International Journal of Physical Medicine & Rehabilitation
Open Access
ISSN: 2329-9096
ISSN: 2329-9096
Review Article - (2021)
Supraspinatus tendinopathy is a common cause of shoulder pain and tendon degeneration in individuals who participate in repetitive overhead activities, such as tennis players or tradespeople. Early diagnosis and treatment of tendinopathies is necessary to prevent chronic sequelae and tendon rupture, which is especially important for groups such as professional athletes and manual workers for avoidance of prolonged downtime.
Shear wave elastography; Supraspinatus tendinopathy; Achilles; Patellar; Humeral epicondylar tendons
Traditionally, B-mode sonography, power Doppler and magnetic resonance imaging have been used for the recognition of tendinopathies [1,2]. Morphologically, tendon thickening, inhomogeneous tendon structure and loss of tendon thickness are indicative of a pathological tendon, alongside nonmorphological changes such as increased vascularization [2]. However, morphological changes may not be present in symptomatic patients with tendinopathy, leading to a high falsenegative rate. This limits the sensitivity of ultrasonography and power Doppler to 67% for detecting tendinopathy in the Achilles, patellar and humeral epicondylar tendons [2]. Additionally, correct observation of features consistent with tendinopathy is dependent on the assessor’s ability and experience. An interobserver B-mode ultrasonography study evaluating the supraspinatus tendon for tendinosis found decreased agreeability between the three assessors, which included two musculoskeletal sonographers, each with greater than 6-years of experience, and another individual with 6- months of experience [3]. Between the two musculoskeletal sonographers, the kappa value was only 0.55 (p=0.005), highlighting a weak level of agreement regarding pathological tendons despite both being of a professional standard [3]. Similarly, whilst intra-observer reliability of supraspinatus tendinosis using magnetic resonance imaging was reported as excellent (intraclass correlation coefficient of 0.85), the interobserver reliability was only fair to good (intraclass correlation coefficient of 0.55) [4].
Although B-mode sonography and magnetic resonance imaging morphologically provides information indicative of tendon quality, it does not quantify or rate a tendon’s mechanical properties, such as stiffness [2].
Shear wave elastography is a developed application of ultrasonography that quantifies the mechanical properties of soft tissues, such as tendons, by measuring the rate at which shear waves propagate through the tissue [5]. While its musculoskeletal use is still evolving, shear wave elastography has been used to characterise the properties of other soft tissues including the liver, prostate, breast, brain, and carotid arteries [5,6].
In shear wave elastography, an Acoustic Radiation Force Impulse (ARFI) is released, resulting in local stress and displacement of the closest tissue. Shear waves generate perpendicularly to the initial ARFI in the transverse plane and are rapidly attenuated as they travel slowly through nearby tissue, causing shear displacement. Fast plane wave excitation is used to form tissue displacement maps, from which shear wave velocity, expressed in metres per second (m/s), can be derived [6]. Shear wave velocity at each pixel directly relates to the tissue’s shear modulus, which is a marker of the tissue’s mechanical integrity [5]. A tissue’s shear modulus (G) is defined as the ratio of stress to strain and can be calculated by [G=pcs2] where p is the material density, cs is the shear wave velocity and G is recorded in units of pressure, commonly kilopascals (kPa). Shear wave velocity can also be used to evaluate tissue stiffness/elasticity using Youngs modulus, which is defined by the equation [E=3G], where E is Young’s modulus (in kPa units). The process of shear wave elastography is summarised (Figure 1) [6].
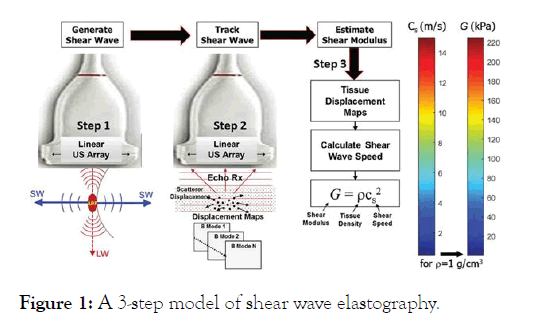
Figure 1: A 3-step model of shear wave elastography.
The underlying principle behind shear wave elastography is that materials deform differently in response to stress, allowing an insight into their biomechanical properties such as stiffness [6]. Tendons with good mechanical integrity have a high velocity and are coloured red on the system, whilst tendons with reduced viability exhibit decreased velocity and are coloured blue (Figure 2). However, as a relatively new technique, there is a need to evaluate the reliability of shear wave elastography ultrasound on the assessment of normal and tendinopathic tendons [7].
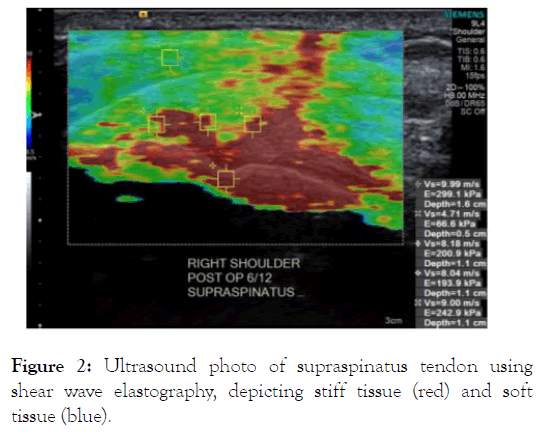
Figure 2: Ultrasound photo of supraspinatus tendon usingcshear wave elastography, depicting stiff tissue (red) and soft tissue (blue).
Shear wave elastography can categorise healthy and pathological tendons independent of location in the body, with studies showing reduced shear wave velocity in tendinopathy of the rotator cuff, Achilles, patellar and humeral epicondylar tendons [2]. Of additional benefit, shear wave elastography can quantify the severity of tendinopathy through ranking tendon stiffness from 0-15 m/s, or in units of kilopascals. In a study of the Achilles, humeral epicondylar and patellar tendons, a shear wave elastography value of less than 70 kPa (4.8 m/s) indicated disease, whilst values above this number highlighted good tendon health [2]. In a study specific to the supraspinatus tendon, the mean shear wave velocity values were found to be greater than 8-9 m/s in the normal tendon, and 5-7 m/s or lower in those with tendon degeneration or tearing [8].
In contrast to B-grade ultrasonography and magnetic resonance imaging, shear wave elastography has been effective in recognising pathology within symptomatic tendons [9], with a specificity of 100% and a positive predictive value [1]. Dirrichs et al. determined that the mean shear wave elastography value of the Achilles, lateral epicondylar and patellar tendons was 60 kPa within symptomatic patients, and significantly higher in asymptomatic patients, at 168 kPa (p<0.0001) [2]. The ability for shear wave elastography to detect reduced stiffness in symptomatic patients is beneficial for early diagnosis, intervention, and post-operative outcomes (Figure 3).
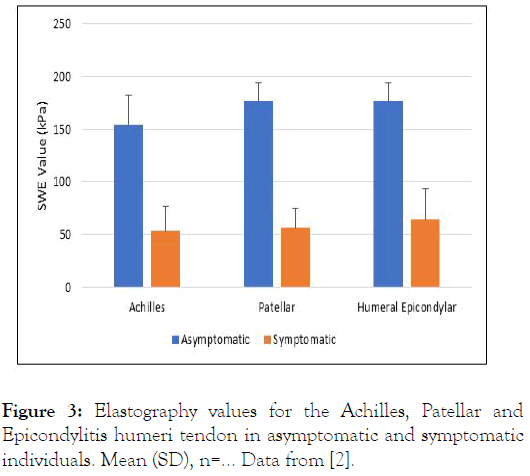
Figure 3: Elastography values for the Achilles, Patellar and Epicondylitis humeri tendon in asymptomatic and symptomatic individuals. Mean (SD), n=… Data from [2].
There was also reported to be a significant, negative correlation between the shear wave velocity and the morphological grade of the supraspinatus tendon (p<0.001), which was ranked from mild tendinosis (grade 1) to full thickness tear (grade 4) [8]. This is important, as many surgeons recognise tendon quality to be an important prognostic indicator for post-operative healing [10]. High grade, tendinopathic tendons, recognised by reduced shear wave velocity, are more likely to exhibit failure at the tendon-suture interface due to suture pull-through. As such, shear wave elastography may be useful for patient selection and surgical planning, as reduced tendon quality may encourage surgeons to attempt alternative repair strategies such as the use of a synthetic graft [8].
Post-treatment, shear wave elastography may be useful in monitoring the healing tendon. In another study of the Achilles, patellar and humeral epicondylar tendon, improvements in the VISA score, an index for the severity of tendinopathy, following 6-months of treatment were accompanied by an increase of 4.6 m/s in shear wave elastography values, indicating improved stiffness [9]. Thus, shear wave elastography may act as an effective indicator for monitoring treatment response in tendinopathies, potentially leading to the establishment of more personalised and effective treatment plans (Figure 4).
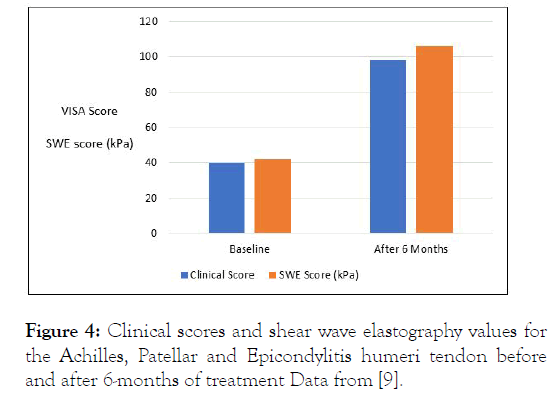
Figure 4: Clinical scores and shear wave elastography values for the Achilles, Patellar and Epicondylitis humeri tendon before and after 6-months of treatment Data from [9].
In this issue of the Journal, the intra- and inter-observer reliability of shear wave elastography for assessing the supraspinatus tendon are reported in a study by Hackett et al. The study focussed on 20 patients, including 10 who had healthy supraspinatus tendons and 10 with supraspinatus tendinopathy. Overall, Hackett et al. demonstrated high intraobserver reliability of tendon assessment when used by a trained musculoskeletal sonographer (intraclass correlation coefficient of 0.95). Reliability decreased when assessment was conducted by three individuals, with an intraclass correlation coefficient of 0.45. This is likely due to variable skill levels of the assessors, which included a trained musculoskeletal sonographer, a research assistant with nil ultrasound experience and a medical practitioner with limited ultrasound use. This study reflects previous research performed by Baumer et al. Which reported high intra-observer reliability in measurement of the supraspinatus muscle and tendon (intraclass correlation coefficient of 0.87), especially when there was a low level of muscle activation [10,11]. Whilst the inter-observer reliability remained high in this study (intraclass correlation coefficient of 0.73), the experience of the two sonographers was not revealed.
Despite the benefits of using shear wave elastography to evaluate the biomechanical properties of tendons, there remain limitations. Tendon imaging requires precise parallel or perpendicular placement of the probe to the tendon fibres [10,12]. However, with the complex structure of tendons, such as the orthogonally shaped supraspinatus, proper positioning may be difficult, especially if the sonographer is inexperienced [13]. For example, the shear wave velocity of the Achilles tendon decreased from 16 m/s to 7 m/s in the sagittal orientation of measurement when the foot was plantar flexed [14.] However, when an ankle fixator was used for standardised foot positioning, reproducibility improved [15,16]. As such, for shear wave elastography values to be a reliable measurement of a tendon’s stiffness, there is a need for the establishment of guidelines, education and standardised methodology regarding correct patient positioning, the use of controls and the location of the measurements.
In addition, reference ranges for healthy and tendinopathic tendons should be defined for different subgroups and tendons. Another study by Dirrichs et al. Established that semiprofessional athletes had significantly higher stiffness in the Achilles tendon than non-athletic individuals (183 kPa and 104 kPa respectively) [17]. No such study has been performed in the supraspinatus tendon, but it is likely that boxers and other athletes training their shoulders have stiffer supraspinatus tendons. These interindividual differences need to be considered when rating a tendon’s integrity as “healthy” or “diseased”. This is because an athlete with tendinopathy may still have a shear wave elastography value in the normal range for a non-athletic individual, thereby delaying diagnosis [17]. Similarly, tendon stiffness decreases with age, with individuals aged 20-35 years reported to have significantly greater (p=0.03) supraspinatus tendon stiffness than those aged older than 60 years (24 kPa and 18 kPa respectively) [18]. As such, reduced tendon stiffness in an older individual may lead to the inappropriate diagnosis of tendinopathy when their stiffness may be normal for their age. Stiffness values also vary depending on tendon location. In a study of asymptomatic, healthy individuals, the supraspinatus tendon averaged a stiffness of 31 kPa, whereas the Achilles tendon was measured to be 74 kPa and 52 kPa in the longitudinal and transverse plane respectively [19]. If the same reference range for identifying tendinopathy is used for all tendons, some pathological tendons may be misdiagnosed as normal.
Overall, shear wave elastography has great potential in the evaluation of the mechanical integrity of a tendon, which is necessary in early diagnosis, intervention, and post-operative prognosis. However, improved education and standardised guidelines are necessary to increase inter-user reliability. Further, it would be beneficial to establish reference ranges for the accurate determination of tendinopathy in different sub-groups.
Citation: Playford SE, Hackett L, AC Murell G (2021) Application of Shear Wave Elastography in Diagnosing Tendinopathies. Int J Phys Med Rehabil. 9: S4:002
Received: 16-Apr-2021 Accepted: 30-Apr-2021 Published: 07-May-2021 , DOI: 10.35248/2329-9096.21.s4.002
Copyright: © 2021 Playford SE, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.