Pancreatic Disorders & Therapy
Open Access
ISSN: 2165-7092
ISSN: 2165-7092
Research Article - (2024)Volume 14, Issue 4
Acute Necrotic Collection (ANC) and Walled-off Necrosis (WON) are two types of acute necrotizing pancreatitis complications that determined according to the duration of collection (>4 weeks) and a weakly formed wall. The risks and benefits of endoscopic treatment of pancreatic necrosis, which occurs approximately four weeks after the onset of illness, can be discussed in our work. In the late stage of Atrial Natriuretic Peptide (ANP), Walled-off Pancreatic Necrosis (WOPN) is typically treated by EUS-guided transmural endoscopic drainage. In the initial stages of ANP, the function of endoscopic intervention is controversial and not clear. The objective of this study was to compare endoscopic draining of early WOPN with endoscopic treatment.
Materials and methods: In total, 142 patients with ANP underwent endoscopy. Endoscopic intervention was performed within the first four weeks of ANP in 50 (35.21%) patients with ANC (Group 1) and 92 (64.79%) patients four weeks after the onset of ANP with WOPN (Group 2). We aimed to improve our conclusions about early WON therapy by matching patients with WON to early intervention cases. The primary outcome was defined as the resolution of collection after endoscopic treatment.
Results: The average age of the patients was 49.9 years (range, 22-79 years), and 59% of them were male in both groups. The mean active drainage timing for group 1 was 26.8 and 16.9 days, while for group 2, it was 270.8 and 164.2 days. The median number of endoscopic drainages in Group 2 was between 4.5 and 9.5 (p=0.0001). The long- term success rates did not differ significantly between the groups (p>0.05). The primary result of early WON timing, based on the additional subgroups, showed no deaths and similar rates of serious side effects after initial assistance, but the total period of treatment was longer (103 vs. 69 days, p=0.042) than that in the matching control group.
Conclusion: Using endoscopy, early ANCs can be successfully treated during the first four weeks of ANP. However, more procedures and a longer drainage period are needed in comparison with early endoscopic intervention in WOPN.
Acute necrotizing pancreatitis; Abdominal compartment syndrome; Direct endoscopic necrosectomy; Walled-off pancreatic necrosis; Early and late endoscopic drainage
Necrotizing Acute Pancreatitis (ANP) occurs in twenty to forty percent of instances cases of acute pancreatitis result in Necrotizing Acute Pancreatitis (ANP) [1]. Solid materials in ANP frequently liquefy after four weeks [2-5]. One frequent side effect of ANP is Infected Necrotizing Pancreatitis (INP) [4,5]. About half the patients showed improvement, and the other half did not. Treatments that have been suggested include fluid rehydration, antibiotics, and monitoring [5,6]. The clinical status of the patient in both the early and late stages of the disease dictates the types of ANP therapy that are used [7-9]. Aggressive conservative therapy is the best course of action, and it should be followed by drainage or necrosectomy as an interventional treatment [10-12]. Patients with ANP who do not respond to conservative treatment or minimally invasive techniques may require an open necrosectomy [11,12]. Since conventional surgery carries a high risk of death and complications, less invasive treatments such as percutaneous Trans peritoneal drainage and retroperitoneal drainage may be considered the primary type of therapy if conservative treatment improves the overall status [12].
International recommendations now in effect state that invasive operations for pancreatic necrosis should be delayed for a minimum of four weeks after the onset of symptoms [3,5,7,12]. Many experts have recommended using fluid drainage or percutaneous therapy in addition to antibiotic therapy [12]. According to a recent study by Trikudanathan, et al. [13], collections older than four weeks and supplies younger than four weeks exhibited increased mortality and required rescue surgery following endoscopic intervention. Nevertheless, the study did not give the precise imaging features of the walls of the necrotic collections or the time interval between the onset of symptoms and intervention. Patients who had previously had percutaneous drainage were included in this analysis.
Endoscopic intervention safety and effectiveness are unknown (WON) [13-18]. Ten to twenty percent of those patients have pancreatic necrosis; the remaining twenty to thirty percent die from Walled-off pancreatic Necrosis (WON). For an infected WON, several researchers have suggested a less invasive draining technique. Nonetheless, there is ongoing discussion over the best method and time for necrosectomy [19]. Global regulations currently recommend the endoscopic step-up technique at this time. The current evidence supports the use of Direct Endoscopic Necrosectomy (DEN) at the time of stent implantation based on a large national cohort. WON recuperates faster, requiring fewer surgeries for necrosectomy [19]. When infectious necrosis is detected, a careful early antibiotic course of therapy is advised based on the outcomes of the step-up method. Additional research on this treatment approach, including ways to enhance the prudent use of antibiotics, is warranted. Endoscopic drainage is performed throughout the first four weeks after ANP until the wall is wholly formed [19]. Acute Physiology and Chronic Health Evaluation II, Sequential Organ Failure Assessment (SOFA), and Ran son scores must be used to evaluate each sensitive pancreatitis patient upon admission and on the second day of care [2,3,16- 18]. No matter how their treatment was handled, all patients with acute pancreatitis underwent Contrast-Enhanced Computed Tomography (CECT) if, within 48 hours of admission, there was no clinical improvement indicating the presence of infected necrosis. Computed tomography assessed severity index values [2,3,18]. This study sought to prospectively assess endoscopic draining of WOPN using early endoscopic methods for ANCs. The WON subgroup, 19 WON-matched patients for early intervention, and 19 control cases for early endoscopic procedures are included to show outcome-based WON therapy.
Endoscopy was used to treat 142 patients with drainage of Acute Necrotizing Pancreatitis (ANP). Fifty patients (35.21%) with ANC comprised Group 1, and ninety-two patients (64.79%) with WOPN treated with endoscopy for drainage in the first four weeks after ANP comprised Group 2. The investigation was conducted at the endoscopic surgical facilities of Zagazig University Hospital. A subgroup of 38 cases was used to ascertain precise outcomes after early endoscopic intervention in the WON subgroup. The first subgroup consisted of 19 matched patients for early endoscopic therapy and the second subgroup consisted of 19 control cases for an early endoscopic approach.
Patients' choice
Qualifications for inclusion in all cases: Patients with necrotic collections (ANC or WON) who underwent endoscopic drainage and who had clinical symptoms and imaging findings were included in the study. Endoscopic intervention was delayed until fluid accumulation was employed (WOPN), which occurred four weeks after the disease began, as indicated by abdominal imaging. If the patient's physical condition did not improve after receiving extensive, optimal conservative treatment in the early phase of ANP (Group 1), endoscopic surgery was performed within four weeks of the onset of acute pancreatitis onset. However, four weeks after the onset of sickness, Group 2 underwent endoscopy. Patient features are listed in Table 1. Radiological and clinical methods were used to identify necrotic collections. Indications for late-stage ANP treatment include acute discomfort, weight loss, Abdominal Compartment Syndrome (ACS) and toxemia. Other factors to be considered include clinical, laboratory, and pressure-related symptoms, and imaging studies. Additional indications are listed in Table 2. Serious indicators of toxemia and septic shock include a poor response to fluids, antibiotics, and medical care. The necrotic contents melted and the necrotic collection was walled off with delayed therapy for at least four weeks after the onset of ANP. During the first four weeks of ANP, interventional treatment was necessary if aggressive care and management improvements did not materialize.
| Variables | ANC (n=50) | WON (n=92) | Total (n=142) | p-value |
|---|---|---|---|---|
| Sex | ||||
| Female | 4 (8.0%) | 20 (21.7%) | 24 (16.9%) | 0.1401 |
| Male | 26 (92.0%) | 72 (78.3%) | 118 (83.1%) | |
| Age (years) | ||||
| Mean (SD) | 44.0 (14.4) | 53.2 (13.9) | 49.9 (14.7) | 0.0114 |
| Range | 22.0-74.0 | 25.0-79.0 | 22.0-79.0 | |
| Median | 42 | 56 | 50 | |
| 95% CI | 38.1-50.0 | 49.0-57.3 | 46.5-53.4 | |
| Etiology | ||||
| Alcoholic | 40 (80.0%) | 54 (58.7%) | 94 (66.2%) | 0.0699 |
| Non-alcoholic | 10 (20.0%) | 19 (41.3%) | 48 (33.8%) | |
| The time among the beginning of pancreatitis and therapy (days) | ||||
| Average (SD) | 16.4 (4.9) | 74.5 (45.9) | 54.0 (46.3) | 0.0001 |
| Range | 8.0-25.0 | 30.0-240.0 | 8.0-240.0 | |
| Median | 16 | 56.5 | 44 | |
| 95% CI | 14.3-18.4 | 60.9-88.1 | 43.1-65.0 | |
| Ranson score (day 0) | ||||
| Mean (SD) | 1.7 (1.1) | 1.3 (1.0) | 1.5 (1.1) | 0.1662 |
| Range | 0.0-4.0 | 0.0-4.0 | 0.0-4.0 | |
| Median | 2 | 1 | 1 | |
| 95% CI | 1.3-2.2 | 1.0-1.6 | 1.2-1.7 | |
| Ranson score (day 2) | ||||
| Mean (SD) | 3.3 (1.3) | 2.5 (1.2) | 2.8 (1.3) | 0.0186 |
| Range | 1.0-6.0 | 0.0-5.0 | 0.0-6.0 | |
| Median | 3 | 2 | 3 | |
| 95% CI | 2.8-3.9 | 2.2-2.9 | 2.5-3.1 | |
| APACHE II score | ||||
| Mean (SD) | 12.7 (4.1) | 11.0 (4.3) | 11.6 (4.3) | 0.1324 |
| Range | 6.0-20.0 | 2.0-21.0 | 2.0-21.0 | |
| Median | 13 | 10.5 | 11 | |
| 95% CI | 11.0-14.4 | 9.7-12.2 | 10.5-12.6 | |
| SOFA score | ||||
| Mean (SD) | 3.8 (2.2) | 2.5 (1.1) | 3.0 (1.7) | 0.0143 |
| Range | 1.0-8.0 | 0.0-5.0 | 0.0-8.0 | |
| Median | 4 | 2.5 | 3 | |
| 95% CI | 2.9-4.7 | 2.1-2.8 | 2.6-3.4 | |
| CTSI | ||||
| Mean (SD) | 8.1 (1.3) | 7.7 (1.3) | 7.8 (1.3) | 0.2062 |
| Range | 6.0-10.0 | 5.0-10.0 | 5.0-10.0 | |
| Median | 8 | 7 | 8 | |
| 95% CI | 7.6-8.7 | 7.3-8.0 | 7.5-8.1 | |
| Initial size of the necrotic collection (mm) | ||||
| Mean (SD) | 185.2 (68.1) | 123.0 (47.7) | 144.9 (62. 8) | 0.0001 |
| Range | 88.0-320.0 | 68.0-247.0 | 68.0-320.0 | |
| Median | 178 | 117 | 130 | |
| 95% CI | 157.1-213.3 | 108.9-137.2 | 130.1-159.8 | |
| Percentage of necrosis | ||||
| 25%-50% | 0 (0.0%) | 19 (19.6%) | 18 (12.7%) | 0.0027 |
| 50%-75% | 14 (28.0%) | 44 (47.8%) | 58 (40.8%) | |
| >75% | 36 (72.0%) | 30 (32.6%) | 66 (46.5%) | |
| Type of necrosis | ||||
| Central | 0 (0.0%) | 18 (19.6%) | 18 (12.7%) | 0.0132 |
| Peripheral | 0 (0.0%) | 8 (8.7%) | 8 (5.6%) | |
| Mixed | 50 (100.0%) | 66 (71.7%) | 116 (81.7%) | |
Table 1: Features of the Patients.
| Indication | ANC (n=50) | WON (n=92) | Total (n=142) | p-value |
|---|---|---|---|---|
| Infection | 32 (64.0%) | 40 (43.5%) | 72 (50.7%) | 0.0985 |
| Subileus/ileus | 16 (32.0%) | 30 (32.6%) | 46 (32.4%) | 0.9583 |
| Icterus | 0 (0.0%) | 10 (10.9%) | 10 (7.0%) | 0.0873 |
| Abdominal pain | 0 (0.0%) | 30 (32.6%) | 30 (21.1%) | 0.0013 |
| Weight loss | 0 (0.0%) | 12 (26.1%) | 12 (16.9%) | 0.0051 |
| Abdominal compartment syndrome | 12 (24.0%) | 0 (0.0%) | 12 (8.5%) | 0.0005 |
Table 2: Endoscopic interventions are necessary for another indication’s.
Criteria for exclusion
• Patients who had pancreatic fluid collection along with acute pancreatitis other than ANC or WOPN were not included.
• Individuals with silent WOPN or ANC were also excluded.
• In addition, cases that were lost during the observation period were not included.
• Individuals with a history of persistent pancreatitis were excluded.
• Individuals who have already undergone pancreatic surgery were excluded.
• Individuals who received treatments for pancreatic necrosis other than endoscopic intervention were excluded.
• In cases where clinical improvement from draining collected purulent necrosis was not achieved, Direct Endoscopic Necrosectomy (DEN) was performed.
Vast regions of necrosis were assessed using the Single Transluminal Gateway Trans Cystic Multiple-Drainage (SGTMD) method. If the Single Transluminal Gateway method (SGT) proved ineffective and necrosis spread outside the smaller sac, Multiple Transluminal Gateway Technique (MTGT) were used in non-communicating necrosis collections. Additionally, laboratory testing, improved CT scans (ANC or WOPN), and physical examinations formed the basis of the retrospective management. Endoscopy was postponed until fluid in the WOPN developed, usually four weeks into the acute period. It was mostly applied to individuals who were in general good health and was performed in the early stages of ANC (before four weeks) (Group 1). Four weeks later, the WOPN wall (Group 2) was liquefied and the fluid was collected. Details of individual’s characters present in Table 1.
Drainage is the primary role of endoscopy in contaminated fluids, and can lead to organ damage, toxemia, and pressure complications. Signs of pressure were observed in the gastrointestinal tract, auxiliary organs, and bile ducts. A 20 mmHg increase in abdominal pressure can result in compartment syndrome. Endoscopic therapy is performed if an internal mass is present in the late stages of ANP associated with abdominal pain. This indicates that it was associated with other symptoms, as described in Table 2. However, endoscopic intervention alone is not recommended in pain management.
Early endoscopy is recommended before four weeks for Acute Necrotizing Pancreatitis (ANP) because of pressure symptoms, worsening toxemia, and lack of response to medical therapy. Abdominal pain and weight loss were associated with the mass and the effect of collection in the late phase of ANP, and were indicators of endoscopic treatment.
The type of endoscopic therapeutic algorithm
Those who had symptoms and necrotic accumulation, as shown by Endoscopic Ultrasound (EUS), underwent transmural drainage with a diameter of less than 30 mm³ across the gut and collection boundary. Prompt Endoscopic Necrosectomy (PEN) is recommended when the patient's condition does not improve after the removal of septic necrosis. A significant volume of material and fluid was drained through a single transluminal gateway using a Single Transluminal Gateway Trans cystic Multiple Drain (SGTMD). Multiple Transluminal Gateway Techniques (MTGT) have been used to treat numerous non-communicating forms of necrosis when Single Transluminal Gateway Procedures (SGT) demonstrate inadequate drainage.
Endoscopic therapy: Endotracheal intubation was performed under general anesthesia during the endoscopic procedures. All the patients agreed to undergo the procedure. All endoscopic procedures were performed using an Olympus GIF-H185 gastro scope (USA) equipped with a carbon dioxide insufflation system. All the patients underwent endoscopic therapy performed by the same specialist. A previous round of prophylactic antimicrobial drugs was administered to all participants along with blood testing, biopsies, and culture swabs.
Single-Gateway Transluminal (SGT 24): The fistulas were successfully created using EUS. Enter ostomy was subsequently performed using a Cystotome (CST-10; Cook Endoscopy). The opening across the intestinal wall and the accumulation of necrosis were found and expanded using a 15-mm inflated balloon (Cook Endoscopy or Boston Scientific). Olympus manufactures a transmural Lumen-Apposing Metal Stent (LAMS) that is 30 mm or 40 mm long and 16 mm in diameter. A 7-Fr or 8-Fr dual helical endoscopic stent with a 7-Fr or 8.5-Fr nasal drain (Cook Endoscopy) has replaced LAMS.
Multiple Translucent Gateway Technologies is what MTGT
stands for: A cooking endoscopy enter ostomy was performed using A CST-10 Cystotome. Cook Endoscopic or Boston Technical a 15-mm-higher was used to enlarge the space between the collected liquid and the next gutter. Between collecting and gut, there is another transmural track for indicated cases.
Trans cystic Multiple Drainage (SGTMD) is a single transluminal gateway: The patients who met the eligibility criteria for SGTMD underwent additional endoscopic procedures [20-22]. The guidewire was inserted into the cavity through the abscess reservoir and gut material, while being monitored by fluoroscopy throughout the abscess sub cavity. Under endoscopy and fluoroscopy supervision, a Boston Scientific 8-mm high-pressure balloon was used to enlarge the canals that divided the necrotic sub cavities (Figure 1). Next, a second 7-Fr or 8-Fr nasal drain and 7-Fr or 8.5-Fr two-pigtail stents were inserted via adjacent channels using Cook endoscopy with one end still inside the sub cavity.
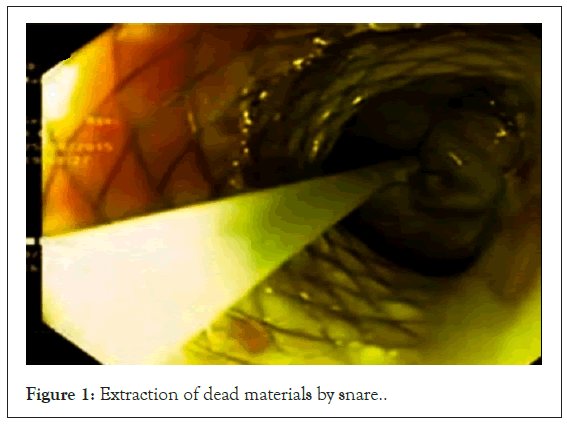
Figure 1: Extraction of dead materials by snare.
Endoscopic Direct Necrosectomy (DEN): The nasal drain was removed using transmural stents before insertion of the gastro scope into the channel [15]. Subsequently, the specimens were cleaned to remove any residual debris. In a straight endoscopic condition, dead tissue was removed with a 15-20 mm extraction balloon and a dormia basket (Cook Endoscopy or Olympus). This process was repeated multiple times for each necrosectomy procedure. A second pigtail stent and transmurally directed nasal drain were used to remove the ischemic material (Figures 2 and 3).
Figure 2: After completion of necrotic debris excision.
Figure 3: Transmural endoscopic evacuation through acute necrosis accumulation of a wall formed through fluoroscopy.
Drainage: For the next 48 hr. Every two hours (Figure 4, shows retraction and rotation after six months), and for the next seven days of active irrigation [22]. Normal saline (60-200 ml) was used for intranasal drainage at intervals of 4-6 hours to drain necrotic build-ups. If there were signs or symptoms of ANC or WOPN with pus discharge, the antibiotic was continued. However, necrotic collection material was sent for a second swap culture.
Figure 4: CT showing regression of collection 6 months.
Monitoring: Using abdominal ultrasonography, the size of the necrotic collection was examined every seven days [22]. Abdominal CECT was performed to confirm remission or to treat patients whose condition deteriorated despite treatment. The duration of active drainage was defined as the time from insertion of the nasal drain to its removal. After achieving clinical success, functional drainage was stopped (Figure 5). The CT results are (Figures 6).
Figure 5: Extensive and extensive pancreatic collection.
Figure 6: CECT scans with added contrast were used to examine acute necrotic collections that were treated endoscopically. An arrow indicates a portion of the collection with a wall, while an arrowhead indicates a portion without a wall. Note: A: Partially thick wall; B: A thick full wall; C: Partially thick wall; D: Partially thin wall.
Defined terms: Complications were classified as early (occurring up to 30 days after treatment) or late (occurring>30 days after treatment) [22]. The absence of symptoms related to collection and complete regression of the collection or a collection diameter of less than 40 mm on imaging was considered a clinical success. When active drainage was stopped and the collection completely regressed or had a diameter of less than 40 mm after one year of follow-up, it was considered a long-term success. Recurrence of a collection was defined as a size greater than 40 mm or recurrence of symptoms during follow-up.
The study of the data: Version 12.0 of the Statistician Programme Inc. Data visualization software system (2014, STATISTICA, Tulsa, Oklahoma, USA) was used for the experiment. The average, Standard Error of the Mean (SEM), average range, and 95% Confidence Intervals (95% CIs) were used in the quantitative analysis. Percentages and numerical styles were used to present subjective data. The symmetry of the ranges was confirmed using the Shapiro-Wilk test. The Brown-Forsythe test, also known as the dispersion hypothesis, was confirmed using Levene's test. Depending on the situation, the Student's t-test, Welch test for non-uniform variability, or Mann-Whitney U test was used to analyze the differences and similarities between the two groups. Qualitative variables, including Cochran's analyses, Fisher's test, and Yates adjustment for cells with less than ten, were analyzed using the chi-squared test.
Endoscopic methodology: In all the cases, the accumulated pus was removed via. endoscopic evacuation (Trans gastric, n=140; Trans duodenal, n=2). Despite lack of further use, maintenance monotherapy was administered. For example, minimal SGT was used in 40% and 67.4% of the cases, MTGT in 36% and 17.4%, and SGTMD in 24% and 15.2% of the cases, respectively (p=0.0770). Twenty-eight (30.43%) and forty-two (86%) patients in groups 1 and 2, respectively, underwent DEN (p=0.0001) (Table 3).
| The parameter in blood test | ANC (n=50) | WOPN (n=92) | p-value |
|---|---|---|---|
| Hemoglobin g/dl mean, (SD) [range] | 12.6 (3.1) [8.3-18.4] | 13.8 (2.80) [8.6-17.7] | 0.144 |
| Leukocytes,mm3, mean, (SD) [range] | 18.5 (6.8) [7.7-32.08] | 13.09 (7.2) [6.1-31.01] | 0.008 |
| Thrombocytes,mm3, mean, (SD) [range] | 489.1 (133.8) [154.0-553.0] | 292.9 (125.9) [110.0-555.0] | 0.013 |
| C-reactive protein,mg/L, mean, (SD) [range] | 225.7 (110.6) [58.8- 444.2] | 252.8 (105) [49.9-504.6] | 0.2 |
| Procalcitonin, µg/L, mean, (SD) [range] | 3.65 (5.2) [0.09-23.4] | 2.21 (3.5) [0.05-13.5] | 0.185 |
| Creatinine, mg/dl, mean, (SD) [range] | 2.0 (0.9) [0.8-2.6] | 1.8 (0.8) [0.8-2.8] | 0.052 |
| Amylase, U/L | 139.8 (119.4) [30-590] | 109.7 (76.8) [23-334] | 0.23 |
| Lipase, U/L | 117.9 (41.4) [51-222] | 82.5 (35.7) [23-166] | 0.015 |
| Bilirubin,mg/dl, mean, (SD) [range] | 2.3 (3.0) [0.4-13.6] | 1.9 (2.3) [0.5-10.0] | 0.204 |
| AST U/L, mean, (SD) [range] | 226.7 (230.6) [45-1105] | 230 (184.4) [34-652] | 0.812 |
| ALT U/L, mean, (SD) [range] | 218.9 (213.4) [51-1015] | 253.9 (205.2) [34-782] | 0.623 |
| D-dimer, mg/L | 1.28 (0.9) [0.39-4.6] | 0.96 (0.7) [0.5-3.55] | 0.731 |
Table 3: Results of blood tests on day of starting endoscopy.
Duration and efficacy of treatment: Complete elimination typically took 26.8 (15-56) days in Group 1 and 16.9 (4-47) days in Group 2 (p=0.0001). The average number of endoscopic attempts was 4.5 (2-10) in Group 2 (p=0.0001) compared to 9.5 (4-15) in Group 1. In Group 1, the average surgery time was 270.8 (146- 383) days, while in Group 2, it was 164.2 (28-412) days (p=0.0001).
In Group 2, pain was reduced in forty-six patients (92%) and in eighty-eight cases (95.7%) patients, respectively (p=0.5238).
Early difficulties: Endoscopic-related problems were observed in group 2 (22 [23.8%]) but not in group 1 (14 [28%]). (p=0.7054). None of the patients required any treatment. The challenges associated with the endoscopic symptoms and early indicators of pancreatic necrotic collection are presented in Table 4.
| Methods | ANC (n=50) | WOPN (n=92) | Total (n=142) |
|---|---|---|---|
| Complication (method of complication treatment) | |||
| Hemorrhage needs transfusion | 8 (16.0%) | 12 (13.04%) | 20 (14.08%) |
| Loss of the stents removed endoscopically | 6 (12.0%) | 8 (8.7%) | 14 (9.86%) |
| Perforated wall need conservative treatment | 0 (0.0%) | 2 (2.17%) | 2 (1.4%) |
Table 4: Reported Difficulties of endoscopic symptoms and early indicators of pancreatic necrotic.
Fatality: The overall death rate was 4.3% (2/46) in the first group and 4.3% (1/25) in the second group (p=0.9445). Multiple organ failure due to ANP is a cause of death.
Extended success: The average interval between consecutive appointments was 14 months (Range: 10-20 months). After the first few months of the inquiry, one person passed away.
Sustained success: 72 participants in the second group (84.8%) compared to 42% participants in the first group (84%) (p=0.9306); recurrent collection occurred in 12 patients (12% in Group 1) and 13% participants in category 2 (p=0.9000). Drainage was performed each time.
Late challenges: After therapy, 28 (31.11%) patients in the second group and 14 (28%) in the first group were compared (p=0.8947). There were ten (20%) and 40 (43.5%) splenic and portal vein emboli in Groups 1 and 2, respectively (p=0.0479). Dependence of treatment outcomes on the timing of endotherapy initiate.
The negative significant findings were: The frequency of endoscopic drainage (R=-0.51, p=0.003), overall duration of endoscopic therapy (R=-0.87, p=0.0001), and interval between the start of ANP and current endoscopic evacuation (R=-0.80, p=0.0001).
WON subgroup's results
Thirty-nine initial treatment participants were included in the information research for the early treatment timing of patients to WON controls (19 matched cases and 19 controlled cases for early intervention). Clinical characteristics and demographic data are shown in Table 5. In all 19 cases of timely therapy, pancreatic and peripancreatic tissue necrosis was visible on CECT (Figure 6). The most common reason for treatment was infection; no patient received rapid care for pain alone. Five of the 11 patients who required rapid treatment were hospitalized during their index operation, and all required Intensive Care Unit (ICU)-level care during their stay. However, two of the late-response controls required treatment in the intensive care unit, and two of them were present during their index operation. Patients receiving initial treatment were less likely than those receiving later treatment to have a full wall at the start of the first treatment (8 of 19 vs. 17 of 19), P.C.01 (by unconditional logistic regression).
| Contents | Early intervention cases (n=19) | Late intervention controls (n=19) | p-value |
|---|---|---|---|
| Age (years), median (range) | 64 (21-79) | 56 (28-86) | 0.58 |
| Gender (female), n (%) | 6 (32) | 6 (32) | 1 |
| Body mass index (kg/m2), median (range) | 29.5 (20.7-43.0) | 27.4 (19.7-46.2) | 0.58 |
| History of previous pancreatitis, n (%) | 5 (26) | 2 (11) | 0.25 |
| Indications for intervention, n (%) | |||
| Infection | 13 (68) | 13 (68) | 1 |
| Pain | 9 (47) | 12 (63) | 0.17 |
| Gastric outlet obstruction | 0 (0) | 1 (5) | 0.37 |
| Nausea and vomiting | 5 (26) | 4 (21) | 0.57 |
| Enlarging collection | 6 (32) | 4 (21) | 0.41 |
| Bleeding in cyst | 2 (11) | 2 (11) | 1 |
| GI bleeding | 1 (5) | 0 (0) | 0.37 |
| Cause of pancreatitis, n (%) | |||
| Gallstone | 8 (42) | 10 (53) | 0.32 |
| Alcohol | 0 (0) | 1 (5) | |
| Post-ERCP | 2 (11) | 0 (0) | |
| Unknown or other causes | 9 (47) | 8 (42) | |
| Size of the collection (cm), median (range) | 16 (7-24) | 15 (5-22) | 0.021 |
| Collection age at time of intervention (days), median (range) | 23 (15-27) | 64 (32-2747) | |
| Wall characteristics | |||
| Thick wall, n | 17 | 18 | 0.57 |
| Thin wall, n | 2 | 1 | |
| Collection wall completeness on CT, n | |||
| Full | 8 | 17 | <0.01 |
| Partial | 11 | 2 | |
| Collection wall at drainage site, n | |||
| Thick | 14 | 18 | 0.032 |
| Thin | 5 | 0 | |
| None | 1 | ||
| Air in collection before intervention, n (%) | 2 (11) | 7 (37) | 0.049 |
| Fat in collection before intervention, n (%) | 17 (89) | 12 (63) | 0.093 |
| Number of initial endoscopic drainage sites, n (%) | |||
| One drainage site | 13 (68) | 18 (95) | 0.014 |
| Two drainage sites | 6 (32) | 1 (5) | |
| Location of drainage, n (%) | |||
| Transgastric | 8 (42) | 15 (79) | 0.038 |
| Transduodenal | 6 (32) | 3 (16) | |
| Both | 5 (26) | 1 (5) | |
Table 5: Lists the clinical and imaging characteristics of the 19 early intervention patients who were walled off and had endoscopic intervention.
Patient characteristics
Overall, 142 consecutive patients with ANP were enrolled, of which 59% were men with a mean age of 49.9 (interquartile range: 22-79) years. Groups 2, 92 patients, and 50 were assigned to Group 1. Necrotic specimens and patient features are presented in Table 1. The administration techniques are presented in Table 2. In the second group, 45.65% of patients met several criteria for transmural endoscopic evacuation and repeated necrosectomies inside a well- formed wall (Figures 2 and 3). The CT contrast showed collection and regression after debris removal (Figures 4 and 5). In Group 1 (ANC), the average time from the start of the episode to endoscopy was 16.4 (8-25) for 50 patients (35.21%). For the 90 patients in the second set of WOPN instances, the average time from the start of the episode to surgery was 74.5 (30-240) days. In Groups 1 and 2, 32 (64%) and 40 (43.5%) cases of infected pus required endoscopy, respectively (p=0.0985). The most common bacteria found in necrotic pus were pneumonia, Enterococcus faecalis, Klebsiella, Escherichia coli, and Staphylococcus epidermidis.
Endoscopic methodology: In all the cases, the accumulated pus was removed via endoscopic evacuation (transgastric, n=140; transduodenal, n=2). Despite lack of further use, maintenance monotherapy was administered. For example, minimal SGT was used in 40% and 67.4% of the cases, MTGT in 36% and 17.4%, and SGTMD in 24% and 15.2% of the cases, respectively (p=0.0770). Twenty-eight (30.43%) and forty-two (86%) patients in Groups 1 and 2, respectively, underwent DEN (p=0.0001).
Duration and efficacy of treatment: Complete elimination typically took 26.8 (15-56) days in Group 1 and 16.9 (4-47) days in Group 2 (p=0.0001). The average number of endoscopic attempts was 4.5 (2-10) in Group 2 (p=0.0001) compared to 9.5 (4-15) in Group 1. In Group 1, the average surgery time was 270.8 (146- 383) days, while in Group 2, it was 164.2 (28-412) days (p=0.0001). In Group 2, pain was reduced in forty-six patients (92%) and in eighty-eight cases (95.7%) patients, respectively (p=0.5238).
Early difficulties: Endoscopic-related problems were observed in Group 2 (22 [23.8%]) but not in Group 1 (14 [28%]). (p=0.7054). None of the patients required any treatment. The challenges associated with the endoscopic symptoms and early indicators of pancreatic necrotic collection are presented in Table 4.
Fatality: The overall death rate was 4.3% (2/46) in the first group and 4.3% (1/25) in the second group (p=0.9445). Multiple organ failure due to ANP is a cause of death.
Extended success: The average interval between consecutive appointments was 14 months (range: 10-20 months). After the first few months of the inquiry, one person passed away. Sustained success: 72% participants in the second group (84.8%) compared to 42 participants in the first group (84%) (p=0.9306); recurrent collection occurred in 12 patients (12% in Group 1) and 13 participants in category 2 (p=0.9000). Drainage was performed each time.
Late challenges: After therapy, 28 (31.11%) patients in the second group and 14 (28%) in the first group were compared (p=0.8947). There were ten (20%) and 40 (43.5%) splenic and portal vein emboli in groups 1 and 2, respectively (p=0.0479). Dependence of treatment outcomes on the timing of endotherapy initiate.
The negative significant findings were: The frequency of endoscopic drainage (R=-0.51, p=0.003), overall duration of endoscopic therapy (R=-0.87, p=0.0001), and interval between the start of ANP and current endoscopic evacuation (R=-0.80, p=0.0001).
WON subgroup's results
Also known as the ICU, only 16 control cases were included in the evaluation due to incomplete results. The initial endoscopic operation was performed during the inpatient phase. Unfortunately, two patients identified in the initial therapy cases were excluded because they did not meet the eligibility criteria. Consequently, they were left to be monitored, which meant that it would never have been possible to determine whether their illnesses had improved. In contrast to the average of 22 days for those with a positive result (range,15-27 days), the collection days for these two cases were 26 and 28 days, respectively. Additionally, unlike the 19 patients who showed outstanding results, these two individuals had an entire wall on CECT (Table 6). Twenty-six days after the onset of symptoms, the first patient lost to further assessment required invasive radiology-guided evacuation for an infection in the left liposcopy muscle caused by a damaged pancreatic duct following transgastric endoscopic therapy for a 16 cm collection. After four endoscopic procedures (necrosectomy, further irrigation, and stent extraction), the patient failed to undergo surveillance. During the most recent monitoring visit, the patient experienced sporadic abdominal pain, and imaging showed intrapancreatic fluid accumulation of 4.8 × 3.5 cm. The second patient, who was lost to further detail, underwent endoscopic therapy, and a 16-cm accumulation was observed 28 days after symptom onset. During the patient's post-hospital monitoring visit, the clinical symptoms subsided, with the exception of a few mild occurrences of loose stool 2-3 times per day. Nevertheless, because radiology monitoring could not be performed, no broad conclusions regarding the effectiveness of the procedure could be drawn by the radiologist.
| Detection Technique | Early intervention cases (n=19) | Late intervention controls (n = 19) | p- value |
|---|---|---|---|
| Endoscopic necrosectomy during index intervention | 11 (58) | 15 (79) | 0.15 |
| Total number of endoscopic necrosectomy sessions, median (range) | 4 (1-9) | 3 (1-11) | 0.71 |
| Subsequent percutaneous drainage required | 3 (16) | 4 (21) | 0.66 |
| Type of stents placed during index procedure | |||
| Plastic | 9 (47) | 10 (53) | 0.18 |
| LAM stent (Axios) | 2 (11) | 6 (32) | 0.18 |
| Other metal stent (Niti-S, Alimaxx-ES) | 2 (11) | 0 (0) | 0.18 |
| Plastic and LAM stent | 6 (32) | 2 (11) | 0.18 |
| None | 0 (0) | 1 (5) | 0.18 |
| Mention of disrupted/disconnected duct on imaging or ERCP | 9 (47) | 8 (42) | 0.78 |
| Pancreatic stent placement for disrupted/disconnected duct | 3 (16) | 3 (16) | 1 |
| Drainage stents left in place for disconnected/disrupted duct | 0 (0) | 1 (5) | 0.37 |
| Distal pancreatectomy for disconnected/disrupted duct | 1 (5) | 2 (11) | 0.57 |
Table 6: Lists the procedure details for the 19 patients who underwent matching walled-off endoscopic intervention and early intervention.
In the ICU, only 16 control cases were included in the evaluation due to incomplete results (Table 7). The initial endoscopic operation was performed during the inpatient phase. Unfortunately, two patients identified in the initial therapy cases were excluded because they did not meet the eligibility criteria. Consequently, they were left to be monitored, which meant that it would never have been possible to determine whether their illnesses had improved. In contrast to the average of 22 days for those with a positive result (range,15-27 days), the collection days for these two cases were 26 and 28 days, respectively. Additionally, unlike the 19 patients who showed outstanding results, these two individuals had an entire wall on CECT. Twenty-six days after the onset of symptoms, the first patient lost to further assessment required invasive radiology-guided evacuation for an infection in the left liposcopy muscle caused by a damaged pancreatic duct following transgastric endoscopic therapy for a 16-cm collection. After four endoscopic procedures (necrosectomy, further irrigation, and stent extraction), the patient failed to undergo surveillance. During the most recent monitoring visit, the patient experienced sporadic abdominal pain, and imaging showed intrapancreatic fluid accumulation of 4.8 × 3.5 cm. The second patient, who was lost to further detail, underwent endoscopic therapy, and a 16-cm accumulation was observed 28 days after symptom onset. During the patient's post-hospital monitoring visit, the clinical symptoms subsided, with the exception of a few mild occurrences of loose stool 2-3 times per day. Nevertheless, because radiology monitoring could not be performed, no broad conclusions regarding the effectiveness of the procedure could be drawn by the radiologist. contrast to the average of 22 days for those with a positive result (range,15-27 days), the collection days for these two cases were 26 and 28 days, respectively. Additionally, unlike the 19 patients who showed outstanding results, these two individuals had an entire wall on CECT. Twenty-six days after the onset of symptoms, the first patient lost to further assessment required invasive radiology- guided evacuation for an infection in the left liposcopy muscle caused by a damaged pancreatic duct following transgastric endoscopic therapy for a 16-cm collection. After four endoscopic procedures (necrosectomy, further irrigation, and stent extraction), the patient failed to undergo surveillance. During the most recent monitoring visit, the patient experienced sporadic abdominal pain, and imaging showed intrapancreatic fluid accumulation of 4.8 × 3.5 cm. The second patient, who was lost to further detail, underwent endoscopic therapy, and a 16 cm accumulation was observed 28 days after symptom onset. During the patient's post- hospital monitoring visit, the clinical symptoms subsided, with the exception of a few mild occurrences of loose stool 2-3 times per day. Nevertheless, because radiology monitoring could not be performed, no broad conclusions regarding the effectiveness of the procedure could be drawn by the radiologist.
| Time period | Early intervention cases (n=19) | Late intervention controls (n=19) | p- value |
|---|---|---|---|
| Resolution of symptoms | 17 (89) | 17 (89) | 1 |
| Resolution of the collection on cross-sectional imaging studies | 19 (100) | 18 (95) | 0.37 |
| Primary outcome achieved | 19 (100) | 18 (95) | 0.37 |
| Time from initial procedure to removal of all stents and drains (days), median (range) | 103 (44-422), n=18 | 69 (27-330), n=17 | 0.042 |
| Patients requiring surgery before stent removal | 1 (5) | 0 (0) | 0.37 |
| Length of hospital stay | 26 (6-44) | 6 (0-40) | <0.01 |
| (days), median (range) | |||
| Number of ICU days | 1 (0-22) | 0 (0-6) | <0.01 |
| (days), median (range) | |||
| Number of ICU days before index intervention (days), median (range) | 1 (0-18) | 0 (0-4) | <0.01 |
| Number of ICU days after index intervention (days), median (range) | 0 (0-21) | 0 (0-2) | 0.092 |
| Requiring ICU care at the time of index intervention | 5 (26) | 1 (5) | 0.093 |
| Patients experiencing adverse events likely related to endoscopic intervention | 4 (21) | 6 (32) | 0.41 |
| Stent migration | 2 (11) | 4 (21) | 0.15 |
| Stent occlusion | 2 (11) | 2 (11) | 1 |
| Hemorrhage | 1 (5) | 3 (16) | 0.32 |
| Aspiration pneumonitis | 1 (5) | 0 (0) | 0.37 |
| Patients experiencing adverse events likely not related to endoscopic intervention | 5 (26) | 8 (42) | 0.36 |
| New diabetes mellitus | 2 (11) | 1 (5) | 0.57 |
| Venous thrombosis (portal/splenic/superior mesenteric vein) | 4 (21) | 5 (26) | 0.71 |
| New varices (gastric or esophageal) | 0 (0) | 5 (26) | 0.014 |
| Mortality (1 year) | 0 (0) | 1 (5) | 0.37 |
Table 7: Outcomes of endoscopic intervention for the 19 patients with early intervention and matched walled-off necrosis controls. Note: Values are expressed as percentages (%) unless otherwise noted.
The current guidelines for addressing ANP advocate delaying endoscopic therapies for necrosis accumulation for at least four weeks after the sickness begins [1,6-9,11,15]. Early on in ANP, injections of antibiotics and supportive medical therapy should be administered [16,17]. More information is needed to determine the benefits of endoscopic evacuation during the first four weeks of ANP [11-14,1]. To execute surgical intervention, the step-up method combines percutaneous drainage with Trans peritoneal or retroperitoneal access [10-20]. Compared to exterior (percutaneous) evacuation, interior (endoscopic) evacuation lowers the risk of infection and cannot result in a pancreatic cutaneous fistula. However, with percutaneous accessibility and a less invasive method (local anesthesia), evacuation is still feasible regardless of the location of the necrosis buildup, particularly in severely ill patients who are not suited for anesthesia [10]. In the current experiment, endoscopic draining proved more effective than percutaneous evacuation. Early pancreatic necrosis after percutaneous drainage entails a more extended treatment duration and frequent exfoliation to remove solid components from the dissolved sac. When fluid is removed percutaneously, transmural endoscopic procedures are more effective if they are not accessible. Transmural irrigation and early percutaneous endoscopy also make it possible to remove suppuration and dead tissue effectively. These are all very important for managing pancreatic necrosis. The window for endoscopic treatments gets smaller when endoscopic evacuation is put off until WOPN forms. Creative surgical methods, like endoscopic clearance and necrosectomy, have been used. Nonetheless, in certain situations where surgery is required in the early stages of APN, endoscopy for ANCs should be performed effectively and safely. Contrary to popular belief, endoscopy can occur four weeks after ANP. It is possible to prevent the need for therapy for ANP by performing early active endoscopic operations. If endoscopic evacuation is unsuccessful, more therapeutically regulated intrusive treatment alternatives may be used by the endoscopic step-up strategy. Unlike endoscopic therapy for WOPN, the results suggest that various endoscopic techniques, treatments, and extensive surgical operations are required. A history of issues and lowered security surrounds more than 40% of the solid materials used in endoscopy. Careful record-keeping is crucial, according to Rana et al. This experiment had no potentially adverse treatment effects because endoscopy for WOPN and ANP was equally safe and effective. Transmural pus evacuation has a higher chance of success when transmural implantation of LAMS results in a more extensive fistula. In our trial, LAMS was administered during therapy to patients who were ANP or WOPN and had a risk of pus reaccumulation. The most dangerous side effects of endoscopy are constipation and perforations, which happen when pancreaticocutaneous or pancreaticogastro fistulas don't work out (usually because the stent moves through the muscle). Two scientists looked into the benefits of using an endoscopic technique for ANP with the first ANP. Trikudanathan, et al [13]. Identified an irregular population of 305 ANP individuals as a result of treatment. It is incredibly challenging to compare these results with the findings of the current investigation because, until recently, endoscopic evacuation was thought to be the only option for treating necrosis accumulation. Better results have been linked to a reduced length of hospital stay, fewer patients requiring emergency surgery, and a less invasive step-up procedure when using WOPN therapies. The anticipated advantage of early catheter drainage (step-up) in patients with necrotizing pancreatitis who were infected was not demonstrated by the current experiment. In this study, very few surgeries for septic necrosis were performed, and more than one- third of patients received conservative care when a delayed drainage technique combined with antibiotic treatment was used. The makers of Hot-Spaxus and Hot-Axios are Boston Scientific in Massachusetts, USA, and Gimpo in Korea, Taewoong Medical. EUS-guided endoscopic necrosectomy Lumen-Apposing Metal Stent (EC-LAMS) is now available for various treatments. They are currently available for many EUS-guided surgeries. Using EC- LAMS microspheres in our study may have improved the efficacy of both early and late ET. The newest research on this method shows that the new EC-LAMS is more specific, competent, and compelling at endoscopic transmural drainage of both peripancreatic and post- pancreatic collections. It is currently unclear how precisely the wall thickness determined during surgery using EUS and CECT imaging relates to one another. Noninvasive, contrast-enhanced imaging may or may not show the wall around the necrosis. This suggests that there is more room for development in imaging technology than an issue with how radiologists or endoscopic interventionists interpret these images=-23. Trikudanathan, et al [13]. Experimented to record the outcomes of early endoscopic surgery for necrosis. A retrospective study of prospective instances is reported for the first time, accurately matching longer and newer sequences with the best treatment time. The interval between the emergence of pancreatic indications and the start of early therapy was not documented. Many patients, including those who underwent their first interventional evacuation, were assessed. We found that the group receiving the first endoscopic procedure had longer therapy durations and longer stays in the Intensive Care Unit (ICU) than the WON control group. Furthermore, compared to patients treated for WON, their rates of hospitalization, ICU stay, catheter drainage (42% vs. 21%), surgery (7% vs. 1%), and death (19% vs. 5%) were significantly higher. Our investigation demonstrated the safety and efficacy of an endoscopic treatment for necrotic accumulations as early as 15 days after pancreatitis onset. Additionally, it proved the use of plastic and metal stents for Trans duodenal and Trans gastric irrigation without the need for prior percutaneous draining, and it developed several locations for drainage systems. Furthermore, we saw a propensity for fewer adverse outcomes to happen following early endoscopic therapy as compared to controls for subsequent interventions; nevertheless, we did not see an increase in mortality, ER visits, or catheter drainage. The accepted criteria for necrotic pancreatic collections are divided into two extremes: WONs, typically older than four weeks and surrounded by an established wall, and ANCs, younger than four weeks and do not have a wall [2,3]. Eventually, ANC turns into WON, and physicians often handle specimens that don't fit into either category. Our findings show that 49%, 37%, and 7% of the cases treated with rapid endoscopy had an incomplete accumulation. This means that there was a clear, smoother border between the collected tissue and nearby tissue that held 20% to 80% of the collection. We believe that individuals in the partially walled group need a cautious endoscopic procedure to reduce the possibility of guidewires or necrosectomy equipment entering the septic collection. Despite these drawbacks, our data suggest early endoscopic intervention is a workable therapeutic approach. Most of the prospective trial participants had illnesses that were not well treated with antibacterial medications, necessitating emergency medical intervention. The need for intensive care unit care indicated the condition was more severe. Yet, despite this, we found that early endoscopic therapy had fewer cumulative adverse outcomes than future treatment. We acknowledge that the early- intervention patients' and the late-intervention controls' ages, sexes, collection sizes, and underlying diagnoses were prospectively matched. Conversely, air was more frequently observed in patients with late activity, indicating that the intestinal fistulization had already occurred. However [19], states that this difference was not statistically significant. The small number of patients lost to follow- up may have contributed to the adverse events observed in the initial therapy group. One advantage of this study is that a co- investigator in radiography, blind to the case or control status, appropriately analyzed Computed Tomography (CT) examination data using preset diagnostic parameters. It was incorrect to apply our WON subgroup results to people whose collection was delayed during the early phases of their illness. Recommendations for necrotic pancreatic collections define two ends of a spectrum: WONs persist or are often longer than four weeks. At the same time, ANCs do not have a conspicuous wall and are younger than four weeks. The walls were developed enough to enclose the WONs entirely. Doctors periodically manage collections that don't fully fit into either group, and there is a gradual transition from ANC to WON. For patients receiving initial endoscopic therapy, Trikudanathan, et al [13]. Report that "some," "extensive," or "full wall growth" was observed in 49%, 37%, and 7% of cases, respectively. The radiological criteria did not describe the collecting wall's size, condition, or fullness, nor did they present a randomized contrast between the cases and controls. The presence, thickness, and fullness of the whole wall were accurately and consistently described by imaging, and the research clinician was kept in the dark about the case/control status. Most of the patients we treated and who received early care had a partial collection wall, according to CT scans. This wall, which separates the collected area from the surrounding tissue, encloses 20%-80% of the site and is smooth and unambiguous. If validated, these standards could help physicians weigh the advantages and disadvantages of early endoscopic management of symptomatic pancreatic necrosis. The main drawbacks of this study are its small sample size and comparison methodology, which came about as a result of our careful selection of patients who required endoscopic surgery shortly after due to necrotic accumulation. The fact that highly skilled endoscopists performed the treatments for pancreatic necrosis at a single site might have impacted the trial's efficacy. The small number of patients in the earlier therapy group who did not respond to follow-up may have contributed to the unfavorable events we recorded in this cohort. One advantage of this study is that the co-investigator, a radiologist, thoroughly reviewed the CT scan data using predetermined imaging criteria while remaining blind to the case or control condition. Also, patients with insufficient collection walls need careful endoscopic procedures to lower the chance that necrosectomy instruments or guidewires will be used for necrotic collection. Our findings imply that early endoscopic intervention is a manageable strategy with outcomes comparable to late intervention in an adequately chosen patient population. The air was more frequently observed in late intervention patients, suggesting pre-existing gut fistulization, even though we compared early intervention cases and late intervention controls based on age, sex, collection size, and grounds for intervention. It's also possible that different groups had different additional variables, which would have obscured differences in the outcomes. However, all of the early intervention patients in the trial required emergency care; usually, this was because they had a suspected infectious illness that was challenging to treat with antibiotics alone. We discovered that early endoscopic intervention had fewer overall adverse outcomes than late intervention, even when the sickness necessitated treatment in an intensive care unit. Nevertheless, there was no statistically significant variation.
Limitations
Patients require early endoscopic intervention for necrotic collection. Moreover, our study may be biased toward positive results because highly skilled endoscopists performed these procedures at a single clinic specializing in treating pancreatic necrosis. The early intervention group saw a patient loss to follow-up, which would have affected the adverse event rates and cohort development previously mentioned. A radiology co-investigator who meticulously marked each case while remaining unaware of the case or control status strengthened our investigation. We discovered that early endoscopic intervention was associated with fewer overall adverse events than late intervention, even though the need for intensive care unit care suggested that the illness was more severe. However, because of the constraints of individual facilities and small sample sizes, this difference was not statistically significant. A further drawback is the high number of adverse effects that were observed during a prolonged period of observation. Compared to those who need surgery, the early stages of ANP are linked to decreased rates of morbidity and mortality.
According to our research, it is advisable to postpone starting endoscopic treatment for necrotizing pancreatitis until the material has dissolved and turned fluid. By avoiding surgery or other procedures, the endoscopic approach can aid in severe instances in the early stages of ANP, even in cases where WOPN develops. Early endoscopic intervention for pancreatic necrosis in the third and fourth weeks after the start of pancreatitis is safe and effective when there is a clinical reason to act quickly. Contrast Enhanced Computed Tomography (CECT) revealed a collection wall, either in whole or partially, supporting our findings. Our findings remained the same after the WON subgroup analysis.
The study was approved by Zagazig University Hospital and the Institutional Committee of Science and Research Ethics (ZUM/4097-5/2023). All experiments were performed in accordance with the relevant guidelines and regulations (such as the Declaration of Helsinki). As this retrospective cohort study was performed using an anonymous database, informed consent was waived by Zagazig University Hospital and the Institutional Committee of Science and Research Ethics (Zagazig University, Faculty of Medicine, Egypt).
All the data were reviewed and made available by the corresponding authors. All the authors approved, agreed to, and shared the database.
HAS, MF: Conception and design; MR, AB: Development of methodology; MR, AK: Acquisition of data; ME, KS: Analysis and interpretation of data; HAS, ME, and MF: Writing, review, and/or revision of the manuscript; HAS: Administrative, technical; HAS, MF, KS: Material support. All authors equally shared, agreed and approved the final manuscript.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Soliman AR, Baz A, Farid MI, Eraky ME, Riad M, Sharaf K, et al. (2024) Analyzing Endoscopic Treatment for Symptomatic Pancreatic Necrotic Collection Retrospectively: The Impact of Intervention Timing. Pancreat Disord Ther.14:311.
Received: 14-Jun-2024, Manuscript No. PDT-24-31017; Editor assigned: 17-Jun-2024, Pre QC No. PDT-24-31017 (PQ); Reviewed: 01-Jul-2024, QC No. PDT-24-31017; Revised: 08-Jul-2024, Manuscript No. PDT-24-31017; Published: 15-Jul-2024 , DOI: 10.35841/2165-7092.24.14.311
Copyright: © 2024 Soliman AR, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.