Immunome Research
Open Access
ISSN: 1745-7580
ISSN: 1745-7580
Research Article - (2022)Volume 18, Issue 2
Introduction: Vaccination against COVID-19 promoted among high-risk populations such as an oral health care worker is one of the most rapidly and massively deployed interventions in history.
Objective: The overall objective of our study was to assess the perception and attitudes regarding COVID-19 vaccination among oral health care workers in comparison to other health care workers in Yaoundé.
Materials and methods: A cross-sectional study was conducted from February to April 2022 (3 months) on 360 health personnel in three hospitals in Yaoundé. All health personnel who gave informed consent were included in the study. Statistical analysis was performed using SPSS 26.0 software with a significance level of p<0.05.
Results: In more than half of the cases, doubt about the efficacy of the COVID-19 vaccines was found without any difference between the oral practitioners (53.3%) and the others (58.7%) (p=0.476). Fear of harm was mainly found among oral practitioners (75.0% vs. 46.4%; p=0.006). There was no statistically significant difference in terms of vaccination coverage and motivations for vaccination between our two socio-professional groups (p ≥0.05).
Conclusion: the fear of the harmfulness of the COVID-19 vaccine was preponderant among healthcare personnel working in the oral sphere. De-structuring the representation of this vaccine among this population could improve the response to this disease.
COVID-19 vaccination; Perception; Attitude; Health workers; Oral health care
Coronavirus 2019 (COVID-19) vaccination is one of the most rapidly and massively deployed public health interventions in history worldwide [1]. According to the World Health Organization, most countries in the African Region will miss the target of vaccinating 70% of their populations by the end of June 2022, underscoring the need to focus on achieving targets among priority groups in all countries [2]. As of April 2022, 14.3% of Africans were fully vaccinated against severe acute respiratory syndrome coronavirus (SARS-CoV 2). COVID-19 is a highly contagious viral infection classified as a pandemic due to the rapid spread of the virus throughout the world [3]. In Cameroon, more than one hundred thousand cases have been reported with a case-fatality rate of 1.6% and a vaccination rate of 8.5% in the general population [4]. Health personnel in the front line of the fight against the disease are one of the priority groups that should benefit from response interventions [5,6]. In May 2022, 54.9% of health personnel were fully vaccinated in Cameroon [4]. The mode of transmission of this disease is airborne by inhalation of the virus from contaminated respiratory droplets, and by direct or indirect contact with an infected person [7]. The oral sphere, including the oral cavity, ears, nose and sinuses, is the primary site of virus multiplication. Due to their proximity to this area, direct contact with oral fluids and the generation of aerosols during health care procedures, health care personnel working in the oral area (oral medicine, maxillofacial surgery, otolaryngology) appear to be at increased risk of contracting SARS-CoV 2 [8,9]. The still low vaccination coverage according to WHO recommendations raises the question of cognitive constructs around vaccines among health care personnel. The aim of this study is to evaluate the difference in perception and attitudes regarding COVID-19 vaccination among oral health care workers compared to other health care workers in Yaoundé.
Type, location and period of the study
A cross-sectional analytical study was conducted over a three-month period from February 1, 2022 to April 30, 2022 in three hospitals in Yaoundé. Our study sites were the Yaoundé Central Hospital, the Yaoundé General Hospital, and the Yaoundé Gyneco-Obstetric and Pediatric Hospital. These are reference hospitals in the Cameroonian health system, and are among those with the largest number of health care personnel in the city of Yaoundé. They have many specialized services and care units.
Study population
The study population consisted of the medical and paramedical staff of the hospitals in our study. Oral practitioners were defined as oral physicians, Ear-Nose-Throat (ENT) specialists, residents in stomatology and ENT, and technicians and nurses in stomatology and ENT departments. All other health care personnel were considered to be practitioners outside the oral sphere. In these two groups, those of Cameroonian nationality and having given their consent were included. Any participant who voluntarily withdrew from the study or did not wish to provide certain information from the questionnaire was excluded from the study. The recruitment method was non-probability consecutive and exhaustive.
Procedure
Health care personnel from all functional departments at each study site were approached. A physical, self-administered questionnaire was submitted to each participant at the conclusion of the interview and after informed consent was obtained. An online version was made available to facilitate the collection of information from the majority of staff.
Study variables
The data collected were socio-demographic variables such as gender, age, marital status, religion, professional specialty, and years of experience, and those related to COVID-19 vaccination such as perception, motivations, and reasons for reluctance to take vaccines.
Statistical analyses
The data collected were entered and analyzed using SPSS (Statistical Package for Social Sciences) version 26.0 software. Categorical variables were expressed as numbers and percentages and quantitative variables as mean and standard deviation or median and interquartile range depending on the distribution of the data. Comparison between variables was done using the Chi-square or Fisher exact test. A p value<0.05 was considered statistically significant.
Administrative and ethical considerations
We obtained research authorizations in the different study sites, associated with an ethical clearance from the ethics committee of the Faculty of Medicine and Biomedical Sciences of Yaoundé (FMSB). The information collected was used exclusively within the framework of this study and in strict compliance with research ethics.
During the study period, we recruited 377 health personnel, of whom 17 participants were excluded, for a participation rate of approximately 95%. A total of 360 questionnaires were analyzed.
General characteristics of the study population
The female gender (222; 61.7%) and the model classes (30-40 years) in terms of age (136; 37.8%) and (1-10 years) in terms of years of work experience (248; 68.9%) of the participants were predominant. A total of 60 (16.7%) oral health personnel and 300 (83.3%) non-oral health personnel were selected. Oral physicians, ENT and stomatology nurses, and otolaryngologists were the most common oral health care professionals: 23.3% (14/60), 21.7% (13/60), and 20.0% (12/60) respectively. As for the other practitioners, paramedical personnel represented more than half (162/300; 54.0%) (Table 1).
| Variable | Number | Percentage (%) |
|---|---|---|
| Gender (N=360) | ||
| Male | 138 | 38,3 |
| Female | 222 | 61,7 |
| Age range (years) (N=360) | ||
| [20-30] | 103 | 28,6 |
| [30-40] | 136 | 37,8 |
| [40-50] | 88 | 24,4 |
| [50-60] | 33 | 9,2 |
| Work expérience (years) (N=360) | ||
| [1-10] | 248 | 68,9 |
| [10-20] | 86 | 23,9 |
| [20-30] | 24 | 6,7 |
| [30-40] | 2 | 0,6 |
| Area of expertise (N=360) | ||
| Oral (n=60) | 60 | 16,7 |
| Non-oral (n=300) | 300 | 83,3 |
| Oral staff (N=60) | ||
| Oral physician | 14 | 23,3 |
| Nurse | 13 | 21,7 |
| ENT specialist | 12 | 20,0 |
| ENT Resident | 7 | 11,7 |
| Stomatology Resident | 5 | 8,3 |
| Dental Technician | 5 | 8,3 |
| Maxillofacial Surgeon | 2 | 3,3 |
| Orthodontist | 1 | 1,7 |
| Prosthodontist | 1 | 1,7 |
| Non-oral staff (N=300) | ||
| Paramedical staff | 162 | 54,0 |
| Medical Specialist | 84 | 28,0 |
| General practitioner | 49 | 16,3 |
| Pharmacist | 5 | 1,67 |
| Note: ENT: Ear-Nose-Throat | ||
Perception and attitudes toward COVID-19 vaccines
Slightly more than half of the participants (208/360; 57.8%) doubted the efficacy of the vaccines. There was no statistically significant difference between the two socio-professional groups (p=0.476). Oral health workers were significantly more likely to report that they perceived the COVID-19 vaccines as harmful (53.3% vs. 46.4%; p=0.006). Approximately three out of ten healthcare workers (123/360; 34.2%) had received at least one dose of a COVID-19 vaccine. The field of expertise was not significantly associated with vaccination status (p=0.135). In our two socio- professional groups, few were in favor of taking the booster doses with 19.2% in the oral sphere group and 32.5% in the non-oral sphere group, with no significant difference (p=0.156) (Table 2).
| Variable | Oral sphère (%) N=60 | Non-oral sphère | P |
|---|---|---|---|
| (%) N=300 | |||
| Doubtfulness of vaccine efficacy | 32 (53,3) | 176 (58,7) | 0,476 |
| Harmfulness of vaccines | 45 (75,0) | 167 (46,4) | 0,006 |
| Taking the vaccine | 26 (43,3) | 97 (32,3) | 0,135 |
| Complete vaccination | 24 (40,0) | 93 (31,0) | 0,606 |
| Acceptability of the booster dose | 26 (19,2) | 97 (32,5) | 0,156 |
Motivations for vaccination against COVID-19
There was no statistically significant difference in the distribution of motivations for vaccination between our two groups: vaccination of colleagues (p=0.624), compulsion (p=0.327), exposure to the disease by profession (p=0.374). The main reason for vaccination was its usefulness in the response to the disease in both the oral group (18; 69.2%) and the non-oral group (72; 74.2%) (Figure 1).
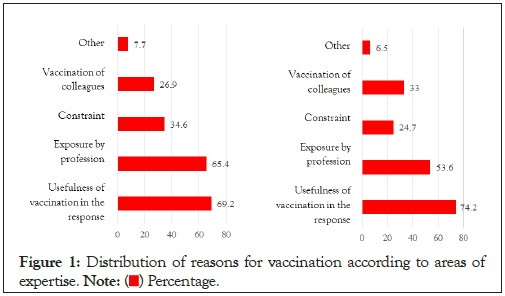
Figure 1: Distribution of reasons for vaccination according to areas of expertise. Note: ( ) Percentage.
) Percentage.
The general objective of this study was to evaluate the difference in perception and attitudes related to COVID-19 vaccination among oral health practitioners compared to other health personnel in Yaoundé. In our study we found a predominance of women (61.7%) with a sex ratio of 0.61 in favor of women; this trend was similar to that of Doumou et al. in Cameroon in 2022, who found a predominance of women in a study conducted among medical and paramedical personnel [6]; Fouogue et al. in 2020 in Cameroon also found a predominance of women in a study conducted among health personnel [10]. This trend could be explained by the predominance of women in the medical professions in Cameroon (55.74%) [11]. A mean age of 36.1 ± 8.52 years was found, with extremes of 20 and 57 years, which was similar to that reported by Fouogue et al. in Cameroon in 2020 who found a mean age of 35 ± 8.9 years [10]. This could be explained by the fact that we included in our study residents and interns, who were young, newly graduated health personnel.
Fifty-eight percent (58.0%) of the health personnel in our study found COVID-19 vaccines ineffective and 58.9% found these vaccines harmful. These results would be in agreement with those of Alle et al. in Ethiopia in 2021 [12] who estimated that 57% of health workers found these vaccines ineffective and 62% found them harmful. This could be explained by the fact that information about these vaccines suggests that they do not prevent disease occurrence, the need for booster doses, and the reported cases of severe side effects from vaccination [13]. Nevertheless, these trends were in contrast to those of Moucheraud et al. in Malawi in 2021 [14] and Ye et al. [15] in China in 2021 who found respectively 26% and 39.1% of staff who found these vaccines ineffective; the difference observed would reflect the fact that the perception of COVID-19 vaccines in terms of efficacy and harm is variable, and could be explained by the infodemia that exists around COVID-19 vaccines; the types and qualities of sources of information about vaccination among health care staff would therefore vary. In addition, a majority of oral and non-oral healthcare workers reported that they found these vaccines ineffective. However, those in the oral group reported significantly more that they found these vaccines harmful.
The main reasons for vaccination were the usefulness of vaccination for the fight against the disease (73.2%) and the fear of contracting the virus through work (56.1%); these results corroborated those of Li et al. in 2021 in China [16], who found in his series the same main determinants for vaccination. Indeed, vaccines have always been considered as the safest and most efficient means of controlling the spread of diseases [1,2], which would justify the reason why health workers accepted to receive them. In our study population, 32.5% of those vaccinated reported acceptability of a booster dose of vaccine. This low figure could reflect a lack of satisfaction with vaccination, which could be explained not only by the fear of adverse effects experienced with the first doses of vaccine, but also by the possibility of contracting the disease despite vaccination and the occurrence of post-vaccination deaths that have been documented [17,18]. These results were, however, contradictory to those of Moucheraud et al. This difference may be due to the fact that the Moucheraud et al. study was conducted shortly after the introduction of corona virus vaccination and therefore the vaccinated individuals were still very receptive to receiving the booster doses. The lack of evidence of vaccination at the time of our investigation was our main limitation.
The fear of the harmfulness of the COVID-19 vaccine was preponderant among health personnel working in the oral sphere; on the other hand, doubt about the efficacy of the COVID-19 vaccine was predominantly found among all health personnel. The main reason for vaccination was the usefulness of vaccines for the response to the disease. It seems important to focus communication on the safety and efficacy of COVID-19 vaccines for health personnel.
The research team gratefully acknowledges the administrative staff of the Yaoundé Central Hospital, Yaoundé General Hospital, and the Yaoundé Gyneco-Obstetric and Pediatric Hospital and all participants in this study.
The authors declare that they have no conflicts of interest.
Esther Voundi Voundi, Marie Elvire Nokam and Joseph Kamgno designed the study. Jacqueline Michèle Lowe and Elisabeth Songue collected the data. Eric Nseme, Haamit Abba-kabir and Elisabeth Songue performed the statistical analysis. Esther Voundi Voundi, Jacqueline Michèle Lowe and Marie Elvire Nokam wrote the manuscript. Joseph Kamgno, Eric Nseme and Haamit Abba-kabir critically reviewed the manuscript. All authors gave their approval for publication.
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
Citation: Voundi EV, Lowe JM, Abena MEN, Nseme E, Abba-kabir H, Songue E, Kamgno J (2022) Anti-COVID-19 Vaccination: Perception and Attitudes among Oral Health Practitioners and Other Health Personnel in Yaoundé. Immunome Res 18: 154.
Received: 27-Jun-2022, Manuscript No. IMR-22-18084; Editor assigned: 30-Jun-2022, Pre QC No. IMR-22-18084 (PQ); Reviewed: 14-Jul-2022, QC No. IMR-22-18084; Revised: 20-Jul-2022, Manuscript No. IMR-22-18084 (R); Published: 29-Jul-2022 , DOI: 10.35248/1745-7580.22.18.154
Copyright: © 2022 Voundi EV, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.