2020. However, on their 29th January report WHO specified that we don't know how many infected and provisional estimates that might have changed were. On 3rd March 2020 WHO Director-General Dr. Tedros Adhanom Ghebreyesus said in his inaugural remarks at the COVID-19 that there is a 3.4% mortality rate globally. In comparison with seasonal influenza, the case fatality rate is fewer than 1% [14,15]. The fatality rate of Severe Acute Respiratory Syndrome (SARS) was round about 10% in the 2002 outbreak. While with the Middle East Respiratory Syndrome (MERS) about 34% fatality rate [16]. On 04th February 2020 National Health Commission publishes the following figures [15].
The mortality rate was 4% in Wuhan, City.
The mortality rate was 2.1% nationwide.
The fatality rate in Hubei province was 3.1%.
0.16% fatality rate in other provinces of China.
Casualties of Hubei province account for 97% of all total death in China.
Geriatric patients are more prone to illness regardless of whether they have a coronavirus or not [17]. Patients who are suffering from cardiac disease, Diabetes Melilites (DM), or high blood pressure treated with ACE-2 increasing drugs are more susceptible to serious COVID-19 infection [18,19]. A comparison of the COVID-19 mortality rate with other viruses is shown in Table 1.
| Serial. No | Virus | Mortality rate |
|---|---|---|
| 1 | Swine Flu | 0.02% |
| 2 | SARS-COV-2 | 2% |
| 3 | SARS | 9.60% |
| 4 | MERS | 34% |
Table 1: Mortality rate of COVID-19 compared with other viruses [19].
Susceptible population for COVID-19 (cancer patients, cardiac Patients, and obstetric patients)
Cancer patients consequences: A report published by the American Association of Cancer Research, a research team from China, the united states, and Singapore those cancer patients infected with COVID-19 were more likely to develop respiratory failure or spend more time in the intensive care unit (ICU) [20]. China reported that among cancer patients about 1% had COVID-19 infection. And about 40% of COVID-19 had pre-existing cardiovascular diseases who were hospitalized with pneumonia [21]. From 01 January 2020 to 24th February 2020 fourteen hospitals provided data of 641 patients for Randomized Control Trials (RCT) [22]. Patients were categorized in; patients with cancer and COVID-19 (n=105) and patients without cancer who had COVID-19 (n=536) with mean ages of 63.5 and 64.0 years respectively. Patients with cancer get on worse compared to patients without cancer in in- hospital infection. The death rate among the general population with COVID-19 is relatively 2% to 3%, patients with cancer and COVID-19 have 3 fold increase in death rate but also a higher chance to get serious complications ( prolong hospital stay, ICU admission) [20]. Those cancer patients receiving chemotherapy are more vulnerable to COVID-19 infection. It is recommended that cancer patients who are on chemotherapy should have rigorous screening for COVID-19 [23]. Different cancer types among COVID-19 are shown in Figure 2.
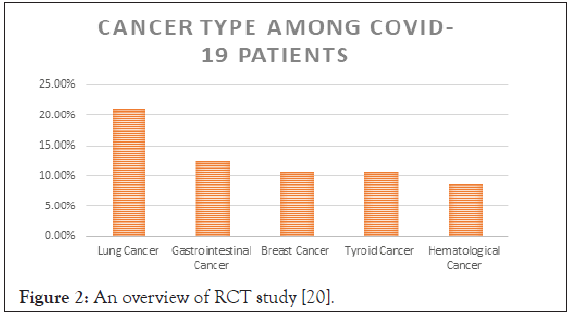
Figure 2: An overview of RCT study [20].
Cardiovascular patient’s consequences: According to the Center for Diseases Control and Prevention (CDC) people with 65 years or older having a serious cardiac problem is more vulnerable to severe illness from COVID-19 [24]. American College of Cardiology (ACC) stated that viral respiratory infection has a great impact on a patient with cardiac issues especially in light of coronavirus [25]. Data collected from 211 hospitalized patients with COVID-19. After excluding closed 67 cases and 47 patients who died in this study duration. Of 187 participants, 66 patients (35.3%) are suffering from CVD including coronary heart diseases, hypertension, and cardiomyopathy. In TnT elevated patients 52 patients (27.8%) exhibited by myocardial injury. The mortality rate was high in patients with elevated TnT level 31(59.6%) compared with normal TnT patients 12(9.9%) [26]. Clinical characteristics of patients with COVID-19 are shown in Table 2.
| Characteristic | Total patients | Normal TnT level | Elevated TnT level |
|---|---|---|---|
| No of Patients | 187 | 135 | 52 |
| Age (Mean) | 58.5 | 53.53 | 71.4 |
| Comorbidities | |||
| Hypertension | 61(32.6%) | 28 (20.7%) | 33 (63.5%) |
| CHD | 21(11.2) | 4(3.0) | 17(32.7) |
| Cardiomyopathy | 8(4.3) | 0(0) | 4(77) |
Table 2: Demographic and clinical characteristics of COVID-19 patients [2,26].
Data on SARS and MERS are spare in pregnancy. In COVID-19 pandemic pregnant women and foetuses are at high risk. During pregnancy mechanical and physiological changes increase susceptibility to infection. Especially when cardiorespiratory physiology is affected [27]. Complications related to COVID-19 include sepsis, Disseminated Intravascular Coagulation (DIC), acute respiratory distress syndrome (ARDs), and renal failure. There is no evidence of uteroplacental transmission in both (SARS) and (MERS) [28]. On 01 January 2020 a 36 years old female presented for the emergency Caesarean section with symptoms of COVID-19 after delivery neonatal vital signs were stable. The nucleic acid of the pharyngeal and anal swab for SARS-CoV-2 was negative [29]. Among 12 infected pregnant women three patients were died giving a fatality rate of 25%. Spontaneous miscarriage was reported in four out of seven (57.0%) patients in their 1st trimester. In four out of five patients who presented after 24 weeks of gestation delivered preterm. Two pregnant women recovered without delivery but due to intrauterine growth restriction, their on-going pregnancy was complicated. Pregnant women infected with COVID-19 have a high risk of preterm delivery, spontaneous miscarriage, and intrauterine growth restriction [30]. The consequences of Covid-19 disease in women that are pregnant are shown in Table 3.
| Serial.No | Characteristic | Total |
|---|---|---|
| 1 | No of cases | 13 |
| 2 | Asymptomatic | 2 |
| 3 | Died | 3 |
| 4 | Fetal demise | 2 |
| 5 | Pre-term | 2 |
Table 3: Consequences of Middle East Respiratory Syndrome (MERS) in pregnant women [28].
Pregnancy associated within SARS-CoV-1 infection: Severe Acute Respiratory Syndrome (SARS) is responsible for any adverse outcomes like miscarriage, preterm delivery, and maternal death although there is no evidence so far from severe outcomes for mothers and infants; however, the possibility should be considered [31]. A case of 33-year old para 1, gravida 2, pregnant women with 31 weeks of gestation infected with SARS-CoV. With symptoms of dry cough, fever, and patchy infiltrate on chest X-rays, in her 21 days of stay in hospital she doesn't need any ventilator support, ICU. Baby delivered at term with no evidence of infection [32]. A study of case-control type was conducted in Tertiary Hospital Hong Kong. Pregnant women infected with SARS-CoV1 compared with non-pregnant SARS-CoV1 patients. In the pregnant group (n=10) 4/10 pregnant patients, does not require endotracheal intubation and six patients were sensitive and shifted to the ICU. On the other side in the non-pregnant group with 12.5% of patients need intubation and 17.5% of patients need ICU admission. We demonstrate that impact of SARS-CoV1 in pregnant women lead to worse clinical outcome. And the higher risk of mortality and morbidity [33]. SARS infection I associate with spontaneous abortion, critical maternal illness, and maternal death [34,35]. Six studies shares information on SARS-CoV infection in women with pregnancy shown in Table 4 [35-40].
| Serial. No | Author | Study location | Study period | Study design | Pregnancies | Mean maternal age (years) | Type of coronavirus |
|---|---|---|---|---|---|---|---|
| 1 | Yudin, et al. [3] | Canada | Not reported | Case report | 1 | 33 | SARS-CoV |
| 2 | Wong, et al. [4] | Hong Kong, China | 2003 | Retrospective | 12 | 30.6 | SARS-CoV |
| 3 | Lam, et al. [5] | China | 2003 | Retrospective | 10 | 31.6 | SARS-CoV |
| 4 | Robertson, et al. [6] | USA | 2003 | Case report | 1 | 36 | SARS-CoV |
| 5 | Schneider, et al. [7] | United States | 2003 | Case report | 1 | Not reported | SARS-CoV |
| 6 | Stockman, et al. [8] | United States | 2003 | Case report | 1 | 38 | SARS-CoV |
Table 4: Characteristics of included studies. Characteristics of included studies.
MERS-CoV infection associated with pregnancy: Spare data exists to scientific and clinical characteristics of MERS disease during the gestation period, birth, and the postnatal period [41]. Pregnant women infected with MERS-CoV are more prone to morbidity and severe clinical outcome when compared with non-pregnant women. However, today a very few MERS-CoV associated pregnancy cases (n=11) have been registered with (91%) adverse clinical outcome [42]. In February, a total of 2143 cases of Middle East Respiratory Syndrome Coronavirus (MERS-CoV) were reported to the World Health Organization, (WHO) including 750 deaths in 27 countries [43]. There were 10 cases reported with (MERS-CoV) in pregnancy [44]. A study report 5 cases of (MERS-CoV) in pregnancy from Saudi Arabia all cases related to maternal and perinatal death or diseases [45]. An epidemiological investigation by Payne MERS outbreak in Zarqa Jordan, report a case of 2nd trimester with exposure of MERS-CoV. Pregnant women experienced fever, headache, cough, and fatigue concurrently with abdominal pain and vaginal bleeding. She died on the 7th day of appearing the symptoms. Later on, a clinical sample of the women was confirmed with an antibody against MARS-CoV [46]. Different characteristic among five patients are shown in Table 5.
| Characteristic | Patient. No 1 | Patient. No 2 | Patient. No 3 | Patient. No 4 | Patient. No 5 |
|---|---|---|---|---|---|
| Age | 29 years | 39 years | 34 years | 32 years | 31 years |
| Citizenship | Saudi | Saudi | Saudi | Saudi | Saudi |
| Gravida (G) para (P) | G2, P1 | G6, P5 | G7, P6 | G2, P1 | Primigravida |
| ICU admission | No | No | Yes | Yes | Yes |
| Gestational age at illness onset (week) | 6 | 24 | 34 | 38 | 24 |
| Source of infection | From household contact | Contact with MERS-CoV case in HD | Unknown | Unknown | HCW, occupational exposure |
| Maternal co-morbidities | None | ESRD on hemodialysis, HTN | Preeclampsia | None | Asthma, pulmonary fibrosis |
| Maternal outcome | Survived | Survived | Survived | Died | Died |
| Fetal outcome | Survived | Survived | Died | Survived | Died |
| Delivery info | Delivery at term | Delivery at term | Intrauterine fetal death at 34 weeks | Vaginal delivery at 38 weeks | The cesarean section at 24 weeks |
Table 5: An outline of pregnant women correlated with MERS-CoV infection [43].
Pregnancy associated with SARS-CoV-2 infection: In the Covid-19 pandemic, the New York obstetrical population faces a unique challenge in the form of multiple interactions with multiple healthcare practitioners. Between 22 March and April 2020, two hospitals in New York as the name on Presbyterian Allen Hospital and Columbia University Irving Medical Centre present 215 pregnant women for delivery. At the time of admission, four (1.9%) of them tested positive for COVID-19. The nasopharyngeal swab was collected from 210 (99.5%) patients out of 211 patients remember they are asymptomatic. The above cite data are labeled in Figure 3 [47].
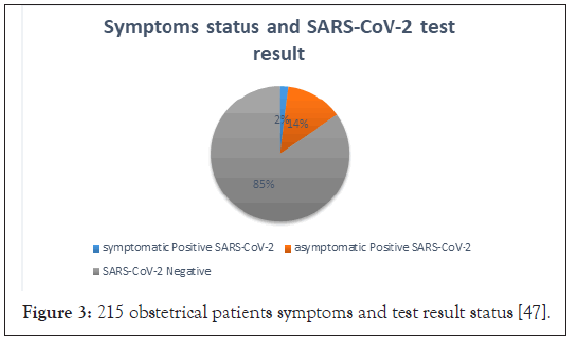
Figure 3: 215 obstetrical patients symptoms and test result status [47].
Summary of (SARS-CoV, MERS, SARS-CoV2) in pregnancy
SARS: Pregnant women infected with SARS reported foetal distress with 35.9% (3 out of 9 foetuses), there is no case of perinatal death although asphyxia in neonates was noted in a few cases. There was no case of admission of infants to ICU. During the follow-up period no new-born show signs of vertical transmission of SARS (Table 6).
| Outcome | SARS | MERS | SARS-CoV2 | |||
|---|---|---|---|---|---|---|
| Studies | fetus/Newborn | Studies | Fetus/Newborn | Studies | Fetus/Newborn | |
| n/N | n/N | n/N | ||||
| Fetal distress | 5 | 3/10 | 4 | 0/5 | 4 | 12/30 |
| Neonatal asphyxia | 4 | 0/4 | 2 | 0/2 | 3 | 0/21 |
| ICU admission | -- | -- | 2 | 0/2 | 2 | 1/10 |
| Perinatal death | 5 | 0/9 | 6 | 3/10 | 5 | 2/41 |
| Vertical transmission | 6 | 0/14 | 4 | 0/4 | 6 | 0/42 |
Table 6: Cumulative proportion of different perinatal consequences explained concerning different infections [40].
MERS: In the 1st trimester is no case of miscarriage among MERS infected pregnant women. Out of seven pregnant women, one case of preeclampsia was reported with (19%). The rate of perinatal death (33%) among pregnant women infected with MERS. There is no data on foetal distress although asphyxia in neonates and many patients were admitted to ICU. Further, follow period no evidence on vertical transmission of MERS (Table 6).
SARS-CoV-2: Pregnant women infected with COVID-19 are no case miscarriage during 1st trimester. There is a very low rate of perinatal death (7%). And a high foetal distress rate of (43%) compared with SARS and MERS infection among pregnant women, the new born was admitted to neonatal ICU. There is no data on neonatal asphyxia. Further, follow period no evidence on vertical transmission (Table 6).
Normal vaginal delivery and caesarean section COVID-19 patients
Currently all over the world maternity units considering management protocol for pregnant patients [48]. Serious morbidity related to Covid-19 occurs in pregnant women compared with SARS and MERS, COVID-19 were identified as not as much as lethal as other [49]. During the current period of emergency, senior obstetrician in Wuhan suggests caesarean section for women with COVID-19 infection should be applied flexibly and the threshold for caesarean section lowered [50]. Previous epidemics of many emerging viral infections resulted in poor obstetrical outcomes including maternal morbidity and mortality, perinatal infections and death, and maternal-foetal transmission of the virus. A study of 38 pregnant women revealed that COVID-19 did not lead to any maternal deaths and importantly there is no confirmed case of intrauterine transmission to their foetus similar in Pregnancies with SARS and MERS [51]. A study of 17 pregnant women scheduled for caesarean section. There was no event of serious neonatal asphyxia or death. SARS-CoV-2 nucleic acid tests were negative among all neonates [52]. There is no clear evidence regarding the safety of vaginal delivery, or whether caesarean delivery prevents vertical transmission at the time of delivery; therefore, the route of delivery should be individualized based on obstetrical indications and maternal-foetal status [53].
Anaesthetic consideration in COVID-19 patients
Anaesthetic consideration for caesarean section in patients with COVID-19 is different from an ordinary surgical procedure. To reduce the effect of drugs on the respiratory and circulatory system of maternal and foetus intraspinal anesthesia is preferred for ordinary COVID-19 Patients. While for critically ill patients general anesthesia suggested [54]. Both epidural and general anesthesia were safely practiced for Caesarean delivery but the incidence of hypotension during epidural anesthesia appeared more [55]. Combine spinal and epidural anesthesia (CSEA) is safe and efficient in achieving satisfactory obstetrical anesthesia and postoperative analgesia among COVID-19 infect pregnant women presenting for caesarean section. No cross infection occurred among Health Care practitioners working in this operation room [56].
Anesthesia in elective caesarean section for ordinary COVID-19 pregnant women
Spinal anesthesia is still recommended as the primary choice of anesthesia for caesarean delivery in a mother with COVID-19 [57]. According to the society of Obstetric anesthesia and perinatology in case of the elective case (elective induction of labour, planned caesarean delivery) patients should be phoned before admission to screen for symptoms consistent with COVID-19 [58]. To avoid the possibility of virus spread anesthesia inform consent signed in the isolation room or ward. Prepare special COVID-19 kit with equipment used for labour delivery and caesarean section. Before entering labour, the room uses the contact and droplet precaution with eye protection (gown, gloves face shield, N95 mask). Although the use of spinal anesthesia is not contraindicated in a patient infected with SARS-CoV-2 early epidural anesthesia reduces the need for analgesia and general anesthesia [59]. After routine monitoring (ECG, Pulse oximetry, and continuous non-invasive blood pressure) Epidural or CSEA is the best choice among pregnant women with Covid-19 [60].
Anesthesia in emergency caesarean section for ordinary COVID-19 pregnant women
For emergency caesarean section proper systematic plan and preparedness for minimizing cross infection [61]. In case of emergency (desaturate>92%) general anesthesia should be administered with Rapid Sequence Induction (RSI) and cuffed Endotracheal tube. If patients have systemic diseases like disseminated intravascular coagulation, renal failure need to use invasive monitoring [62]. Rapid sequence spinal anesthesia is defined as for emergencies caesarean section, pre scrubbed patient in the left lateral position with supplemental oxygen a single shot intraspinal block. The procedural readiness time comparable to general anesthesia and the neonatal outcome is excellent [63]. Extubating protocol should be with the same precaution as with the conduct of intubation [64].
Recommendation for pregnant lady, gynaecologist, and health policymaker
The policies and guidelines concerning infection prevention and control related COVID-19 recommended by WHO and notified by the government to be made mandatory in the hospital in terms of adoption and implementation. The government should ensure the availability of relevant PPE's for health care workers at all costs. Video tutorials, drills, and demonstrations for Infection prevention and control precautions like social distancing, cough etiquettes, handling of patients with relevant PPE's, donning and doffing to be implemented as a matter of routine for all Health Care Workers starting from sanitation staff, Class-4 staff up to professor level including administrative staff. All patients should be encouraged for strictly following hand hygiene and cough etiquettes by providing surgical masks. Appropriate triage mechanism to be implemented as recommended by the government for the segregation of suspected cases both inpatients and attendants. One patient/ one attendant policy should be adopted and strictly implemented with zero tolerance for gatherings. The gates and entrances to wards and delivery suites should be monitored by video cameras and security guards to check their compliance especially at night and in odd hours when this whole building gives an impression of chaos, disarray, and lawlessness with female staff vulnerable and impuissant. Departments should make contingency plans for emergency preparedness and HOD should be made responsible for hire and train accordingly. To lessen stress and anxiety symptoms, staff debriefing sessions must be arranged in the coordination of the psychiatry department to accelerate recovery following recent incidents of COVID-19 positive staff members. To relieve the suffering of the ailing community, O.P.D to be functionalized in light of the guidelines suggested by the government mentioned in the attached document. every patient should be considered as potentially COVID 19 positive until proved otherwise, as due to its varied symptomatology the patient may be in the as asymptomatic carrier state.
In our review study, we conclude that patients with co-morbidities (cancer patients) have a 3-fold increase in death rate and reduce chemotherapy dose. Although there is no evidence to suggest the potential risk of intrauterine vertical transmission among SARS and MERS in previous literature. Although two cases reported of intrauterine vertical transmission in COVID-19. MERS have more percentage of perinatal death than MERS and COVID. Both epidural and general anesthesia is safe and effective for pregnant women and new-borns. And it preserves respiratory function and avoids aerosolization and hence viral transmission Intraspinal injection (Epidural, Spinal) remain the best choice for elective caesarean section patient with COVID-19.
Citation: Tayyeb M, Owais M, Abbas M, Ahmad W, Ullah SA, Jadoon A, et al. (2021) Anaesthetic Management for Emergent Caesarean Delivery in a Parturient with Recent Diagnosis of COVID-19. J Antivir Antiretrovir. 13:206.
Received: 10-Dec-2020 Accepted: 24-Dec-2020 Published: 31-Dec-2020 , DOI: 10.35248/1948-5964.21.13.206
Copyright: © 2020 Khan H, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.