Journal of Depression and Anxiety
Open Access
ISSN: 2167-1044
ISSN: 2167-1044
Research Article - (2022)Volume 11, Issue 12
Introduction: Insufficient and poor quality sleep has plagued contemporary university students in China. As young adults fail to cope with their stress properly, they become vulnerable to psychological distress and sleep disorders during the COVID-19 pandemic.
Methods: A cross-sectional survey was conducted amongst 1326 university students from Hubei Province, China. Latent profile analysis was conducted on results of class-difference tests of sleep patterns. Multiple logistic regressions were used to explore the relationship between the influencing factors and the three classes of sleep quality.
Results: The overall score of sleep quality (9.17 ± 3.22) amongst university students was assessed by using the PSQI scale, and 427 (32.20%) students reported poor sleep quality. Three distinct classes of sleep patterns were identified, namely, good sleepers (Class 1, 70.44%), poor sleep quality with less medication use (Class 2, 26.55%) and poor sleepers (Class 3, 3.01%). Compared with ‘good sleepers’, students having ‘poor sleep quality with less hypnotic drug use’ were affected by their education stage, smoking habits, physical activity, depression and anxiety. Meanwhile, ‘poor sleepers’ were affected by their age, origins, smoking habits, mental stress, depression and anxiety.
Conclusion: Results confirmed a significant heterogeneity in the sleep patterns of university students, and their behavioral lifestyles and mental-health-related factors demonstrated different relationship patterns with sleep quality. Multiple sleep promotion interventions, including moderate aerobic exercises, psychological counseling and mindfulness training, should be performed in groups regularly to improve their sleep quality.
Sleep quality; University students; Depression; Anxiety; Physical activity; Stress
A deep and sufficient sleep has become an immediate need for the public. According to the China sleep research report (2022), most Chinese suffer from sleep deprivation. Over the past decade, the Chinese sleep for an average of 8.5 hours in 2012, this was reduced to 7.06 hours in 2021. In addition, nearly 64.75% of the respondents sleep for less than 8 hours a day. Amongst university students, the most common sleep disorders include Inadequate Sleep Hygiene (ISH), staying up late, daytime dysfunction and insomnia [1-6]. Russell and Petrie demonstrated that students experience an important autonomy and independent process during their university years, which is also considered a key transition period of rapid psychological development [7-9]. Other empirical studies suggest that young adults are vulnerable to negative distress and other psychological problems. Their stress mainly comes from heavy academic pressure, severe employment difficulties and emotional regulation [10-16]. As many students fail to cope with their stress properly, they start to feel helpless and develop negative expectations for their future, both of which lead to psychological disorders. Specifically, depression and mental stress share many cognitive components that can have a strong negative connection to sleep disturbance [17].
Apart from negative emotions, other factors that affect sleep duration include problematic mobile phone or internet use and long work hours, both of which crowd out sleep time. Apart from throwing their psychology and lifestyle off balance, the COVID-19 pandemic has spurred fears of catching the virus or dramatically shifted the learning patterns of university students. During the height of the pandemic, most university students were restricted inside their dormitories or houses, which exacerbated their overuse of mobile devices and resulted in sleep disorders, such as insomnia and disturbed sleep rhythm. Irregular and unhealthy living habits tend to have adverse effects on the endocrine, immune system and metabolism and in turn disturb the underlying mechanisms of normal sleep. A growing body of research shows that good sleep quality and quantity are associated with an appropriate amount of Physical Activity (PA). Other researchers contend that inadequate PA and sedentary behavior can lead to mental health issues and poor sleeping quality amongst students. Using a standardized Pittsburgh Sleep Quality Index (PSQI) instrument. Observed a higher frequency of insomnia symptoms and less restorative sleep amongst smokers than amongst non-smokers. To further understand the relationships amongst these variables in a population of university students, health-related lifestyles should be considered when analyzing those factors that influence their sleep quality.
Previous studies that evaluate the sleep quality of university students mainly categorized their participants into ‘good’ and ‘poor’ sleepers based on substantive domains of assessment. However, whether the sleep patterns and sleep related potential risk factors of university students have various manifestations remains unknown. In addition to their complexities, those factors that influence sleep quality show obvious group heterogeneity. Following a ‘person-centered’ approach, this study employs Latent Profile Analysis (LPA) to examine the distinctiveness of the sleep quality sub-types of university students and to identify their potential sleep categories based on their symptoms. This study aims to assess the sleep status of university students during the COVID-19 pandemic and to identify those factors affecting their sleep quality. Those students reporting poor sleep related impairments and sleep deprivation are hypothesized to have an unhealthy behavioral lifestyle, mental stress and depression.
Study design and participants
A cross-sectional study was designed to assess the sleep quality of university students in Hubei Province, China. Wuhan city was taken as the survey anchor, and university students from the cities of Xiao an and Huanggang (about half an hour away from Wuhan) were recruited via convenience sampling. A 100-item self-designed questionnaire was constructed under the guidance of previous studies and related theories. This questionnaire comprised the following parts: 1) basic information, which asked for the gender, age, origins, education stage and other basic personal characteristics of the participants; 2) the PSQI; 3) the 10-item version of the Centre for Epidemiological Studies Depression Scale (CESD-10); and 4) a PA measurement. All participants provided their informed consent before answering the questionnaire. The following inclusion criteria were adopted in the sampling: 1) ≥ 16 years of age; 2) no mental disorders; and 3) pursuing undergraduate degrees.
Measurement
Pittsburgh Sleep Quality Index (PSQI): The sleep quality of the participants was assessed by using the Chinese version of PSQI (revised by Liu Xianchen). This scale contained 18 items and 7 components, namely, subjective sleep quality, sleep latency, sleep duration, sleep efficiency, sleep disturbance, hypnotic drug use and daytime dysfunction. Each component was weighted equally on a scale of 0 to 3, with a total score ranging from 0 to 21. A higher score corresponded to a poorer sleep quality. The PSQI scale had a Cronbach’s alpha of 0.728.
Depression: CES-D10 was used to measure the depressive symptoms amongst the participants. An example item was ‘I felt upset this week’. The participants were required to report how they had been feeling during the previous week on a 3-point scale, ranging from 0 (‘less than 1 day’) to 3 (‘5 to 7 days’). The total score ranged from 0 to 30, with a higher score indicating more depressive symptoms. CES-D10 has reported good internal reliability and validity in previous studies.
Physical activity: Self-report items were used to measure the PA of the participants. The items ‘Over the last week, how often have you exercised for at least 30 minutes per day?’, ‘How long do you usually exercise per day last week?’ and ‘How intense are your physical activities?’ were rated on a 5-point Likert scale. This PA measurement had a Cronbach’s alpha of 0.790. An exploratory factor analysis was performed to test the validity of this scale, and a KMO value of 0.753 and significant Bartlett’s sphericity (P<0.001) were obtained. This validity and reliability of this measure were also supported in previous research.
Data collection: This survey was carried out by online survey from December 2021 to January 2022. Participants were recruited from 9 universities (including science and technology universities, normal universities, medical universities and comprehensive universities) in Wuhan, Huanggang and Xiaogan cities of Hubei Province, China. At least 100 students were selected from each university. They completed the questionnaires voluntarily through a WeChat QR code or Wenjuanxing link for cluster sampling. Dedicated quality controllers were trained to eliminate the invalid questionnaires by inspecting their time, content quality and data format. A total of 1361 questionnaires were received, of which 1326 were deemed valid, yielding an effective recovery rate of 97.43%.
Data collection
This survey was carried out by online survey from December 2021 to January 2022. Participants were recruited from 9 universities (including science and technology universities, normal universities, medical universities and comprehensive universities) in Wuhan, Huanggang and Xiaogan cities of Hubei Province, China. At least 100 students were selected from each university. They completed the questionnaires voluntarily through a WeChat QR code or Wenjuanxing link for cluster sampling. Dedicated quality controllers were trained to eliminate the invalid questionnaires by inspecting their time, content quality and data format. A total of 1361 questionnaires were received, of which 1326 were deemed valid, yielding an effective recovery rate of 97.43%.
Statistical analyses
Data were entered into Microsoft Excel 2016, and the descriptive statistics were analysed using SPSS 24.00. The LPA on the results of class difference tests of sleep quality was conducted using Mplus 7.0. To determine the optimal number of profiles in the data, the LPA model evaluation indicators were used, including the Akaike Information Criterion (AIC), Bayesian Information Criterion (BIC) and adjusted BIC (aBIC). A smaller value of these indices indicates a better model fit. The entropy index is commonly used in previous research to evaluate the classification quality of a model. The LPA model obtained an entropy index of over 0.80, indicating a classification accuracy of over 90%. Meanwhile, results of the Lo–Mendell– Rubin (LMR) likelihood ratio test and Bootstrap-Based Likelihood Ratio Test (BLRT) were P<0.05, indicating that the model with K categories was superior to that with K-1 categories. Multiple logistics regression was performed on potential types of sleep quality using the R3.6.0 software, and the difference was statistically significant at P<0.05.
Demographic characteristics
Amongst the 1,326 participants, 938 were female (70.7%), 792 (59.7%) were from rural areas, 66 (35.1%) had below undergraduate education levels, 744 (56.1%) were undergraduates, 116 (8.7%) were pursuing a master’s degree or higher and 1243 (93.8%) were living in their university apartments. These participants had a mean age of 19.54 ± 2.47 years (Table 1).
| Dimension | M ± SD | 0 (N/%) | 1 (N/%) | 2 (N/%) | 3 (N/%) |
|---|---|---|---|---|---|
| score of PSQI | 9.17 ± 3.22 | ||||
| subjective sleep quality | 1.05 ± 0.74 | 278 (20.97) | 763 (57.54) | 230 (17.35) | 55 (4.15) |
| sleep latency | 1.14 ±0.95 | 375 (28.28) | 531 (40.05) | 277 (20.89) | 143 (10.78) |
| sleep duration | 1.95 ± 1.43 | 465 (35.07) | 778 (58.67) | 69 (5.20) | 14 (1.06) |
| sleep efficiency | 2.43 ± 1.13 | 217 (16.37) | 36 (2.72) | 40 (3.02) | 1033 (77.90) |
| sleep disturbance | 0.92 ± 0.64 | 314 (23.68) | 825 (62.22) | 168 (12.67) | 19 (1.43) |
| hypnotic drug use | 0.11 ± 0.48 | 1250 (94.27) | 36 (2.71) | 14 (1.06) | 26 (1.96) |
| daytime dysfunction | 1.58 ± 0.90 | 170 (12.82) | 418 (31.52) | 539 (40.65) | 199 (15.01) |
Table 1: Evaluation score of each sleep quality component amongst university students.
The overall score of sleep status (9.17 ± 3.22) amongst the participants was assessed using the PSQI scale. The mean and standard deviation for the 7 dimensions are shown in (Table 1), amongst which sleep duration (1.95 ± 1.43), sleep efficiency (2.43 ± 1.13) and daytime dysfunction (1.58 ± 0.90) obtained the highest scores. Meanwhile, subjective sleep quality (1.05 ± 0.74), sleep latency (1.14 ± 0.95), sleep disturbance (0.92 ± 0.64) and hypnotic drug use (0.17 ± 0.53) obtained relatively low scores.
Amongst the 1326 participants, 17 (13.27%) reported that they had a good sleep quality, 688 (51.89%) reported having general sleep quality and 427 (32.20%) reported poor sleep quality (Table 2, Figure 1).
| Model | AIC | BIC | aBIC | Entropy | P Value | |
|---|---|---|---|---|---|---|
| LMR | BLRT | |||||
| Class 1 | 21047.72 | 21120.38 | 21075.91 | <0.001 | <0.001 | |
| Class 2 | 20041.02 | 20155.2 | 20085.32 | 0.807 | <0.001 | <0.001 |
| Class 3 | 17818.29 | 17973.99 | 17878.69 | 0.841 | <0.001 | <0.001 |
| Class 4 | 16792 | 16989.23 | 16868.52 | 0.853 | 0.855 | 1 |
Note: AIC = Akaike information criterion; BIC=Bayesian information criterion; aBIC = adjusted BIC; LMR-LRT=Lo–Mendell–Rubin likelihood ratio test; BLRT=bootstrap-based likelihood ratio test.
Table 2: Latent class model fit indicators of the Pittsburgh sleep quality index (N=1326).
Latent profile analysis
Table 2 shows the number classification of the LPA analysis. A significant decline was observed in AIC, BIC and aBIC. The p value of LMR and BLRT further indicated that a 3-class solution yielded the best fit for the data, and such fit was significantly better than that of a 4-class model (p<0.001). Therefore, the 3-class model was considered the optimal classification for this study (Figure 1).
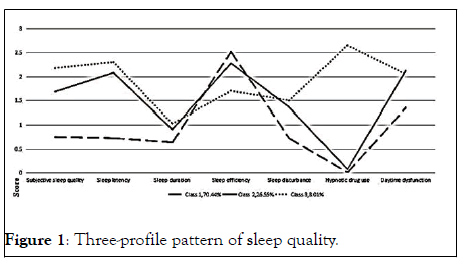
Figure 1: Three-profile pattern of sleep quality.
Distinct subgroups of the sleep quality of university students
Three profiles of PSQI (Class 1, Class 2 and Class 3) are shown in (Figure 1). Profile 1, labeled as ‘good sleepers’ (N=934, 70.44%), was characterized by a low probability of responding ‘high’ to any sleep component except for “sleep efficiency’. Profile 2, labeled as ‘poor sleep quality with less hypnotic drug use’ (N=352, 26.55%), was characterized by a relatively low probability of responding ‘high’ to all sleep components except for ‘daytime dysfunction’. Profile 3, labeled as ‘poor sleepers’ (N=40, 3.01%), was characterized by relatively higher scores for each sleep component compared with those in the two other profiles, especially for ‘hypnotic drug use’ (Table 3).
| Variable | Class 1 | Class 2 | Class 3 | χ2 | P |
|---|---|---|---|---|---|
| N= 934 | N=352 | N=40 | |||
| -70.44% | -26.55% | -3.01% | |||
| Age ≤ 18 | 454 (48.60) | 161 (45.74) | 9 (22.50) | 10.83 | 0.004 |
| > 18 | 480 (51.40) | 191 (54.26) | 31 (77.50) | ||
| Gender Male | 282(30.19) | 91 (25.85) | 15 (37.50) | 2.68 | 0.16 |
| Female | 652 (69.81) | 261 (74.15) | 25 (62.50) | ||
| Student’s origin place | 9.12 | 0.01 | |||
| Urban | 376 (40.26) | 133 (37.78) | 25 (62.50) | ||
| Rural | 558 (59.74) | 219 (62.22) | 15 (37.50) | ||
| Lunch break | |||||
| None | 179 (19.17) | 89 (25.28) | 9 (22.50) | 13.17 | 0.01 |
| ≤ 30 min | 384 (41.11) | 119 (33.81) | 9 (22.50) | ||
| >30 min | 371 (39.72) | 144 (40.91) | 22 (55.00) | ||
| Education stage | 7.79 | 0.1 | |||
| Below undergraduate | 316 (33.83) | 140 (39.77) | 10 (25.00) | ||
| Undergraduate | 541 (57.92) | 178 (50.57) | 25 (62.50) | ||
| Master degree or above | 77 (8.24) | 34 (9.66) | 5 (12.50) | ||
| Graduation confidence | |||||
| No confidence | 23 (2.50) | 31 (8.81) | 8 (20.00) | 44.82 | 0 |
| Have confidence | 911 (97.50) | 321 (91.19) | 32 (80.00) | ||
| Smoking | 44.38 | 0 | |||
| None | 904 (96.79) | 326 (92.61) | 30 (75.00) | ||
| Yes | 30 (32.11) | 26 (7.39) | 10 (25.00) | ||
| Drinking | 8.24 | 0.016 | |||
| None | 544 (58.24) | 180 (51.14) | 17 (42.50) | ||
| Yes | 390 (41.76) | 172 (48.86) | 23 (57.50) | ||
| Sedentary screen | 4.28 | 0.118 | |||
| None | 584 (62.53) | 198 (56.25) | 25 (62.50) | ||
| Yes | 350 (37.47) | 154 (43.75) | 15 (37.50) | ||
| Sedentary book | 2.55 | 0.28 | |||
| None | 861 (92.18) | 316 (89.77) | 38 (95.00) | ||
| Yes | 73 (7.82) | 36 (10.23) | 2 (5.00) | ||
| Mental stress | 65.09 | 0 | |||
| None | 861 (92.18) | 288 (81.82) | 23 (57.50) | ||
| Yes | 73 (7.82) | 64 (18.18) | 17 (42.50) | ||
| Physical activity | 31.51 | 0 | |||
| Insufficient active | 459 (49.14) | 234 (66.48) | 24 (60.00) | ||
| Active | 475 (50.86) | 118 (33.52) | 16 (40.00) | ||
| Depression | 204.04 | 0 | |||
| None | 664 (71.09) | 104 (29.55) | 9 (22.50) | ||
| Have | 270 (28.91) | 248 (70.45) | 31 (77.50) | ||
| Anxiety | 131.78 | 0 | |||
| None | 747 (79.98) | 185 (52.56) | 11 (27.50) | ||
| Yes | 187(20.02) | 167 (47.44) | 29 (62.50) | ||
Table 3: Univariate analysis of different sleep types amongst university students.
Table 3 summarizes and compares the differences in the sociodemographic and lifestyle characteristics of the students in the three aforementioned profiles. The differences in the sleep patterns of the university students were statistically significant in terms of age (X2=10.83, P=0.004), origin (X2=9.12, P=0.01),lunch break (X2=13.17, P=0.01), graduation confidence (X2=44.82, P<0.001), smoking habit (X2=44.38, P<0.001), drinking habit (X2=8.24, P=0.016), mental stress(X2=65.09, P<0.001), PA (X2=31.51, P<0.001), depression (X2=204.04, P<0.001) and anxiety (X2=131.78, P<0.001) (Table 4).
| Variable | Class 2 vs Class 1 | Class 3 vs Class 1 | ||||||
|---|---|---|---|---|---|---|---|---|
| β | P | OR | 95%CI | β | P | OR | 95%CI | |
| Gender | 0.23 | 0.19 | 1.25 | 0.92-1.59 | 0.13 | 0.75 | 1.14 | 0.35-1.68 |
| Age | 0.18 | 0.236 | 1.21 | 0.89-1.52 | 1.13 | 0.011* | 3.08 | 2.21-3.41 |
| Student’s origin 0.08 | 0.556 | 1.09 | 0.80-1.38 | -0.94 | 0.013* | 0.39 | -1.08 | |
| place (refer urban) | ||||||||
| Education stage | ||||||||
| Undergraduate | -0.42 | 0.012* | 0.65 | 0.32-0.98 | -0.34 | 0.456 | 0.71 | -1.28 |
| Master degree or above | -0.2 | 0.476 | 0.81 | 0.24-1.38 | -0.64 | 0.346 | 0.52 | -1.68 |
| Graduation | -0.43 | 0.165 | 0.65 | 0.03-1.26 | -1.04 | 0.054 | 0.35 | -1.37 |
| Confidence | ||||||||
| Smoking | 0.64 | 0.000** | 1.91 | 1.28-2.54 | 2.3 | 0.000** | 9.94 | 8.92-10.26 |
| Drinking | 0.22 | 0.12 | 1.26 | 0.97-1.54 | -0.11 | 0.773 | 0.89 | 0.13-1.67 |
| Mental stress | 0.38 | 0.536 | 1.47 | 1.05-1.88 | 1.33 | 0.001* | 3.78 | 2.99-4.86 |
| Physical activity (Refer active) | 0.47 | 0.001* | 1.61 | 1.32-1.90 | 0.23 | 0.536 | 1.26 | 0.52-2.23 |
| Depression | 1.4 | 0.000** | 4.06 | 3.76-4.36 | 1.14 | 0.012* | 3.15 | 2.38-4.40 |
| Anxiety | 0.64 | 0.000** | 1.91 | 1.60-2.22 | 1.26 | 0.000** | 3.54 | 2.70-4.50 |
Notes: *P<0.05 * *P<0.001
Table 4: Multiple logistic regression analysis of the influencing factors amongst the different sleep classes of university students.
Table 4 presents the results of the multinomial logistic regression for predicting the three latent profiles. To prevent and reduce the detrimental effect of PSQI, Class 1 was designated as the referent cluster and compared with the two other two groups. Compared with class 1, class 2 was affected by education stage, smoking habit, PA, depression and anxiety. Those university students with a below undergraduate education level (OR=0.65 P=0.012), smoking habit (OR=1.91 P< 0.001)), regular PA (OR=1.61 P=0.001), depression (OR=4.06 P<0.001) and anxiety (OR=1.91 P<0.001) were significantly more likely to be in Class 2.
The sleep quality of the participants in class 3 was affected by age, origin, smoking habit, mental stress, depression and anxiety. Those university students who were aged ≥ 18 years were more likely to be in class 3 compared with those students aged below 18 years (OR=3.08 P=0.011). University students coming from urban areas (OR=0.39 P=0.013) and with unhealthy behavioral and psychological lifestyles, such as smoking (OR=9.94 P<0.001), mental stress (OR=3.78 P=0.001), depression (OR=3.15 P=0.012) and anxiety (OR=3.54 P<0.001), also showed a high likelihood to belong to this class.
A sleep disorder detection rate of 34.84% was recorded amongst the participants, and this value is higher than the sleep disorder rate (13.22%) of university students previously surveyed in Tianjin, China. Meanwhile, the overall score of sleep quality (9.17 ± 3.22) was above the norm (5.26 ± 2.38). These results underscore the prominence of sleep disorders amongst the surveyed university students. By further analyzing the homogeneous groups of individuals, the LPA method identified 3 latent profiles, namely, good sleepers (70.44%), poor sleep with less hypnotic drug use (26.55%) and poor sleepers (3.01%). Amongst the 5 components in PSQI, actual sleep time (1.95 ± 1.43) and sleep efficiency (2.43 ± 1.13) obtained the highest scores, which may be ascribed to the multiple internal dimensions of sleep problems. Hypnotic drug use (0.17 ± 0.53) was also uncommon amongst the university students, that is, these students showed low dependence on hypnotic drugs for improving their sleep quality. This finding may be ascribed to the possibility that most of these students only have mild sleep disorders and that they are very cautious about the side effects of these drugs. Moreover, young adults are relatively energetic and confident in their health coping ability. The interview data revealed that the participants tended to use alternative ways to address their sleep problems instead of relying on hypnotic drugs.
The senior students demonstrated a higher likelihood to have poor sleep quality compared with the lower-level students possibly due to the fact that these students are facing direct pressure to look for jobs or pursue further education. For instance, the number of regular Chinese university graduates in 2021 was reported to be 9.09 million, which were 350,000 greater than the number reported in the previous year. Faced with new challenges and uncertainties in a new era, university graduates face fierce competition in the Labour market. Moreover, the COVID-19 pandemic has reduced the number of employment opportunities, hence pushing more university students to pursue higher education instead, hence intensifying the competition for graduate studies. These pressures increased the anxiety of senior students, thereby leading to their poor sleep quality.
Students from rural areas (OR=0.39; 95% CI-0.36, 0.72) are not prone to having sleep problems, which contradicted the results of a previous study. This finding may be ascribed to their affective coping styles. Specifically, urban students prefer to suppress their modes of expression or regulate their emotions; in other words, instead of focusing on their emotional states, they avoided interpersonal communication. Accordingly, urban university students excessively use their mobile phones or play computer games at night to eliminate negative emotions, and the excessive amount of time they spend on these activities leads to an inefficient and inadequate sleep.
A common factor shared by the class 2 and class 3 students is anxiety. Those university students with anxiety are more likely to be in either class 2 (OR=1.91; 95% CI 1.60, 2.22) or class 3 (OR=3.54; 95% CI 2.70, 4.50). Poor sleep quality is not only a subjective wakefulness disorder but is also caused by psychological disorders. Sleep quality is uniquely associated with perceived stress and psychological factors. Previous research has also identified university students as a group facing a high incidence of anxiety. These students face challenges in adapting to psychologically stressful scenarios, including competitive academic pursuits, employment anxiety, social phobia, COVID-19 insecurity and negative emotion. This might explain their poor sleep quality.
Students with depression have a high likelihood to be in class 2 (OR=4.06; 95% CI 3.76, 4.36). Students with depressive symptoms or mental stress (OR=3.78; 95% CI 2.99, 4.86) may suffer from poorer sleep quality than those without mental health problems. This view was supported by previous studies and may be ascribed to the fact that depression weakens the regulation function of the human serotonin system, which reduces sleep quality by suppressing slow-wave sleep, increasing wakefulness and introducing difficulties in falling asleep or sleep maintenance disorder. Stephen highlighted the importance of evaluating multiple mental health symptoms simultaneously given that the associated mental health symptom dimensions strongly interact with one another. A higher level of mental stress corresponds to a worse quality of sleep. Mental stress can activate the brain in its high excitatory state and, as a result of long-term tension, may consume many body functions continuously, hence affecting sleep quality.
Sleep quality is also associated with unhealthy behaviors. Those students who smoke (OR=9.94; 95% CI 8.92-10.26) tend to be in class 3. An experiment amongst young smokers in Germany revealed that some changes in sleep patterns depend on the amount of daily tobacco consumption and level of serum cotinine in the body, hence proving that the nicotine from tobacco can influence the sleep-regulating mechanisms of the body. These effects stimulate the release of dopamine, norepinephrine, serotonin and acetylcholine, all of which define the arousal levels of wakefulness.
PA plays a proactive role in sleep quality. Those people who seldom take part in PA (OR=1.61; 95% CI 1.32, 1.90) tend to demonstrate poor sleep quality. Oliveira proposed that regular PA will increase the body temperature and in turn stimulate the hypothalamus to control the heat dissipation mechanism of the body, hence triggering and increasing slow-wave sleep, which is conducive to entering the deep sleep stage quickly and increasing the need for sleep to achieve anabolism. These results altogether show that psychological well-being and behaviors are vital in sleep regularity and satisfaction.
This study has several limitations. Firstly, using a cross-sectional design did not produce very precise or convincing results, hence preventing this research from establishing a causal conclusion. In-depth longitudinal studies should therefore be carried out in the future. Secondly, all information presented in this study was assessed using self-reported questionnaires, which are prone to subjective bias. Future research may combine self-reported questionnaires with objective measurements or diagnosis results to improve the scientificity of their findings.
This study explored the 3 latent classes of sleep quality of 1326 university students in Hubei Province, China during the COVID-19 pandemic by conducting PSQI measurements. Results show that behavioral lifestyle (e.g. smoking habit and PA) and mental health related factors (e.g. anxiety, depression and mental stress) are consistently and strongly correlated with the sleep quality of these students. Universities and psychological consulting centers should organize regular psychological problems screening and focus on those students with mental health problems. They should help these students improve their ability to self-manage their sleep and actively engage in PA (e.g. moderate aerobic exercises) by regularly carrying out multiple health promotion interventions in groups and publicizing the benefits of sleep through we chat or TikTok. Mindfulness intervention as a potential pathway can help students relieve their negative emotions effectively and cultivate positive stress coping strategies. This intervention may help students minimize their poor cognitive behavioral patterns and subsequently improve their sleep quality.
DF and ZCF contributed to conceptualization and project administration. CY: writing-original draft, writing-review and editing. ZC contributed to data collection and visualization, SY: analysis and interpretation of data, ZQ and GY contributed to raising many useful amendments of this article. ZM: data duration, writing-review and editing. Last, all the authors contributed to implement and revise the manuscript.
We would like to thank all the participants for participating in the study and all coordinators in the project for their efforts in data collection.
This research was funded by National Key R&D Program of China (Grant No. 2020YFC2006500).
We declared that all the authors in our study that have no conflicts of interests.
This study was approved by the ethics committees of the Tongji Medical University and the Huazhong University of Science and Technology under Grant No. 2021S317.
Informed consent was obtained from all subjects involved in the study.
The datasets used or analyzed during the current study are available from the corresponding author on reasonable request.
[Crossref]
Citation: Chen C, Feng D, Song S, Chen Z, Yan Z, Feng Z, et al. (2022) Analysis of the Potential Profile and Predictors of Sleep Quality among University Students during the COVID-19 Pandemic in Hubei Province, China. J Dep Anxiety. 11:478.
Received: 28-Nov-2022, Manuscript No. JDA-22-17308; Editor assigned: 01-Dec-2022, Pre QC No. JDA-22-17308(PQ); Reviewed: 16-Dec-2022, QC No. JDA-22-17308; Revised: 23-Dec-2022, Manuscript No. JDA-22-17308(R); Accepted: 30-May-2023 Published: 31-Dec-2022 , DOI: DOI: 10.35248/2167-1044.22.11. 478
Copyright: © 2022 Chen C, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.