Medicinal & Aromatic Plants
Open Access
ISSN: 2167-0412
ISSN: 2167-0412
Commentary Article - (2023)Volume 12, Issue 1
Muehlenbeckia platyclda is a medicinal plant which contains quercetin, kaemferol and luteolin and it is used to treat a wide range of disorders including seizure. However, the anticonvulsant activity of this plant has not been studied. We therefore sought to evaluate the anticonvulsant activity of ethanolic extract of M. platyclada aerial parts. Phenyl tetrazole (PTZ) induced convulsion, maximum electro shock (MES) induced convulsion and 6Hz induced convulsion were carried out for screening anticonvulsant activity. The extract was effective in controlling the seizures and its ED 50 value was calculated. It was evident from the studies that the M.platyclada extract had marked anticonvulsant activity. Further experiments will be required to identify the active molecules(s) and their mechanism(s) of action.
Anticonvulsant activity; quercetin; kaempferol; luteolin; Phenyl tetrazole
Evaluation of Anticonvulsant Activity
Evaluation of anticonvulsant activity; maximum electroshock-induced seizures
MBEE at the dose of 400mg/kg had completely abolished HLTE (Hind limb tonic extensor) and HLTF (Hind limb tonic flexion). MBEE (50, 100, 200 and 400 mg/kg) has offered significant and dose-dependent protection against MES-induced HLTF (P <0.01), HLTE (P < 0.01) and stupor (P < 0.01) compared to control. Further, the high dose of MBEE has completely abolished hind limb tonic extensor and hind limb tonic flexion. The reference phenytoin (25 mg/kg) also had completely abolished MES-induced convulsions and mortality. The effective dose (ED50) value of MBEE was found to be 174.28 mg/kg
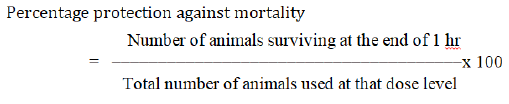
Evaluation of anti-convulsant activity; Phenyl tetrazole (PTZ) induced convulsion
In continuation with MES model, MBEE (50, 100, 200 and 400 mg/kg) was evaluated against PTZ-induced seizures in mice. On administration of PTZ (80 mg/kg,i.p.) the control group animals have showed clonic and tonic convulsions and death. Remarkably, MBEE (50, 100, 200 and 400 mg/kg) has prolonged the PTZ-induced onset of clonus, onset of tonic, and reduced the mortality rate in dose dependent manner compared to control. Exceptionally, a high dose of MBEE (400 mg/kg) has completely inhibited the PTZ-induced tonic convulsions and mortality.
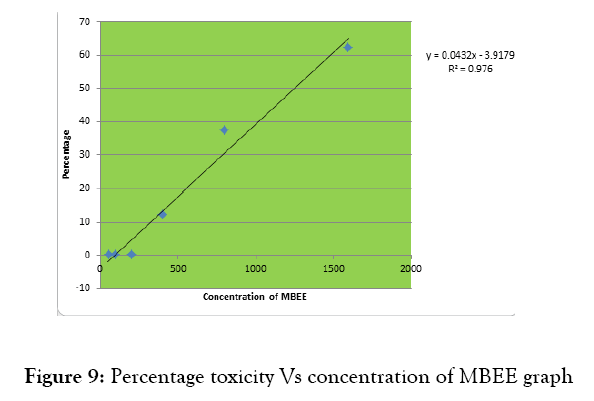
Figure 9: Percentage toxicity Vs concentration of MBEE graph
MBEE (50-400 mg/kg) conferred strong dose-dependent protection in the PTZ induced seizures. At the dose of 400mg/kg it suppressed the tonic seizure by100 %.
MBEE at the doses of 50, 100, 200 and 400 mg/kg showed a protection against PTZ induced mortality in a dose dependent manner. The convulsions were completely abolished by Diazepam (5 mg/kg). ED 50 value is calculated as 173.42 mg/kg.
Evaluation of anticonvulsant activity; 6 HZ seizures test
MBEE exhibited a dose dependent protective activity against this model at the dose levels of 50 – 400mg/kg .Nearly complete protection was observed at the dose of 200 mg/kg. Complete protection was observed at 400 mg/kg dose levels and also the same protection level was observed for diazepam (5mg/kg). ED 50 value was calculated as 158.21mg/kg.
Phenyltetrazole induced convulsion, maximum electro shock induced convulsion and 6Hz induced convulsion were carried out for screening anticonvulsant activity. The extract was effective in controlling the seizures and its ED 50 value was calculated. It suggests that the anticonvulsant activities of MBEE occur through elevation of brain GABA content. Also in the present study the excitatory neurotransmitter glutamate levels were reduced significantly indicating its effectiveness in convulsion MBEE also showed significant increase in the endogenous antioxidant GSH level, in kindled mice brain compared to control mice. MBEE increased the level of SOD, the antioxidant enzyme of the brain
50, 100 and 200 and 400mg/kg doses of MBEE exhibited anticonvulsant effect. The effective dose (ED50) value of MBEE was found to be 174.28 mg/kg. The extract showed a decrease in the duration of the extensor phase. Percentage protection increased with the dose of MBEE. Phenytoin completely inhibited the duration of the tonic extensor phase and protected 100% of animals. HLTE is the universal feature of the MES test in mice, rats and humans [17]. The electroshock assay in mice is used primarily as an indication for compounds which are effective in grandmal epilepsy. Protection against HLTE in the MES test indicates the ability of a drug to prevent the spread of seizure discharge from the epileptic foci in the brain. Its efficacy in the MES test correlates with the efficacy of drugs that suppress generalized tonic–clonic and partial seizures. It acts by causing dose dependent blockade of voltage sensitive sodium channels and by enhancing GABAergic mediated neurotransmission.
An anticonvulsant effect in the MES test model also indicates the ability of the drugs to inhibit or prevent seizure discharge within the brainstem. This indicates the effectiveness of a drug in generalized tonic clonic and partial seizures [18]. MBEE at high doses (200 and 400 mg/kg) inhibited MES induced convulsion, suggesting this may have weak activity against grand mal type of convulsion.
Electroshock delivered in MES model potentiates the sodium influx through opening of sodium channels leading to increased glutamate levels. Glutamate is an excitatory neurotransmitter, which binds with NMDA receptors and induces the symptoms that exactly mimic the petit mal epilepsy in humans. Based on the underlying mechanism of MES convulsions, it can be understood that the agents which could block the voltage-dependent sodium channels (phenytoin, sodium valproate and or the agents that decrease the levels of excitatory amino acids and/or antagonize their actions are proved to be effective in MES-induced epilepsy model [19].
ED 50 value by PTZ model is calculated as 161.36 mg/kg. PTZ is a potent GABA receptor antagonist which is well known to decrease the GABA levels and density of GABA-A receptors in various parts of the brain. This leads to continuous stimulation of cortical neurons and results in convulsions similar to absence seizures in humans. The agents which enhance GABA levels, and/or enhances GABA-A receptor density, and/or GABA-A receptor agonists (like diazepam), and/or the agents behave like GABA are thought to be useful in abolishing PTZ-induced convulsions. PTZ induced convulsions are produced due to diminution of GABA level in brain [20].
ED 50 value using 6 Hz was calculated as 158.21mg/kg. The 6 Hz model is an alternative low frequency (6 Hz), long duration (3 s) electrical stimulation to induce a “psychomotor” seizure. It involves forelimb clonus and stereotyped behaviors that are reminiscent of those exhibited by human patients with complex partial seizures. The 6 Hz seizure model is widely used to identify compounds with unique anticonvulsant profiles and unknown mechanism of anticonvulsant action [21]. Effectiveness of MBEE in 6 Hz model suggests that this compound may be beneficial in complex partial seizures.
The administration of MBEE at 200mg/ kg and 400 mg/kg significantly increased GABA level in the brain. It suggests that the anticonvulsant activities of MBEE occur through elevation of brain GABA content.
It is reported there is a decrease in central nervous system GSH concentration in animals that exhibit generalized seizures. GSH is an endogenous antioxidant. The reduced form of GSH reacts with free radicals and prevents the oxidative toxic injury. The decreased level of reduced glutathione in control group mice seen in the present study indicates that there was an increased generation of free radicals and the reduced glutathione was depleted during process of combating oxidative stress. MBEE showed significant increases the GSH level in mice brain [22].
The findings of current study indicate oxygen and nitrogen free radical contents were considerably enhanced following kindling. These free radicals lead to cellular dysfunction by attacking the polyunsaturated sites of the biological membranes resulting in increased lipid peroxidation. Brain is highly susceptible to oxidative stress because of high demand for oxygen and abundant polyunsaturated fatty acids. Current findings indicate a significant reduction of the brain antioxidant enzymes following kindling because there was a considerable reduction in the activities of SOD. SOD is the main antioxidant enzyme of brain. The ability of the antioxidant defines system of brain against ROS is feeble compared to other tissues. Therefore, brain cells are susceptible to more damages by free radicals. Higher dose of MBEE (400mg/kg) increased the level of SOD which is comparable to that of diazepam (5mg/kg) treated group.
GABA and glutamate are the main neurotransmitters in the brain, and are involved in the pathophysiology of epilepsy. The excitatory neurotransmitter glutamate has been implicated in early changes that lead to the initiation of hyperactivity. The amplification and spread of the excitatory hyperactivity work through two main families of receptors, the inotropic and metabotropic glutamate receptors. In the present study glutamate levels were reduced significantly indicating its effectiveness in convulsion.
The action of serotonin in epilepsy is not clearly understood. In genetically epilepsy prone rat (GEPR) model of epilepsy, the serotonin concentration in the brain was found to be decreased. Pharmacological treatments that facilitate serotonergic neurotransmission inhibit seizures in many animal models, including the MES and PTZ induced convulsions [23].Reduction of brain serotonin concentration may lead to increased seizure susceptibility in animal models of epilepsy as well as in humans [24]. In the current study also MBEE increased serotonin level in brain significantly.
Rotarod Test
The motor toxic effects such as sedation and ataxia to barrel rolling were observed for MBEE. Motor toxicity occurred for 60% of mice at a dose of 1600 mg/kg of MBEE. The TD 50(dose to produce motor incoordination in 50% of the animals) was calculated 45 min after the administration of test compound was found out.
TD50 dose was found out to be 1253.88.30 mg /kg. Muscle grip strength and motor incoordination are known problems associated with antiepileptic drugs. In this study, MBEE showed its therapeutic effect below 400 mg/kg in PTZ, 6HZ and MES induced seizures. No motor incoordination was observed upto 400 mg/kg. At the doses of 800 and 1600 mg/kg showed a gradual increase in motor incoordination. The motor toxicity test (TD50) using rota rod apparatus is commonly used to find out the anticonvulsant potency (ED50) and protective index (PI). In the safety and efficacy evaluation of anticonvulsant drugs, the protective index is much accepted as a standard criterion during the preliminary or secondary screening. A protective index value ≥ 5 is considered as a good margin of safety.
Protective index was calculated based on the formula TD50 / ED50 where TD50 is the dose that produced motor incoordination in 50% of animals.
Glutamate level is significantly reduced (P˂0.0001) in MBEE (400 mg/kg) treated group. Increase in the glutamate level leads to epilepsy but the extract and the standard drug diazepam (5mg/kg) lower the glutamate level. From the results it is clear that MBEE possesses promising anticonvulsant activity.
The level of SOD was increased in MBEE treated group. Administration of MBEE changed the enzyme level with respect to doses. Higher dose of MBEE (400mg/kg) increased the level of SOD which is comparable to that of diazepam (5mg/kg)treated group.
The data is expressed as mean ±SEM. N=5. Analysis of the data was performed by one way analysis of variance(ANOVA) followed by Newman- Keul’s multiple comparison test, at a-P˂0.0001(***) ,compared to the control, b-P˂0.001(**),compared to control.
MBEE exhibited significant increase in reduced glutathione when compared to control. Standard drug benzodiazepine (5mg/kg) also increased glutathione content significantly. The level of reduced GSH was increased in Diazepam (5mg/kg) treated group to 20.4±0. 89micromole/mg. Administration of MBEE changed the enzyme level with respect to doses. Higher dose of MBEE (400mg/kg) increased the level of reduced GSH to 16.4±2.09. The low dose of MBEE showed less significant action (P˂0.05). The higher dose of MBEE shows higher activity. (P˂0.001)
MBEE (200 and 100 mg/kg) increased the GABA level in brain . A similar effect was observed with diazepam (5mg/kg). Pre-treatment with MBEE (200 and 400 mg/kg) increased the brain GABA level in a dose-dependent manner.
Muehlenbeckia genus is also known as maidenhair genus. This genus is indigenous to the Southern Hemisphere, particularly South America, Australia, Papua New Guinea and New Zealand. It might have introduced by cultivation to temperate local north of the equator. [1]Flavanoids were reported in this plant. The main flavanoids were morin-3-O-α rhamnopyranoside, rutin, kaempferol-3-O-βglucopyranoside, quercetin 3-O-α- rhamnopyranoside and (+)-catechin were reported in the plant [2]. These compounds have been reported to possess beneficial effects in numerous diseases in humans, including cancer and cardiovascular diseases. In addition, they also have exhibited antioxidant, antiinflammatory, antitumor and antiviral properties [3]. The ability of flavonoids to cross the blood–brain barrier causes numerous effects on the central nervous system including brain which was revealed both in the in vitro and in vivo studies. Most of the mechanisms involved in generation of seizures in epilepsy have been found to be inhibited by flavonoids. They can modulate neuronal Na+ channels, Ca2+ channels, GABA ergic pathway, glutamatergic pathway and opioid pathway [4].
Figure 1: Evaluation of anticonvulsant activity: Maximum electroshock-induced seizures
Results are expressed as means ± standard error of the mean (SEM). Comparisons between the averages of series of values were performed by ANOVA followed by Dunnett’s multiple comparisons test. Data analysis employed GraphPad INSTAT version 2.0 software; statistical significance was set at.
Six animals were used in each group for each experiment separately. Animals treated with 5% gum acacia suspension (0.1 ml p.o.) served as control. Diazepam (2 mg/kg i.p.) was used as standard. Animals in test group were treated with MBEE (400 mg/kg i.p.). Each animal was treated with respective drug 30 min before experiment. Tests performed were as follows:
Rota-rod performance
Four animals at a time were placed on a rod rotating at 20–25 rpm speed. Only the mice that demonstrated their ability to remain on the revolving rod (20–25 rpm) for 5 min were selected. Training sessions and pretest screening were performed and selected mice were used for studies. The fall off time was recorded in all the groups before and 30 min after administration of drug. Decrease in fall off time is suggestive of depression of the central nervous system (CNS). [15, 16]
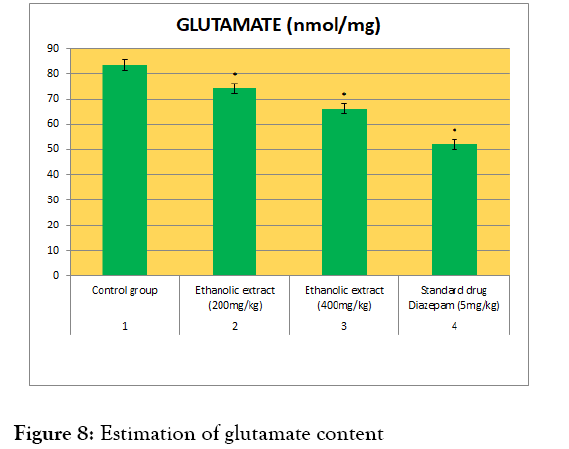
Figure 8: Estimation of glutamate content
Procedure
1.0 ml of the supernatant from brain homogenate was evaporated to dryness at 70°C in an oven and the residue was reconstituted in 100 ml of distilled water. Standard solutions of glutamate and GABA at a concentration of 2mM along with the sample were spotted on Whatman No. 1 chromatography paper using a micropipette. It was placed on a chamber containing Butanol: acetic acid: water (12: 3: 5 v/v) as solvent. When the solvent front reached the top of the paper, it was removed and dried. A second run was performed similarly, after which the papers were dried and sprayed with Ninhydrin reagent and placed in an oven at 100°C for 4 minutes. The portions which carry glutamate corresponding with the standard are cut and eluted with 0.005% CuSo4 in 75% ethanol. The absorbance was read against blank at 515 nm in spectrophotometer. [14]
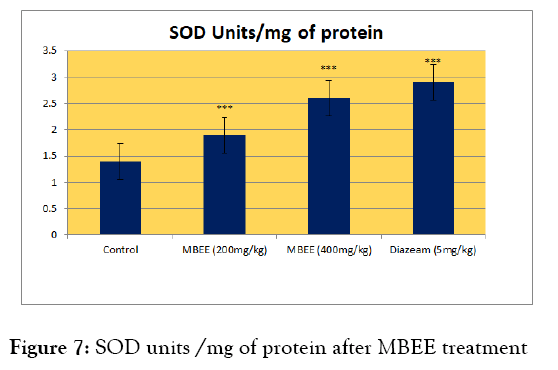
Figure 7: SOD units /mg of protein after MBEE treatment
Calculation
Amount of glutamate are calculated by using the following formula:
A =Unknown OD X Standard in μg (3μg) X 1000 / Standard OD X Volume spotted (10μl) X W
Where, A = Amino acid content in moles/gram wet weight tissue
100 = Conversion factor for gram wet weight tissue
W = Weight of the tissue in gram
OD = Optical density
The data is expressed as the mean ±SEM. N=6. Analysis of the data was performed by one way analysis of variance(ANOVA) followed by by Newman- Keul’s multiple comparison test, at -P˂0.0001(***) ,compared to the control. -P˂0.001 (**),P˂0.05(*), compared to control
Principle
Superoxide radical was generated from the photo reduction of riboflavin and was detected by NBT reduction method.
Procedure
The enzyme extract was prepared by crushing the tissue (0.25g) in 5ml of 0.1M Tris-HCl buffer (pH 7.4).It was then centrifuged at 10000 rpm for 10 minutes at 5°C.The supernatant was used for further assay.Superoxide radical was generated from the photo reduction of riboflavin. Riboflavin is detected by NBT reduction method.
The reaction mixture (2 ml) contained 50 mM Potassium phosphate buffer (pH 7.8), 1.17 mM riboflavin, 10 mM L- methionine, 56 mM NBT and 100 μl protein extract. The absorbance of purple formazan was measured at 560 nm. All photoinduced reactions were performed in an aluminum foil lined box fitted with a 15 W fluorescent lamp. One unit of SOD activity was defined as the exact volume of enzyme causing half maximal inhibition of the NBT. [13]
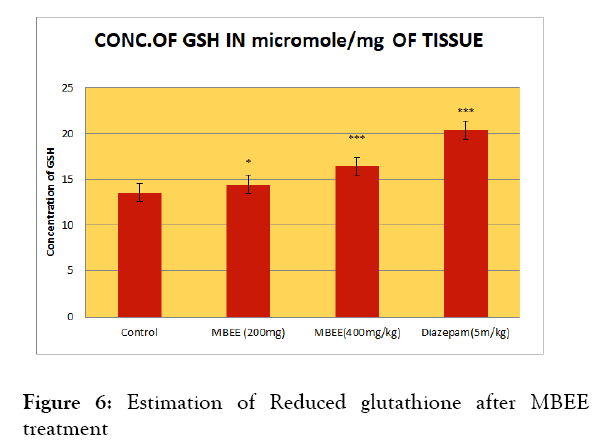
Figure 6: Estimation of Reduced glutathione after MBEE treatment
Preparation of tissue homogenate is as follows. 0.5 g tissue weighed and placed in 5 mL of ice-cold TCA (10% w/v). The tissue was then homogenized and centrifuged at 10,000 rpm for 10 min at 0°C. The supernatant was used for estimation of glutamate content.
The data is expressed as the mean ±SEM. N=6. Analysis of the data was performed by one way analysis of variance(ANOVA) followed by by Newman- Keul’s multiple comparison test, at -P˂0.0001(***) ,compared to the control. -P˂0.001 (**),P˂0.05(*), compared to control
| Treatment | Number of animals fell from the grid | Percentage toxicity |
|---|---|---|
| MBEE 50 | 0/8 | 0 |
| MBEE 100 | 0/8 | 0 |
| MBEE 200 | 1/8 | 12.5 |
| MBEE400 | 2/8 | 25 |
| MBEE 800 | 3/8 | 37.5 |
| MBEE1600 | 5/8 | 62.5 |
Table 8: Percentage toxicity after administration of MBEE
Principle
DTNB and glutathione (GSH) react to generate 2-nitro-5-thiobenzoic acid and glutathione disulphide (GSSG), where 2-nitro-5-thiobenzoic acid yield a stable yellow coloured product, which is proportional to GSH concentration, measured at 412 nm. Glutathione (GSH) is important for cellular defense against peroxides,free radicals, and other toxic compounds.
| SL. NO. | TREATMENT GROUPS | GLUTAMATE(nmol/mg) |
|---|---|---|
| 1 | Control group | 83.38±1.2 |
| 2 | MBEE (200mg/kg) | 74.1±1.3* |
| 3 | MBEE (400mg/kg) | 62.2±2.22* |
| 4 | Standard drug diazepam (5mg/kg) | 53.1±4.2* |
Table 7: Estimation of glutamate content
Procedure
GSH was estimated by the method described by Ellman.[12] The supernatant (0.5 ml) obtained from the brain tissue was mixed with 1 ml of 5% trichloroaceticacid. The mixture was then centrifuged for 10 min at 2000 rpm to remove the proteins. Ellman’s reagent is composed of 5, 5’-dithiobis-2-nitrobenzoic acid prepared in 0.3 M phosphate buffer with 1% of sodium citrate solution. The homogenate (0.1 ml) was mixed with 0.5 mL of the Ellman's reagent, 4 ml of phosphate buffer, and 0.4 ml of double-distilled water. This mixture was then vortexed.The absorbance of the solutions was measured at 412 nm against blank.The results are compared with a standard curve generated from known GSH. The concentration of nonproteinthiols was determined by linear standard graph and expressed as μg/g of brain tissue.
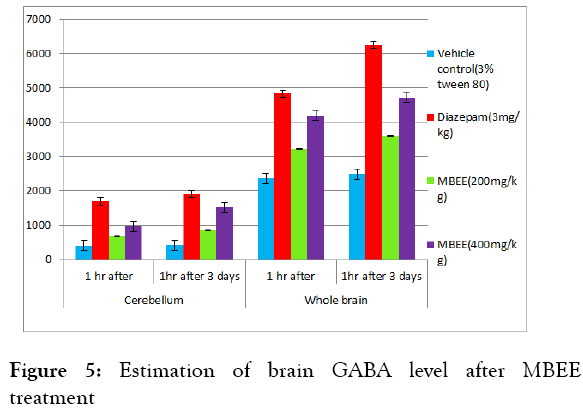
Figure 5: Estimation of brain GABA level after MBEE treatment
The data is expressed as the mean ±SEM. N=10. Analysis of the dta was performed by one way analysis of variance (ANOVA) followed by Newman- Keul’s multiple comparison test, at *P<0.05 and **P<0.00
The test was performed in two different experimental sets. Male Swiss albino mice (25-30 g) were treated with MBEE (200 and 400 mg/kg, p.o.) and also diazepam (3 mg/kg, p.o.) as standard for1 day (single dose) or 3 days (three doses). The first set of experimental animals was sacrificed on day 1, 1 h after the dosing. The second set of animals was sacrificed on day 3, 1 h after the assigned treatment. The brains were collected from all animals and were freezed. The cerebellum and whole brain were separated using microtome blade. These tissues were weighed and transferred to 10 ml of ice-cold 0.1 M perchloric acid that contain 15 μg/ml of valine (internal standard). Under ice-cold conditions the contents were homogenized and centrifuged at 5000 rpm for 10 min at 4°C.The supernatant obtained was subjected to GABAestimation as per Suheretetal [10].
| Treatment | Number of animals that did not showed convulsions | % Protection against convulsions |
|---|---|---|
| Control (3 % Tween 80) | 08-Aug | 0 |
| Diazepam (5 mg/kg) | 0/8 | 100 |
| MBEE(50mg/kg) | 02-Aug | 25 |
| MBEE(100mg/kg) | 03-Aug | 37.5 |
| MBEE(200mg/kg) | 05-Aug | 62.5 |
| MBEE(400mg/kg) | 08-Aug | 100 |
Table 3: Effect of MBEE on anticonvulsant activity: 6 Hz seizures test
100 μl of each supernatant of the samples or the standard GABA was added to a micro-tube that contained 100μl of 0.1 M potassium carbonate solution, to induce dansylation reaction. These solutions were vortexed and centrifuged at 10000 rpm for 10 min. Later, 100 μl of supernatant from each sample was transferred into a Pyrex tube containing 100 μl of 0.1 M sodium hydrogen carbonate solution. To this mixture 400 μl of working dansyl chloride solution (1.25 mg/ml anhydrous acetone) was added.The tubes were vortexed for 30 s and the tubes were incubated at 90°C in benchtop oven for 30 min. During the incubation period the tubes were not capped to allow most of the solvent to get evaporated. The tubes were taken out of the oven, and allowed to cool to room temperature. The dansylated derivatives obtained were transferred to 1.5 ml microtubes and subjected to high-performance liquid chromatography (HPLC) analysis. C8 reversed-phase HPLC column (5 μm, 250 × 3.2 mm) was used. The mobile phase used consists of deionized and helium degassed water: Acetonitrile (HPLC grade) mixture (65:35 v/v) containing 0.15% v/v phosphoric acid. Flow rate was kept at 0.5 ml/min. The fluorescence detector with excitation and emission wavelength of 333 nm and 532 nm were used respectively. 25 μl of the dansylated GABA samples were transferred to HPLC micro-sample vials and injected into the HPLC column. The retention time of GABA and internal standard were determined, and peak ratios of the samples were calculated with reference to the internal standard. The quantification of GABA in the unknown biological sample is calculated using the calibration curve of standard GABA and expressed as ng/g of tissue [11]. The calibration curve for standard GABA was established by subjecting various concentrations (25-6400 ng/ml) of standard GABA stock solutions to dansylation process similar to unknown sample supernatants.
Values are expressed as mean ±SEM from 6 rats. Significant at *P<0.05 and **P<0.001 as compared to control group using one way ANOVA followed by Newman- Keul’s multiple range tests method.
| Treatment | Cerebellum(GABA ng/g) | Whole brain(GABAng/g) | ||
|---|---|---|---|---|
| 1 hr after | 1hr after 3 days | 1 hr after | 1hr after 3 days | |
| Vehicle control(3% tween 80) | 412±4.2 | 426±2.9 | 2370±7.9 | 2490±9.2 |
| Diazepam(5mg/kg) | 1700±8.5** | 1900±7.3** | 4830±14.7** | 6241±9.2** |
| MBEE(200mg/kg) | 670±5.5** | 850±7.2** | 3226±14.2** | 3586±16.4** |
| MBEE(400mg/kg) | 975.8±13.9*** | 1520±8.3** | 4200±8.4** | 4726±5.9** |
Table 4: Brain GABA level after MBEE treatment
| Sl no | Treatment group | Con of GSH in micromole/mg protein |
|---|---|---|
| 1 | Control | 13.5±0.40 |
| 2 | Diazepam(5m/kg) | 20.4±0.89*** |
| 3 | MBEE (200mg) | 14.4±05* |
| 4 | MBEE (400mg) | 16.4±2.09*** |
Table 5: Estimation of Reduced glutathione after MBEE treatment
Standard Preparation
A stock solution of standard GABA, 1 mg/mL was prepared in 0.01M HCl. Serial dilutions were prepared to get concentrations ranging from 1ng /10 μL to 1000 ng/10 μL. Standard concentration curve for GABA was prepared using the same procedure followed by replacing brain homogenate with standard GABA solutions.
| SL.NO | TREATMENT GROUP | SUPEROXIDE DISMUTASE(nmol/mg) |
|---|---|---|
| 1 | Control | 1.4±0.02 |
| 2 | MBEE(200mg/kg) | 1.9±0.011*** |
| 3 | MBEE(400mg/kg) | 2.6±0.02*** |
| 4 | Diazepam(5mg/kg) | 2.9±0.012*** |
Table 6: Estimation of Superoxide Dismutase
Evaluation of Anticonvulsant Activity Maximal Electro Shock Method
The maximum electrical shock (MES) induced convulsion in animal’s represents grand mal type epilepsy. In bred, male Swiss albino mice (25-30 g weight) were randomized and assigned in six groups. Each group consisting of eight animals (n = 8). The respective group animals were treated with vehicle (3% tween 80), phenytoin (25 mg/kg) or MBEE (50, 100, 200 and 400 mg/kg) orally for 3 days. On the 3rd day, exactly after 1 h of the assigned treatment, tetracaine ophthalmic solution (0.5% tetracaine hydrochloride) was applied to cornea. Immediately after the electrical stimulation, all the animals were observed in an open top plastic cage for 30 min. The parameters such as duration of hind limb flexion, hind limb extensor, stupor, and death/survival were recorded. All the animals were carefully observed. The percentage protection is calculated using survival rate using the equation. [5, 6, 7]
All of the values are expressed as mean±SEM (n=8); means of various groups were statistically compared by one way ANOVA followed by Newman- Keul’s multiple range tests method. *P<0.01, **P<0.001 compared with control (3% tween 80). MBEE: Methanolic leaf extract of Muhlenbeckia platyclada, HLTE: Hind limb tonic extensor, HLTF: Hind limb tonic flexion, ND: Not detected.
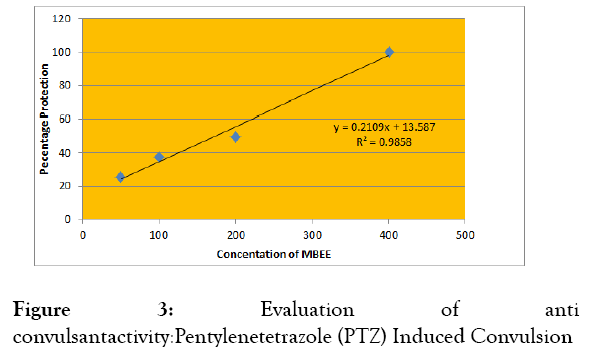
Figure 3: Evaluation of anti convulsantactivity:Pentylenetetrazole (PTZ) Induced Convulsion
| Serial number | TREATMENT | DURATION OF TIME (Sec) | ||||
|---|---|---|---|---|---|---|
| GROUP | ||||||
| HLTE | HLTP | Stupor | Recovery/Death | Percentage Protection | ||
| 1 | Control | 17.63 | 7.13±0.70 | 127.49±1.42 | 0/8 | 0 |
| 2 | Phenytoin (25mg/kg) | ND | ND | 49.15±0.25** | 08-Aug | 100 |
| 3 | MBEE (50mg/kg) | 12.25± | 5.38±0.40* | 109.38±0.47* | 01-Aug | 12.5 |
| 4 | MBEE | 9.63± | 3.88±0.2** | 96.87±4.47* | 03-Aug | 37.5 |
| (100mg/kg) | ||||||
| 5 | MBEE | 4.63±0.25 | 1.13±0.47** | 05-Aug | 62.5 | |
| (200mg/kg) | 88.13±0.25** | |||||
| 6 | MBEE | ND | ND | 68.25±4.9** | 07-Aug | 87.5 |
| (400mg/kg) | ||||||
Table 1: Effect of MBEE on anticonvulsant activity: Maximum electroshock-induced seizures
Evaluation of Anticonvulsant Activity Phenyl tetrazole (PTZ) Induced Convulsions
In bred, male Swiss albino mice (25-30 g) were divided into six groups. Each group consisting of eight animals (n = 8). The respective group animals were treated with either vehicle or diazepam (5mg/kg) or MBEE (50, 100, 200 and 400 mg/kg) orally for 3 days. On the 3rd day, 1 h after the assigned treatment of the vehicle, Diazepam and MBEE, Phenyl tetrazole (PTZ 80 mg/kg) was intraperitoneally administered to all the experimental animals. They were individually observed in a plastic cage initially for 30 min. The animals survived were observed later up to 24 h. During the individual observation, the parameters such as onset of clonus, onset of tonic convulsions, and death/survival were recorded and expressed as percentage protection using the equation. [8]
Figure 4: Effect of MBEE on anticonvulsant activity: 6 Hz seizures test
All of the values are expressed as mean±SEM (n=8); means of various groups were statistically compared by one way ANOVA followed by using Newman- Keul’s multiple range tests method. *P<0.01, **P<0.001 compared with control (3% tween 80). MBEE: ethanolic extract of Muehlenbeckia platyclda, ND: Not detected.
Evaluation of Anticonvulsant Activity; 6 Hz Seizures Test
| Group | Onset of clonus | Onset of tonic | No of animals survived | Percentage protection | ED 50 |
|---|---|---|---|---|---|
| Control(3% tween) | 38.7±2.5 | 72.9±4.1 | 0/8 | 0 | 173.42/kg |
| Diazepam (5mg/kg) | ND | ND | 8/8 | 100 | |
| MBEE(50mg/kg) | 48.7±3.5** | 83.9±5.2** | 1/8 | 12.5 | |
| MBEE(100mg/kg) | 64.8±3.1*** | 100.9±7.12*** | 3/8 | 37.5 | |
| MBEE(200mg/kg) | 148.6±4.2*** | 186.6±11.10*** | 4/8 | 50 | |
| MBEE(400mg/kg) | 194.1±5.1*** | ND | 8/8 | 100 |
Table 2: Effect of MBEE on anti-convulsant activity: Pentylenetetrazole (PTZ) Induced Convulsion
The mice were pretreated with extracts .The doses ranging from 50 to 800 mg/kg, p.o were used for the study. The animals were treated with MBEE for 3 days. The dose selection was done based on acute toxicity study. Based on the response observed at 100 mg/kg, further dose levels were selected to establish dose-response correlation. In the process of establishing the dose response correlation minimum dose was started with 50 mg/mg and saturation was observed after 200 mg/kg. On Day-3, 1 h after the last dose, tetracaine ophthalmic solution (0.5% tetracaine hydrochloride) was applied. After 30 min the corneal electrodes were wetted with saline and electrical stimulation was given for 3 s (200 μs-duration, 32-mA mono polar rectangular pulses at 6 Hz) to all animal, using a constant current device ECT Unit 5780. After the electrical stimulation, a stunned posture will be seen along with rearing and repeated movements that lasted from 60 to 120 s in control animals. After the seizures, animals will be resumed to normal exploratory behavior. The end point in this model is defined as protection against the seizures. The animals which gain their normal exploratory behavior within 10 s of stimulation are considered as protected [9].
Plant Extract Preparation
The entire plant of Muehlenbeckia platyclada was collected from Karyvattom campus, Thiruvananthapuram on April 2015. The plant materials were recognized and authenticated from The Pharmacognosy Unit, Ayurveda Research Institute, and Trivandrum. The herbarium specimen had been lodged in Department of Pharmacognosy, Mar Dioscorus College of Pharmacy, and Trivandrum (Herbarium No: MDCP/PCG/Herb No: 001/11/2015).The materials were cleaned with water dried in shade and was coarsely grinded. The powdered drug was extracted with ethanol in soxhlet apparatus.
Animals
The Swiss Albino mice (18-25g) of either sex were housed in a group of five per cage. They were maintained under natural day and night cycle at 25±2ºC ambient temperature with 45-55% relative humidity. The animals were allowed to acclimatize for one week before the experiment with 12 hours dark and 12 hours, light cycle. Animals were allowed free access to standard pellet diet and water ad libitum. The experiments were carried out as per the guidelines of committee for the purpose of control and supervision of experiments on animals (CPCSEA), New Delhi, India. Study protocol was approved by the Institutional Animal Ethics Committee (IAEC). The protocol number is IAEC/P.ANCY/MAHERU/8814008/PhD/KMCP/ 24/2018.
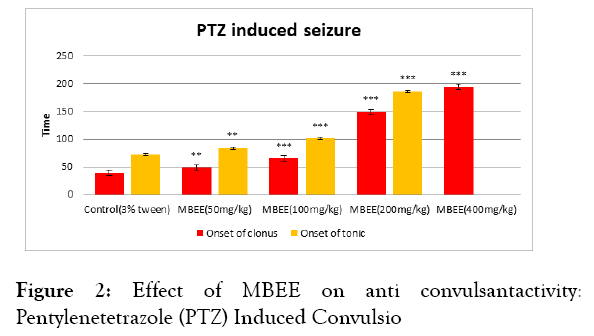
Figure 2: Effect of MBEE on anti convulsantactivity: Pentylenetetrazole (PTZ) Induced Convulsio
Acute toxicity study
The oral acute toxicity study of the aqueous extract of Muehlenbeckia platyclada was carried out using the single doses of 175, 500 and 2000 mg/kg in accordance with the Organization for Economic Development (OECD) guideline no. 425 (Organization for Economic Development, 2001). Five female mice were used for each dose level in the study. An animal was picked at a time, weighed and administered with the equivalent volume of extract dissolved in distilled water. The extract was administered orally using gastric feeding tube. Each animal was observed after dosing for the first 5 min for signs of regurgitation and was kept in a cage. Each animal was then observed every 15 min in the first 4 h after dosing and also every 30 min for 6 h. They were also observed daily for 48 h for behavioral signs of toxicity (changes in skin, hair, eyes, mucous membranes, and respiratory, circulatory, autonomic and central nervous systems, motor activity, convulsion, tremors, salivation, diarrhoea, lethargy, or sleep) according to the specifications of the OECD (2001). The animals were monitored for a total of 14 days for the long-term possible lethal effects if any. The body weights of the animals were measured on days 1, 7, and 14.
Citation: Ancy P, Padmaja V, Nithinmanohar R, Rajkumar R, Shijikumar P S (2021) Anti-convulsant action and amelioration of oxidative stress by ethanolic extract of aerial parts of Muehlenbeckia platyclada. Med Aromat Plants 10:p34
Received: 18-Aug-2021, Manuscript No. MAP-22-12425; Editor assigned: 20-Aug-2021, Pre QC No. MAP-22-12425 (PQ); Reviewed: 10-Sep-2022, QC No. MAP-22-12425; Revised: 17-Sep-2022, Manuscript No. MAP-22-12425 (R); Published: 24-Sep-2022 , DOI: 10.35284/2471-9315.22.11.437
Copyright: © 2021 ANCY P, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.