Advanced Techniques in Biology & Medicine
Open Access
ISSN: 2379-1764
ISSN: 2379-1764
Research - (2022)Volume 10, Issue 9
Objective: To explore the significance of anxiety and depression in children with Postural Tachycardia Syndrome (POTS).
Study design: The study enrolled seventy-one children diagnosed as POTS in Beijing Children's Hospital Affiliated to Capital Medical University and Kaifeng Children’s Hospital, aged 13 ± 2 years; The Self-Rating Depression Scale (SDS), the Self-Rating Anxiety Scale (SAS), the Hamilton Depression (HAMD) scale, and the Hamilton Anxiety (HAMA) scale were carried out in POTS children. The POTS children were divided into two groups: anxiety/depression group and non-anxiety/depression group according to the above scales scores. Heart Rate (HR), and Blood Pressure (BP) were monitored by a Dash 2000 Multi-Lead Physiological Monitor.
Results: Twenty POTS children consisted of anxiety/depression group. Twelve were girls and eight were boys, with mean age of 14 ± 2 years. The non-anxiety/depression group included fifty-one POTS children, aged 12 ± 2 years. Twenty-six were girls and twenty-five were boys. There were no statically differences in weight, gender, Systolic Blood Pressure (SBP), Diastolic Blood Pressure (DBP), and HR in supine. The age and height of anxiety/depression group were higher than that in non- anxiety/depression group. The maximum HR (HRmax) in ten minutes of upright position or tilt, the change of HR from supine to upright position (Δ HR), symptom scores in anxiety/depression group were significantly higher than that in non-anxiety/depression group. Four scale scores were correlated with symptom scores and ΔHR. Multivariate general linear model analysis revealed that HAMD scores and SAS scores were closely associated with the OI symptom scores.
Conclusion: Anxiety and depression emotion might be involved in the pathogenesis of POTS.
Anxiety; Depression; Heart rate; Postural tachycardia syndrome; Score
Postural Tachycardia Syndrome (POTS) is one of the most common syndromes in postural change or prolonged standing with sinus tachycardia accompanied by Orthostatic Intolerance (OI) symptoms [1]. Some POTS patients even might be attacked by syncope in severe cases. The incidence of POTS is approximately 6.8% among children and adolescents, and this condition seriously affects their physical health, psychological health, and quality of life [2]. Therefore, it is great of importance to clarify the pathogenesis of POTS.
The pathogenesis of POTS is complex, because some factors interact or co-exist. Previous studies suggested that the pathogenesis of POTS mainly included elevated catecholamine, insufficient cardiac volume, autonomic nerve dysfunction, vascular endothelial dysfunction, muscle pump dysfunction, etc [3]. Jordan et al. believed that anxiety state, palpitations and increased heart rate in supine position are all susceptible factors of POTS [4]. Liao et al. discovered that Flow-Mediated Dilation (FMD) in POTS children was increased, which indicated that vascular endothelial dysfunction, might be one of the pathogenesis of POTS [5]. However, the pathogenesis of POTS factors has not yet been clarified clearly at present, which needs to be urgently studied.
Several studies showed that psychological factors were closely associated with cardiovascular disease. Rumsfled found that psychological factors were risk factors for cardiovascular patients which could significantly increase the incidence and mortality of cardiovascular diseases [6]. Recent studies showed that depression and anxiety were strongly correlated with high blood pressure, heart failure, coronary heart disease, arrhythmia, etc [7]. With the development of society, the accelerated pace of life and the increase of competitive pressure, the study pressure of children and adolescents in China increases, and the number of people suffering from exam anxiety and the incidence of depression is higher than that reported in previous years [8]. A new research demonstrated that VVS patients compared with normal healthy people, had greater psychological pressure and lower quality of life [9]. Investigations have revealed that anxiety and depression could effect on the Hypothalamic-Pituitary-Adrenocortical axis (HPA) and lead to hyperactivity of the sympathetic nervous system [10]. Remme et al. discovered that depression and anxiety could lead to increased sympathetic nerve excitability and rise of blood catecholamine levels, which could cause the excessive increase of heart rate (HR) [11]. The aim of this study was to explore the significance of anxiety and depression in the pathogenesis of POTS and the correlation between anxiety and depression and severity of POTS.
Seventy-one POTS children diagnosed in Beijing children's hospital affiliated to capital medical university and Kaifeng children's hospital were recruited from November 2018 to October 2019, including 33 boys and 38 girls, with an average age of 13 ± 2 years. The study was approved by the ethics committee of Beijing children's hospital affiliated to capital medical university and Kaifeng children's hospital, and all the subjects' guardians signed informed consent.
Head-Up Test (HUT)
The children were asked to keep in supine for 10 minutes. HR and Blood Pressure (BP) were measured afterwards. Then, the children were instructed to maintain upright position and the changes of BP and HR were recorded dynamically by a Dash 2000 Multi-Lead Physiological Monitor (General Electric, NY, New York, USA). During the HUT, OI symptoms such as dizziness, chest tightness and palpitations should be paid attention. If the patient cannot tolerate the test, the test should be stopped immediately. If the children showed loss of consciousness on HUTT, they would be kept lay down rapidly [12,13].
Head-Up Tilt Test (HUTT)
Before the beginning of HUTT, the children were required to stop taking all drugs that might affect the autonomic nerve function, and kept fast for at least for four hours. The test was carried out in a dim light and quiet environment. First, Children lay down on the tilt bed for 10 minutes and HR, BP were detected by a Dash 2000 Multi-Lead Physiological Monitor (General Electric, NY, New York, USA). Then the tilt bed tilted to 45 degree, and children standed on the bed for 45mintues or until positive response appeared [14].
Diagnosis of POTS
(1) Mostly occurred in elderly children; (2) the condition is often associated with predisposing factors, such as a rapid change from the supine position to the upright position or prolonged standing; (3) symptoms of OI, such as dizziness, headache, fatigue, blurred vision, chest tightness, palpitations, hand tremors, and syncope; (4) a HR increase of ≥ 40 beats per minute (bpm) or a maximum HR (HRmax) of ≥ 130 bpm (for 6-12 year-old children) or ≥ 125 bpm (for 13-18 year-old adolescents) without orthostatic hypotension (BP decrease of >20/10 mmHg) during the first 10 min of the standing test or basic head-up tilt test; and (5) exclusion of other diseases that can cause OI symptoms, such as organic cardiovascular diseases, metabolic diseases, neurological diseases, or mental illness. Patients also underwent evaluations to collect data regarding their medical history, physical status, Usg index, electrocardiograph parameters, standing test, electroencephalography, cranial computed tomography or magnetic resonance imaging, basic head-up tilt test, and psychological tests.
OI symptom scoring system
According to the frequency of clinical OI symptoms, including the followings: syncope, dizziness, chest tightness, nausea, palpitation, headache, blurred vision, trembling hands and cold sweat, symptom scores were calculated. The scoring criteria were defined as follows: zero score, never; one score, once a month; two scores, 2-4 times a month; three scores, 2-7 times a week; four scores, more than once a day. The score was the sum of the symptom scores.
Anxiety and depression rating scales
Zung's self-rating anxiety/depression scales such as Self-Rating Depression Scale (SDS), Self-Rating Anxiety Scale (SAS) and Hamilton Anxiety/ Depression (HAMA/HAMD) scales, are often used evaluation of anxiety in patients with cardiovascular disease for mental disorders and also applied to children and adolescents [15,16]. SDS, SAS, HAMD, and HAMA were applied to evaluate the psychological state of POTS children. The evaluation criteria were made as follows: SAS scores >50 were evaluated as anxiety. SDS score >53 was associated with depression. HAMA scores >14 was considered to be related with anxiety; HAMA scores > was thought as depression. POTS children with both scales positive consisted the anxiety and depression group. On the contrary, POTS children were considered as non-anxiety and depression group. Patients with discordant results of the two scales were excluded. According to their psychological evaluation results, POTS children were divided into anxiety and depression group (20 cases) and non-anxiety and depression group (51 cases).
Statistical methods
SPSS 16.0 version (IBM, Armonk, New York) were employed to data calculation. Measurement data were expressed as mean ± standard deviation or quartile (the upper quartile, the lower quartile). Independent sample t test or independent sample non-parametric test were used for comparison between the two groups. Pearson correlation analysis was used for correlation analysis. P<0.05 was considered difference to be statistically significant.
Comparison of general demographic characteristics and clinical data of POTS children in two groups: Twenty POTS children consisted of anxiety/depression group. Twelve were girls and eight were boys, with mean age of 14 ± 2 years. The non- anxiety/depression group included fifty-one POTS children aged 12 ± 2 years. Twenty-six were girls and twenty-five were boys. There were no statistical differences in weight, gender, Systolic Blood Pressure (SBP), Diastolic Blood Pressure (DBP), and HR in supine between two groups. The age, height, HRmax, and the change of HR from supine to upright position (ΔHR) of anxiety/depression group were higher than that in non- anxiety/depression group (P<0.05, Table 1).
| Characteristics | Anxiety/ depression group | Non-anxiety/ depression group | t/c2 | p value |
|---|---|---|---|---|
| Cases, n | 20 | 51 | - | - |
| male/female | 08-Dec | 25/26 | 0.492 | 0.6 |
| Age, yrs | 14 ± 2 | 12 ± 2 | -2.523 | 0.014 |
| Height, cm | 165 ± 8 | 158 ± 11 | -2.275 | 0.026 |
| Weight, kg | 53.4 ± 7.3 | 48.6 ± 13.5 | -1.492 | 0.14 |
| HRmax, bpm | 129 ± 11 | 122 ± 10 | -2.333 | 0.023 |
| HR, bpm | 52 ± 8 | 44 ± 8 | -3.93 | 0.001 |
| Systolic BP, mmHg | 105 ± 9 | 101 ± 11 | -1.605 | 0.113 |
| Diastolic BP, mmHg | 64 ± 7 | 62 ± 12 | -0.69 | 0.493 |
| Heart rate, beats/min | 77 ± 11 | 78 ± 11 | 0.692 | 0.491 |
Note: BP: Blood Pressure; POTS: Postural Tachycardia Syndrome.
Table 1: Baseline characteristics of the anxiety/depression group and non-anxiety/depression group of POTS.
Comparison of HAMA scores, HAMD scores, SAS scores, SDS scores, and symptom scores: The HAMA scores, HAMD scores, SAS scores, SDS scores, and symptom scores in anxiety/depression group were significantly higher than that in non- anxiety/depression group (P<0.01,Table 2).
| Characteristics | Anxiety/ depression Group | Non-anxiety/ depression Group | t/c2 | p value |
|---|---|---|---|---|
| Cases, n | 20 | 51 | - | - |
| Symptom Score, score | 13 ± 3 | 7 ± 3 | -7.721 | 0.001 |
| HAMA, score | 28 ± 8 | 8 ± 3 | 16.796 | 0.001 |
| HAMD, score | 24 ± 5 | 4 ± 2 | -24.621 | 0.001 |
| SAS, score | 52 ± 6 | 16 ± 8 | -18.763 | 0.001 |
| SDS, score | 33 ± 9 | 14 ± 5 | -11.72 | 0.001 |
Table 2: Parameters compariosn between the anxiety/depression group and non-anxiety/depression group of POTS.
Correlation analysis of HAMA scores, HAMD scores, SAS scores, SDS scores and symptom scores, ΔHR: HAMA scores, HAMD scores, SAS scores, SDS scores were positively correlated with symptom scores and ΔHR (Figures 1 and 2).
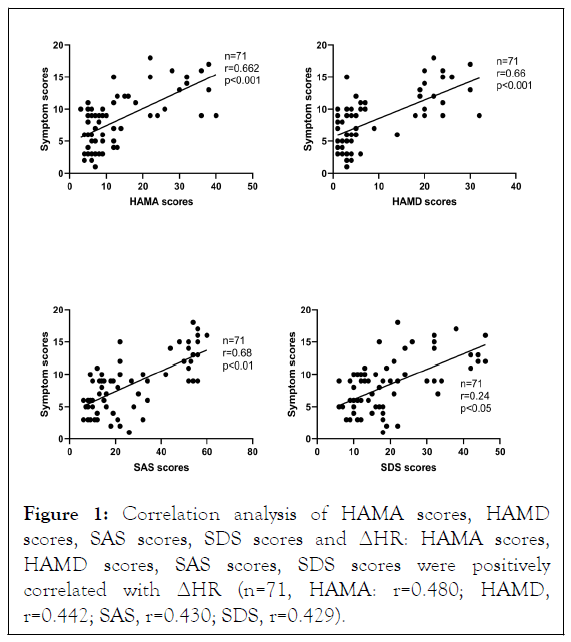
Figure 1: Correlation analysis of HAMA scores, HAMD scores, SAS scores, SDS scores and ΔHR: HAMA scores, HAMD scores, SAS scores, SDS scores were positively correlated with ΔHR (n=71, HAMA: r=0.480; HAMD, r=0.442; SAS, r=0.430; SDS, r=0.429).
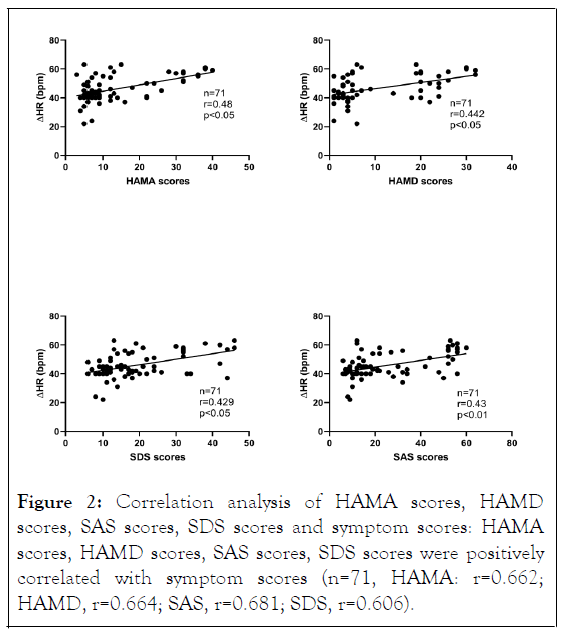
Figure 2: Correlation analysis of HAMA scores, HAMD scores, SAS scores, SDS scores and symptom scores: HAMA scores, HAMD scores, SAS scores, SDS scores were positively correlated with symptom scores (n=71, HAMA: r=0.662; HAMD, r=0.664; SAS, r=0.681; SDS, r=0.606).
Multivariate general linear model analysis: The multi-variable model was adjusted for sex, age, BMI, HAMA scores, HAMD scores, SAS scores, SDS scores, which revealed that HAMD scores (defined as X1)and SAS scores (defined as X2) were closely associated with the OI symptom scores (defined as Y) in children and adolescents with POTS. The regression equation established according to the model is: Y=4.171+0.16X1+0.27X2.
In our study, we firstly discovered that HAMA scores, HAMD scores, SAS scores, SDS scores, HR max in ten minutes of upright position or tilt, the ΔHR, OI symptom scores in anxiety/depression group were significantly higher than that in non- anxiety/depression group of POTS children. More importantly, HAMA scores, HAMD scores, SAS scores, SDS scores positively correlated with symptom scores and ΔHR were newly explored.
POTS are a kind of OI syndrome with complicated pathogenesis. Dizziness, chest tightness, palpitations, blurred vision and sweating are common symptoms of OI, and even syncope can occur in severe cases, which has a serious impact on the daily life and learning quality of children [3]. Lin J discovered that the incidence of POTS in Chinese children and adolescents is up to approximately 7%, and sleeping time less than 8 hours was a risk factor contributing to POTS [14]. The pathogenesis of POTS is complex, nevertheless, not clear [17]. Studies have shown that social psychological factors, especially depressive and anxious states, were closely related to the incidence and mortality of cardiovascular diseases [18]. What’s more, researchers confirmed that anxiety and depression could act on Hypothalamus-Pituitary-Adrenal axis (HPA) and produce hyperactivity of the sympathetic nervous system [10]. Studies have shown that depression and anxiety could increase sympathetic excitability, up-regulated levels of catecholamine in the blood, and heart rate [11]. The increase of catecholamine is one of the main pathogenesis of POTS [19]. In our study, it was found that HR max of POTS children in anxiety/depression group were significantly higher than that in non-anxiety/depression group, which may be related to the increase of catecholamine in blood by influencing hypothalamus-pituitary-adrenal cortex axis and the sympathetic nervous system hyperactivity. Moreover, the OI symptom scores of POTS children was correlated with anxiety/depression scores, which further indicated that anxiety and depression may be involved in the pathogenesis of POTS by increasing the content of catecholamine in the blood.
Previous studies have shown that vascular endothelial dysfunction played a vital role in the pathogenesis of POTS [20]. Gamboa found that the content of Nitric Oxide (NO) and Nitric Oxide Synthase (NOS) in POTS children were significantly higher than those in healthy children, indicating that NO may be related to the pathogenesis of POTS [21]. The plasma C-type Natriuretic Peptide (CNP), a vasoactive peptide mainly derived from vascular endothelial cells, in POTS children was significantly higher than that in the control group, while CNP has the function of vasodilation vessels, which suggested that endothelial dysfunction was involved in the pathogenesis of POTS [3]. In addition, abnormal amounts of sulfur dioxide, intermedin, and other vascular active substances related to endothelial function in POTS children suggested that impaired endothelial function is closely related to the pathogenesis of POTS [22,23].
Studies have shown that anxiety and depression might affect vascular endothelial function in terms of autonomic nervous function, inflammatory factors and bone marrow response after acute ischemia [24-26]. Anxiety and depression in patients with stable angina were found to be an independent risk factor for impaired vascular endothelial function [27]. Sherwood discovered that dependent relaxation function of brachial artery endothelium in patients with coronary heart disease with significant depressive or anxiety was significantly lower than that in patients without depressive or anxiety (P=0.001), and anti-depressive therapy could significantly improve the endothelial function of patients with coronary heart disease (P<0.05) [28]. All the above studies demonstrated that anxiety and depression could affect vascular endothelial function. However, vascular endothelial cells can release a variety of active substances such as endothelin-1 (ET-1) and NO to maintain normal body functions. NO is a substance synthesized by vascular endothelial cells that can relax vascular endothelial function. Anxiety and depression may cause excessive dilation of peripheral blood vessels in POTS children by affecting the level of NO and other active substances, reducing the volume of central blood pressure, thus causing excessive heart rate in POTS children when they are in upright, which further participated in the pathogenesis of POTS.
This study found that HAMA scores, HAMD scores, SAS scores, SDS scores positively correlated with symptom scores and Δ HR, suggesting that anxiety and depression may be involved in the pathogenesis of POTS, which also provides a new treatment approach of POTS. The limitation of this study is that it is a single-center study with a small sample size, and a multi-center and large-sample joint study needs to be further studied. What’s more, if the treatment of follow-up plan is carried out, it will be more meaningful to guide the personalized treatment selection of POTS. For example, OI symptoms of POTS children in the anxiety/depression group were relieved after psychological treatment, which could further indicate that mood disorders may be involved in the pathogenesis of POTS. In the future, large-size based multi-center studies with prolonged follow-up period are needed.
[Crossref][Google Scholar][PubMed].
[Crossref][Google Scholar][PubMed].
[Crossref][Google Scholar][PubMed].
[Crossref][Google Scholar][PubMed].
[Crossref][Google Scholar][PubMed].
[Google Scholar][PubMed].
[Google Scholar][PubMed].
[Crossref][Google Scholar][PubMed].
[Crossref][Google Scholar][PubMed]..
[Crossref][Google Scholar][PubMed].
[Crossref][Google Scholar][PubMed].
[Crossref][Google Scholar][PubMed].
[Crossref][Google Scholar][PubMed].
[Crossref][Google Scholar][PubMed].
[Crossref][Google Scholar][PubMed].
[Crossref][Google Scholar][PubMed].
[Crossref][Google Scholar][PubMed].
[PubMed].
[Crossref][Google Scholar][PubMed].
[Crossref][Google Scholar][PubMed].
[Crossref][Google Scholar][PubMed].
[Crossref][Google Scholar][PubMed].
[Crossref][Google Scholar][PubMed].
Citation: Yuan Y, Shao W, Li H, Gao L, Han Z (2022) Anxiety and Depression in Children with Postural Tachycardia Syndrome. Adv Tech Biol Med. 10:375.
Received: 18-Jul-2022, Manuscript No. ATBM-22-19514; Editor assigned: 21-Jul-2022, Pre QC No. ATBM-22-19514 (PQ); Reviewed: 05-Aug-2022, QC No. ATBM-22-19514; Revised: 12-Aug-2022, Manuscript No. ATBM-22-19514 (R); Published: 19-Aug-2022 , DOI: 10.35248/2379-1764.22.10.375
Copyright: © 2022 Yuan Y, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.