Journal of Women's Health Care
Open Access
ISSN: 2167-0420
ISSN: 2167-0420
Research - (2020)Volume 9, Issue 4
Background: Anemia affects almost two-thirds of pregnant women in developing countries and contributes to maternal morbidity and mortality and to low birth weight. Anemia during pregnancy is associated with negative maternal and neonatal outcomes. However, there is limited data regarding prevalence of anemia and its determinant factors during pregnancy in western Ethiopia.
Objective: To determine the prevalence of anemia and its determinants among pregnant women in Ebantu District, East Wollega zone, Ethiopia.
Material: A cross-sectional study was carried out among pregnant women. A total of 625 pregnant women were screened for hemoglobin level. The test was determined using hemocue screening technique. Weight and height was measured & other determinants of anemia during pregnancy were also assessed using a structured questionnaire.
Results: This study revealed that 23.7% of patients had mild anemia, and 11.9% had moderate and none with severe anemia. Multivariate analysis showed that birth interval less than or equal to two years adjusted odds ratio (95%CI):1.5(1.1, 2.9), a history of abortion adjusted odds ratio (95%CI):2.4(1.6, 3.6), having two or more abortions adjusted odds ratio (95%CI) 2.6(1.3, 6.2), illiteracy with crudes odds ratio (95%CI):2.974(1.5, 5.6) and AOR: 5.92(1.8,18.9) were significantly associated with anemia in pregnancy.
Conclusions: The major determinants of anemia in pregnancy are illiteracy, short birth spaces less than or equal to two, history of abortion and lack of Iron supplementation while pregnant.
Content: The major determinants of anemia in pregnancy are illiteracy, short birth spaces less than or equal to two, history of abortion and lack of Iron supplementation while pregnant.
Anemia; Ebantu; Pregnant women; East Wollega; Determinant factors
ANC: Antenatal Care; PW: Pregnant Women; WHO: World Health Organization
Anemia is defined as a reduction in the oxygen-carrying capacity of the blood as a result of fewer circulating erythrocytes than normal or a decrease in the concentration of hemoglobin [1]. Anemia usually occurred as in non-pregnant women <12 g/dl and pregnant females <11 g/dl. Severe anemia has been defined as <7g/dl [2].
Anemia may result from defects at any stage of red cell and hemoglobin production or when an increased rate of red cell destruction (hemolysis) exceeds the capacity of the bone marrow to mount a compensatory increase in production. Changes in the relationship between red blood cell count and plasma volume may also result in a reduced hemoglobin concentration. Such changes occur physiologically in pregnancy where red blood cell volume is increased less markedly than plasma volume [3].
Anemia is one of the most common nutritional deficiency diseases observed globally. Although nutritional anemia affects members of both sexes and all age groups, the problem is more prevalent among women and contributes to maternal morbidity and mortality, as well as to low birth weight [4].
It was estimated that nutritional anemia affects almost two-thirds of pregnant women (PW) in developing countries with an estimated prevalence of anemia of almost 50% among non-pregnant women [5]. In Ethiopia, prevalence of anemia among pregnant women was 51.9% [6]. A study conducted around Gilgel Gibe Dam revealed prevalence of anemia in PW is 53.5% [7]. Study showed that residence, income, educational level, breastfeeding and high parity were significant predictors to anemia [8].
Worldwide, anemia is a common public health problem. The highest incidence of it is reported in South Asia and Sub-Saharan Africa. It is agreed that nutritional deficiency, due primarily to low bio-availability of dietary iron, accounts for more than half the total numbers of cases. The two major groups at risk are children and pregnant women [9].
Globally, anemia has been found to be the most common complication in pregnancy. The World Health Organization (WHO) estimates that more than 40% of non-pregnant and over 50% of pregnant women in developing countries are affected. The World Bank ranked anemia as the 8th leading cause of disease in girls and women in the developing world. Apart from maternal morbidity and mortality, neonatal mortality is high among the babies of anemic mothers [10].
Iron deficiency anemia in pregnancy is a risk factor for preterm delivery and subsequent low birth weight and possibly for inferior neonatal health. It is the third leading cause of disability-adjusted life years lost for females aged 15-44 year [11]. Anemia during pregnancy is associated with an increased risk of intrauterine growth retardation, premature delivery and low birth weight, resulting in an increase in prenatal mortality. Anemia is directly responsible for 20% of maternal death and is an associated cause in another 20% [12].
In Ethiopia, there are limited studies that had been shown the relationship of determinant factors with anemia. Besides, in Ebantu district, western Ethiopia, there are no previous studies on the associations between anemia and its determinant factors among pregnant PW. However, according to clinical reports of the Health Centers in this district, anemia is currently listed as the first reason why pregnant women visit health facilities. Therefore, the present study was undertaken to investigate the prevalence of anemia and its risk factors among PW.
Study design
A community based cross-sectional study was conducted (Figure 1).
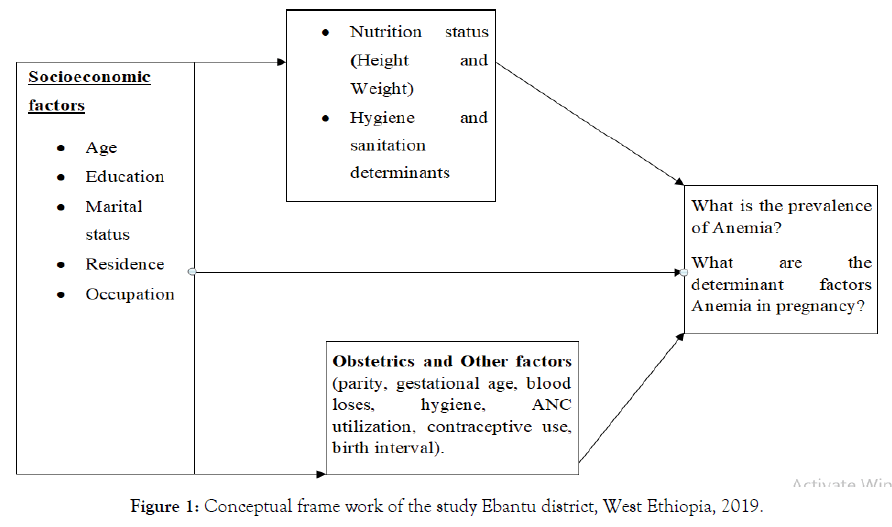
Figure 1. Conceptual frame work of the study Ebantu district, West Ethiopia, 2019.
Study area and period
Ebantu district is located in East Wollega zone and far away 145 km from Nekemte town which is the zone capital. It has a total population of 43,739, and 1,750 PW. This district has 2 governmental health center and 20 health post. It is situated at an altitude greater than 1000 meters above sea level and has tropical and sub-tropical types of climate. The mean annual temperature ranges between 21°C and 24°C. It has a total area of 920 square Kilometers. It is bounded by Gida Ayana district in the East, Benshangul Gumuz regional state and Haro Limmu district in the west, and Blue Nile River in the north and Limu district in the south. This study was conducted from March to April, 2019.
Source population
All pregnant women in Ebantu district.
Study population
All confirmed PW by health professionals and made at least one visit to health post or health center for ANC services.
Sample size
The required sample size for this study was calculated based on the following assumptions:
Prevalence (P) of anemia among women 15-49 years, 50% was taken due to absence of previous study in the area.
Design effect=1.5
95%CI, and 5% margin of error(d) adding 10% allowance for possible non-response; n=633
Sampling procedure
Two-stage sampling was employed to select the household. From total of 20 kebeles [the lowest administrative unit in Ethiopia] in the district, 16 kebeles were selected by using simple random sampling techniques. All PW in randomly selected kebeles were screened and registered by trained Health extension workers (HEW) in their respective Kebeles by conducting house to house visit. All households with eligible participants were registered and code number was given for them sequentially at the district level. Then, for each kebele the sample was proportionally allocated. A systematic random sampling technique was employed and PW who met the inclusion criteria during the study period were approached until the required sample size was fulfilled.
Inclusion criteria
Residents in the study area and who gave consent to participate were involved.
Exclusion criteria
Those participants who were severely sick and unable to speak were excluded.
Data collection procedure
Information on socioeconomic characteristics, obstetric and others factors were collected by using structured and pre-tested questionnaire. First, the questionnaire was developed in English and then translated to Afaan Oromo (the regional language) during the interview and then back to English language by two language teachers. Two medical laboratory technicians who can speak Afaan Oromo were trained on data collection procedures and conducted the data collection. A pre-test was carried out on 31 PW (5%) and some modifications and rephrasing of certain questions were done. All data collectors were regularly supervised by the principal investigator.
Hemoglobin determination
Two diploma holder medical laboratory technicians were trained for standard operational procedure to determine Hemoglobin level with HemoCue A, weight and height measurement intensively for three days with one senior BSc nurse laboratory technologist assigned as a supervisor. A capillary blood sample was taken by sterile technique for measuring Hemoglobin with HemoCue A photometers by two trained medical laboratory technicians. Hemoglobin value was measured on spot.
Hemoglobin determination procedures
Peripheral blood was collected by finger pricking by using a sterile lancet.
The site for blood collection was cleaned with alcohol-soaked cotton and pricked with a blood lancet.
One drop of blood was taken for hemoglobin (Hgb) measurement.
Hemoglobin value was determined in finger prick blood by using a portable, battery-operated hemoglobinometer (HemoCue A, Angelholm, Sweden) (Cohen and Seidi-Friiedman, 1988).
The first drop of blood was wiped away with dry cotton and the next drop was used to fill the cuvette by touching the cuvette tip in the middle of the drop of blood until completely filled.
The filled cuvette was then put on the holder and pushed into the HemoCue instrument.
The Hg value displayed in g/dl after approximately 45 seconds was registered.
Anthropometric measurements
Body size was assessed through height and weight measurements. Weight and height were taken using a digital portable weighing calibrated SECA scale by one HEW in her respective kebele in collaboration with other data collectors. The PW were weighed wearing lightly clothed in their house and without shoes. The calibrated SECA scale has intervals/sensitivity of 0.1 kg with and a capacity of 130 kg. Height was measured to the nearest 0.1 cm precision and length up to 2 meters using the same device that has a scale and a sliding head piece. Weighing SECA was calibrated to the zero before taking every measurement. To reduce intra-individual errors, weight and height were measured twice by different persons and the mean value was used for the analysis.
Operational definitions
Anemia: Hemoglobin level below 11 g/dl is labeled as anemia during pregnancy and classified as mild (10.0-10.99 g/dl), moderate (7.0-9.9 g/dl), and severe (<7.0 g/dl) anemia and same criteria used for PW.
Study variables
Dependent variable
Anemia (Yes, No)
Independent variables
Socioeconomic factors [age, occupation, average monthly income, educational level, spouse’s educational level, possession of house, floor of their house].
Obstetrics and others factors [gestational age, iron supplementation, gravidity, parity, history of abortion, frequency of abortion, number of children, places of delivery of her previous child, history of blood loss during previous child delivery, ANC utilization for previous pregnancy, frequency of ANC used in current pregnancy].
Data quality management
Quality assurance: Training was given on data collection procedures for interviewers and supervisor. Training was given by senior laboratory technicians to apply standard operational diagnostic procedures. The data collection, application of standard procedure, accuracy of test results was supervised by principal investigator. Close follow up by the investigator during data collection process was done. Filled questionnaires were collected after checking for consistency and completeness.
Ethical considerations: The research proposal was first approved by Addis Ababa University school of Public Health. Before starting data collection, a support letter was written to Oromia regional health bureau and to Ebantu district health office. Those pregnant women who were anemic got appropriate treatment accordingly. Anemic pregnant women are treated with ferrous foliate for free [13]. Health education on dietary practices during pregnancy and importance of anemia was given to by data collectors.
Data Analysis: Data was entered, cleaned and edited using Epi info for windows version 3.5.3 and exported to SPSS for window version 20 for analysis. Descriptive statistics like frequencies, percentage, mean, SD and proportion were calculated first. The association between anemia (hemoglobin value <11 g/dl) and independent variables were examined by crude odds ratio and adjusted odds ratio.
The independent variables with a p value (p<0.3) were included in the multivariate logistic regression analysis. A p-value of less than 0.05 was considered statistically significant. Multiple logistic regressions were applied to determine significant predictors of anemia among pregnant women.
A total of 625 PW(98.7 % response rate) were included in the study. The prevalence of anemia in the study was 35.5% with 95%CI(32.0%, 39.2%). Of these, 23.6% and 14.8% had mild and moderate anemia respectively. The majority of the participants were between ages 25-34 years with an average age of 28.5 years. Nearly half of the study participants were illiterate 302(48.6%) (Table 1).
| Variables | Frequency | Percent (%) | |
|---|---|---|---|
| Residence (n=625) | Urban | 101 | 16.2 |
| Rural | 524 | 83.8 | |
| Occupation of Pregnant mother (n=625) | House wife | 471 | 75.4 |
| Farmers | 33 | 5.3 | |
| Merchant and Employee | 121 | 19.4 | |
| Average Monthly income in cash (n=625) | <500 Birr | 294 | 42 |
| 501-1000 Birr | 128 | 20.5 | |
| >1000 Birr | 205 | 32.5 | |
| Educational level (n=625) | Illiterate | 302 | 48.3 |
| Primary school | 197 | 31.5 | |
| Secondary school | 59 | 9.4 | |
| Tertiary school | 67 | 10.7 | |
| Spouse’s educational level (n=601) | Illiterate | 291 | 48.4 |
| Primary school | 120 | 20 | |
| Secondary school | 87 | 14.5 | |
| Tertiary school | 103 | 17.1 | |
| House possession (n=625) | Our own | 542 | 86.7 |
| Rented | 83 | 13.3 | |
| Floor of their house | Cement | 46 | 7.4 |
| Earthen | 579 | 92.6 | |
Table 1: Frequency distribution of socio-economic characteristics of pregnant women, Ebantu district, west Ethiopia, 2019.
The proportion of gravidity increased in study participants in Primigravida 109(17.4%), multi gravida 296(47.4%), and grand gravida 220(35.2%). Proportion of parity also increased across the PW at the study areas with percentage of Primipara 109(17.4%), multipara 260 (47.4%), and grand multipara 256(35.2%) (Table 2).
| Variables | Frequency | Percent (%) | |
|---|---|---|---|
| Gestational age (n=625) | 1st Trimester (<12 Weeks) | 21 | 3.4 |
| 2nd Trimester (12-28 weeks) | 265 | 42.4 | |
| 3rd Trimester (>28 Weeks) | 339 | 54.2 | |
| Iron supplementation at least for one month (n=625) | Yes | 336 | 54.1 |
| No | 286 | 45 | |
| Number of alive children (n=625) | ≤ 2 years | 286 | 45.8 |
| >2 years | 339 | 54.2 | |
| Gravidity (n=625) | Primigravida (1) | 109 | 17.4 |
| Multigravida (2-5) | 260 | 41.6 | |
| Grand gravida (>5) | 256 | 41 | |
| Parity (n=625) | Primipara (0) | 109 | 17.4 |
| Multipara (1-4) | 296 | 47.4 | |
| Grand multipara (≥4) | 220 | 35.2 | |
| History of Abortion in her life (n=625) | Yes | 159 | 25.4 |
| No | 466 | 74.6 | |
| Frequency abortion (n=159) | Once | 124 | 78 |
| Twice& above | 35 | 27 | |
| Number of her alive children (n=625) | ≤ 2 years | 286 | 45.8 |
| >2 years | 339 | 54.2 | |
| Place of delivery of her last baby (n=416) | Health institutions | 35 | 6.8 |
| Home | 481 | 93.2 | |
| Antenatal care[ANC]utilization for previous pregnancy (n=513) | Yes | 204 | 39.8 |
| No | 309 | 60.2 | |
| ANC utilization in current pregnancy (n=625) | Yes | 361 | 57.8 |
| No | 264 | 42.2 | |
| Frequency of ANC used in current pregnancy (n=361) | Once | 138 | 38.2 |
| Twice | 147 | 40.7 | |
| ≥Three times | 48 | 13.3 | |
| Birth spaces (n=625) | ≤ 2 years | 338 | 65.5 |
| >2 years | 178 | 35.5 | |
Table 2: Frequency distribution of Obstetrics and other characteristics of pregnant women, Ebantu District, west Ethiopia, 2019.
The hemoglobin values ranged from 8.0 g/dl to 16 g/dl with mean ± SD level of 11.8 ± 1.8 g/dl. According to WHO category, anemia observed in the study areas was largely mild anemia with mean 10.5 and SD (14) (Table 3).
| Characteristics | Mean | ± | SD |
|---|---|---|---|
| Hemoglobin (n=625) | 11.8 | ± | 1.8 Hg in g/dl |
| Non anemic (n=403) | 12.6 | ± | 1.3 Hg in g/dl |
| Mild anemia (n=148) | 10.5 | ± | 1.4 Hg in g/dl |
| Moderate anemia (n=74) | 9.7 | ± | 1.6 Hg in g/dl |
| Weight (n=625) | 57.2 | ± | 5.9 kg |
| Height (n=625) | 160 | ± | 9.1 cm |
Table 3: Distribution of the mean /SD of hemoglobin and prevalence of anemia among pregnant women, Ebantu district, West Ethiopia, 2019.
Anemia prevalence was high among of illiterate (41%) with compared primary (35%), secondary (27.1%), and tertiary (5.9%) educated) (Table 4).
| Characteristics | Anemic Hb value <11g/dl (Number (%) |
Non anemic Hb value ≥11g/dl Number (%) |
Total | Crude OR | AOR (95% CI) | |
|---|---|---|---|---|---|---|
| Residence | Urban | 43(42.6) | 58(57.4) | 101 | 1 | 1 |
| Rural | 179(34.2) | 345(65.8) | 524 | 1.1(0.9,1.0) | 0.6(0.4, 1.2) | |
| Ethnic group | Oromo | 205(35.2) | 377(64.8) | 585 | 1 | 1 |
| Amhara | 12(35.3) | 22(64.7) | 34 | 0.8(0.4,1.8) | 1.1(0.4 , 2.2) | |
| Others | 5(55.6) | 4(44.4) | 9 | 2.2(0.6,8.6) | 0.6(0.3, 1.4) | |
| Religion | Protestant | 170(33.1) | 306(64.9) | 476 | 1 | 1 |
| Orthodox | 46(33.1) | 93(66.9) | 139 | 0.7(0.5,1.2) | 3.3(0.6, 17.4) | |
| Others | 6(60.0) | 4(40) | 9 | 2.6(0.7,9.4) | 3.6(0.7, 18.5) | |
| Occupation of Pregnant mother | House wife | 178 (37.8) | 293 (62.2) | 471 | 1 | 1 |
| Merchant and Employee | 30(24.8) | 91(75.2) | 121 | 0.5(0.3,1.6) | 1.2(0.4,3.1) | |
| Farmer | 14(42.4) | 19(57.6) | 33 | 1.2(0.6,2.5) | 0.6(0.7,1.2) | |
| Estimated average monthly income in cash (Ethiopian Birr) | <500 Birr | 89(39.0) | 139(61.0) | 228 | 0.8(0.4,1.6) | 0.4(0.2,1.7) |
| 501-1000Birr | 34(50.7) | 33(49.3) | 67 | 0.5(0.2,1.1) | 0.9(0.5,1.5) | |
| >1000 Birr | 61(29.8) | 144(69.2) | 205 | 1 | 1 | |
| Educational level the pregnant women | Illiterate | 124(41.1) | 178(58.9) | 302 | 2.9(1.5,5.6)* | 5.9(1.8,18.9) ** |
| Primary | 69(35.0) | 128(85.0) | 197 | 2(1.1,4.1)* | 2.6(0.9, 7.) | |
| Secondary | 16(27.1) | 43(72.9) | 59 | 1.8(0.8,4.0) | 2.17(0.8,5.8) | |
| Tertiary | 13(19.4) | 54(80.6) | 67 | 1 | 1 | |
| Spouses educational level | Illiterate | 112(52.8) | 179(46.0) | 291 | 1.9(1.1,3.2)* | 1.6(0.9,2.7) |
| Primary | 31(14.6) | 50(12.9) | 81 | 1.872(1.0,3.3)* | 1.7(0.9,3.2) | |
| Secondary | 19(9.0) | 20(5.1) | 39 | 1.7(1.0,3.239)* | 1.6(0.8,3.1) | |
| Tertiary | 30(14.2) | 57(14.5) | 87 | 1 | 1 | |
Table 4: Association of anemia with socio-demographic characteristics of the study subjects, Ebantu district, West Ethiopia, 2019.
Increased prevalence of anemia among pm was observed across parity; Primigravida (1.4%), multigravida (12.4%), and grand gravida 21.6% for, and respectively and showed that the occurrence of anemia increase as gravidity increases. PW attending ANC on the previous pregnancy showed less prevalence of anemia comparing to those PW who did not attend on the previous pregnancy which was 30.5% and 64.5% respectively. The prevalence of anemia had statistically significant association history of abortion with COR(95% CI):2.4(1.6, 3.5) and AOR(95% CI):2.45(1.6, 3.6) and frequency of abortion with COR(95% CI): 2.6(1.1, 2.5) and AOR 2.69(1.16, 6.2) (Table 5).
| Characteristics | Anemic N (%) | Non anemic N (%) | Total | COR (95 %CI) | AOR (95 %CI) | |
|---|---|---|---|---|---|---|
| Gravidity | Primigravida (1) | 29(26.6) | 80(73.4) | 109 | 1 | 1 |
| Multigravida (2-5) | 88(33.8) | 172(66.2) | 260 | 0.6(0.4,11.0) | 2.2(0.7,11.2) | |
| Grand gravida (>5) | 105(41) | 151(59) | 256 | 0.8(0.6,1.4) | 0.1(0.5,2.2) | |
| Parity | Primipara (0) | 29(26.6) | 80(73.4) | 109 | 1 | 1 |
| Multipara (1-4) | 104 (35.1) | 192(64.9) | 296 | 1.3(0.82,2.1) | 0.8(0.6,1.3) | |
| Grand multipara (≥4) | 89(40.5) | 131(59.5) | 220 | 1.5(0.9,2.4) | 1.7(0.9,2.4) | |
| History of Abortion in her life | Yes | 81(50.9) | 78(49.1) | 159 | 2.3(1.6,3.4)* | 2.4(1.6,3.6)** |
| No | 141(30.1) | 325(69.7) | 466 | 1 | 1 | |
| Frequency abortion among those has its history | Once | 48(38.7) | 76(61.3) | 124 | 1 | 1 |
| Twice and above | 19(70.4) | 8(29.8) | 27 | 2.5(1.1,2.5)* | 2.6(1.6,6.2)** | |
Table 5: Association of anemia with obstetric risk factors of pregnant women, Ebantu district, West Ethiopia, 2019.
As indicated on table 6 below, birth interval, taking iron tablets, abortion and frequency of abortion showed a statistically significant difference with anemia. Proportion of anemia was 35.5% in PW who delivered at home, and 22.9% in women who delivered at health institute on the previous delivery. Pregnant mother those took iron tablets, developed anemia 26%, and who did not take iron tablets was 46.98% (Table 6).
| Factors | Anemic Number (%) | Non-anemic Number (%) | Total | COR(95%CI) | AOR(95%CI) | |
|---|---|---|---|---|---|---|
| Number of her alive children | ≤2 years | 68(31.9) | 145(68.1) | 213 | 1.4(0.9,2.0) | 1.3(0.8,1.9) |
| >2 years | 82(38.3) | 132(61.7) | 214 | 1 | 1 | |
| Place of delivery of her last baby | Health institutions | 8(22.9) | 27(77.1) | 35 | 0.6(0.4,1) | 1.5(0.3,6) |
| Home | 171(35.6) | 310(64.4) | 481 | 1 | 1 | |
| ANC utilization for previous pregnancy | Yes | 62(30.7) | 140(69.3) | 202 | 1.3(0.9,1.9) | 0.8(0.5,1.3) |
| No | 117(65.4) | 193(62.3) | 310 | 1 | 1 | |
| ANC utilization in current pregnancy | Yes | 107(29.8) | 252(70.2) | 359 | 1 | 1 |
| No | 115(43.4) | 150(56.6) | 265 | 1.4(1.1,1.7)* | 1.3(0.8,2) | |
| Frequency of ANC utilization in current pregnancy | Once | 41(29.7) | 97(70.3) | 138 | 1.1(0.6,1.8) | 0.8(0.3,2.1) |
| Twice | 50(5034) | 97(66) | 147 | 0.6(0.3,1.1) | 0.51(0.1,1.7) | |
| Once | 41(29.7) | 97(70.3) | 138 | 1.1(0.6,1.8) | 0.8(0.3,2.1) | |
| ≥ Three times | 16(21.1) | 60(78.2) | 48 | 1 | 1 | |
| History Contraceptive use before this pregnancy | Yes | 102(30.3) | 235(69.7) | 337 | 1 | 1 |
| No | 120(41.7) | 168(58.3) | 288 | 2.3(1.6,3.4)* | 2.2(1.5,.3.4)** | |
| Iron supplementation at least for one month | Yes | 91(26.8) | 248(73.2) | 339 | 1 | 1 |
| No | 131(45.8) | 152(54.2) | 286 | 1.8(1.41,2.2)* | 2.3(1.6,3.3)** | |
| History of malaria diseases since last year | Yes | 77(31.4) | 166(67.7) | 243 | 1.3(0.9,1.9) | 1.2(0.8,1.8) |
| No | 145(61.8) | 235(38.2) | 380 | 1 | 1 | |
| Birth spaces (in average ) | ≤ 2year | 140(41.4) | 198(58.6) | 338 | 1.7(1.1,2.6)* | 1.5(1.1,2.9)** |
| >2 years | 51(28.7) | 127(71.3.2) | 178 | 1 | 1 | |
Table 6: Association of anemia with obstetrics and other risk factors among pregnant women, Ebantu district, West Ethiopia, 2019.
It is a known fact; anemia affects the majority of pregnant women. The study has shown that anemia is prevalent in Ebantu district. Almost one in every three PW had anemia. The prevalence was greater than the national average of 22% in 2011 but lower compared to the study from Jimma 57% and in Sidama zone 51.9% [6,14,15].
After controlling for observed covariates only better educated PW was found to be significant protective factors of anemia. Similarly, education was an important determinant factor as revealed by the study done in India [16]. Regarding obstetric and other determinants [history of abortion, frequency of abortion, history of high blood loss on the previous delivery, number of children, birth spacing and iron tablet supplementation remain statistically significant predictors of anemia].
Consistent with finding from study conducted in Sidama zone, this study indicated shorter birth intervals are more likely to be anemic [6]. Pregnancy with a short birth interval leads to iron deficiency anemia (IDA) as iron requirements are substantially higher than the average and because short birth interval increases risks for uterine rupture [17].
This study revealed Iron supplementation was a protective predictor of anemia among PW. PW who did not take iron during pregnancy were more than two times likely to be anemic than those who took iron supplement. This finding was consistent with study done in Sidama zone and in Pakistan [6,18].
Our study also revealed that prevalence of anemia among aborted mothers was much higher (50.9%) as compare to non- aborted mothers (30.1%) which indicates that previous history of the women should be taken during their first ANC visit to properly manage aborted mothers. This study showed the risk of developing Anemia among those had history of abortion was more than two times likely to have the disease than those did not. The occurrence of anemia being more prevalent in this study among the older agegroup was probably because of the high fertility and greater loss of blood on menstrual.
ANC attendant PW showed low prevalence of anemia (29.8%) but there was high prevalence of anemia (43.4%) in none ANC attendants. ANC initiated in the first trimester facilitates early diagnosis of anemia and allows treatment at the periphery so that the condition can be corrected before delivery.
As the study design was cross sectional study it might not show cause and effect relationship of dependent and independent variable.
Frequency, kinds and doses of iron supplemented were not considered in this study
This study showed that there was high prevalence of anemia among PW and it was considerably higher among PW in third trimester, grand gravida, grand multi gravida, those who had history of abortion and PW who did not attend current ANC regularly. Frequency of abortion greater or equal to two times, birth interval less than or equal to two years, less educational status, and history of iron supplementation on the current pregnancy were significant predictors of anemia.
Women in the study area should be encouraged to use contraceptive and increases birth spacing.
Routine supplementation of iron to pregnant women starting at their first prenatal visit should be encouraged at the study area.
Further investigation on the effects of birth spacing on anemia in pregnancy at different areas should be done.
The authors declare that they have no competing interests.
The authors’ responsibilities were as follows: Wondimu Mitiku Geleta participated in the design of the study, performed the data collection and the statistical analysis and served as the lead author of the manuscript. Zalalem Kaba Babure ensured quality of the data; he assisted in the analysis and interpretation of the data. All authors read and approved the final manuscript.
We are grateful to the staffs of Addis Ababa University School of Public Health, Ebantu District Health Office; Kello Health Center health professionals and Health Extension workers, supervisors, data collectors and study participants for their assistance and cooperation during the study.
Citation: Geleta WM, Babure ZK (2020) Anemia and its Determinant Factors among Pregnant Women in Ebantu District, East Wollega zone, Ethiopia. J Women's Health Care 9:490. doi:10.35248/2167-0420.20.9.490.
Received: 06-Mar-2020 Accepted: 11-Jun-2020 Published: 18-Jun-2020 , DOI: 10.35248/2167-0420.20.9.490
Copyright: Ã?â??Ã?© 2020 Geleta WM, et al. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original work is properly cited.