Advances in dairy Research
Open Access
ISSN: 2329-888X
ISSN: 2329-888X
Research Article - (2022)Volume 10, Issue 4
Background: Globally, in 2015 there were an estimated 2.7 million neonatal deaths which represents 45% of all deaths among children under five. In Ethiopia, according to WHO neonatal mortality rate is still high 29 per 1,000 live births. The majority of these new born deaths occur at home where a few families recognize signs of newborn illness and delays in decision to seek care at household level. However, different studies focus mostly on the prevalence of neonatal death and essential newborn care practice disregard of mother’s knowledge about neonatal danger sign and their health care seeking behavior which is one of the critical delays in neonatal illness.
Objective: This study was intended to assess the level of knowledge and health care seeking behavior about WHO recognized neonatal danger signs and associated factors among mothers in Gasera district, Ethiopia.
Methods: A community based cross sectional study design using quantitative supplemented with qualitative methods was conducted from March 12 to April 10, 2017. Stratified multistage sampling and purposive sampling method was used for quantitative to select 501 mothers and qualitative method respectively. Data entering and coding were performed with Epidata 3.1 and analyzed by SPSS version 20 using descriptive, bivariate and multivariate techniques. Thematic qualitative data analysis was also used.
Results: Mothers who had knowledge of neonatal danger signs were found to be 26.0%. The odds of having good knowledge was positively associated with husband’s formal education (AOR=2.33, 95% CI 1.24, 4.53), birth preparedness (AOR=3.04, 95% CI 1.68, 5.52), health extension workers home to home visit (AOR=5.45, 95% CI 2.78, 10.7), receiving family health card (AOR=7.52, 95% CI 4.10, 13.82), PNC follow up (AOR=2.52, 95% CI 1.30, 4.92) and television access (AOR=3.15, 95% CI 1.55, 6.40). About 182(55.8%) of the mother sought medical treatment for their newborn while only 31.3% sought immediate medical treatment within 24 hour. Likewise, the odds of having good health care seeking behavior for neonatal illness was statistically positively associated with maternal knowledge towards neonatal danger sign (AOR=2.56, 95% CI 1.18, 5.54), family income (AOR=2.10, 95% CI 1.15, 3.81), PNC follow up (AOR=2.24, 95% CI 1.24, 4.05), and receiving family health card (AOR=3.04, 95% CI 1.38, 6.70).
Conclusion: This study showed maternal knowledge about neonatal danger signs and health seeking behavior was low. Therefore, intervention modalities focusing on increasing access to PNC service, advocating the use of television, provision and use of integrated family health booklet for health information, and HEWs home to home visit was recognized.
Neonatal danger sign; Health care seeking behavior; Gasera District
ANC: Antenatal Care; AOR: Adjusted Odd Ratio; CBNC: Community Based Newborn Care; CI: Confidence Interval; COR: Crude Odd Ration; CSA: Central Statistical Agency; EDHS: Ethiopia Demographic and Health Survey; ENC: Essential Newborn Care; ETB: Ethiopian Birr; FMOH: Federal Ministry of Health; HEW: Health Extension Worker; IMNCI: Integrated Management of Neonatal and Childhood Illnesses; IMR: Infant Mortality Rate; MCH: Maternal and Child Health; NMR: Neonatal Mortality Rate; PNC: Post Natal Care; PPS: Probability Proportional to Size; SPSS: Statistical Package for Social Scientists; SRS: Systematic Random Sampling; WHO: World Health Organization; WorHO: Woreda Health Office
Background
Newborn danger signs refer to presence of clinical signs that would indicate high risk of neonatal morbidity and mortality, and the need for early therapeutic intervention. The danger signs are; stopped feeding well, history of convulsions, fast breathing (breathing rate >60/min), severe chest in-drawing, no spontaneous movement, fever (temperature >37.5°C), low body temperature (temperature <35.5°C), any jaundice in first 24 hour of life, or yellow palms and soles at any age [1,2].
Globally, the two regions of sub-Saharan Africa and South Asia has both the highest proportion of neonatal deaths and one of the highest overall under-five mortality rates as well as in South Asia neonatal mortality is considerably higher than expected relative to the global pattern [3].
The major causes of neonatal mortality in 2015 were prematurity, birth-related complications (birth asphyxia) and neonatal sepsis, while leading causes of child death in the post-neonatal period were pneumonia, diarrhea, injuries and malaria. Thus, achievement of sustainable development goals (SDG target 3.2) for child survival depends on more effectively addressing neonatal deaths, particularly early deaths in the first week of life [4].
In the first 28 days the majority of newborn deaths could be prevented with key interventions around the time of birth and improved care for small and sick newborns [3]. Integrated Management of Newborn and Childhood Illness (IMNCI) developed by the World Health Organization (WHO) focuses on assessment of general danger signs in the examination of children presenting with illness at health care centers [1,2]. World Health Organization in 2013 strongly recommended specific danger signs that should be assessed during each postnatal care contact and the new born should be referred for further evaluation if any of the signs are present. The family should also be encouraged to seek health care early if they identify any danger signs in-between postnatal care visits [1].
Globally, in 2015 an estimated 5.9 million children under 5 years of age died, with a global under-five mortality rate of 42.5 per 1000 live births. There were 2.7 million neonatal deaths (deaths within the first 28 days of life), with a global neonatal mortality rate of 19 per 1000 live births which represents 45% of all deaths among children under five. A similar number of babies are still born [5,6]. The majority of these new born deaths occur at home where a few families recognize signs of newborn illness and nearly all neonates are not taken to health facilities when they were sick [7].
In most regions, success in tackling later childhood diseases means a larger share of the neonatal period. As global rates of underfive mortality have fallen, neonatal deaths now account for a rising proportion of the remaining burden of under-five deaths. In 1990, neonatal deaths represented 40% of global under-five deaths, compared with 45% today. Of the estimated 5.9 million child deaths in 2015, almost 1 million occur in the first day of life and close to 2 million take places in the first week i.e. Deaths are more concentrated among newborns [3]. This is an urgent call for an increasing focus on newborns for the reason that the neonatal period is the most critical time for the survival of an infant [8].
Early identification of a sick newborn still, has some problems. The clinical features are nonspecific e.g. whether the illness is of infective or metabolic origin; the signs do not help us in differentiating the cause and can be a manifestation of almost any newborn disease. The distinction between variation of normal behavior and early signs of illness becomes more difficult in low birth weight and preterm infants. Neonates are more prone to show subtle signs of illness. Lethargy or difficulty feeding are sometimes the only signs present, which may not be readily recognizable and illness may advance quickly [9,10]. Furthermore, there is overlap in signs and symptoms of the three major causes of death – sepsis, birth asphyxia and complications of prematurity [10,11], as well as with other conditions such as hypoglycemia and hypothermia.
The modified three delays model responsible for newborn death shows that household and health facility related delays were the major contributors to late presentation, treatment initiation and subsequent newborn deaths in many developing countries. These delays especially at the household level are predominantly serious because once there is a delay in the recognition of the danger signs of newborn illnesses there are automatically delays at all other levels i.e. Initiation of appropriate treatment and/or referral to a better resourced hospital etc. [12]. For that reason, reducing neonatal morbidity and mortality requires immediate caregiver’s recognition of suggestive danger signs in the neonates and visiting the nearby clinic [13].
The vast majorities of newborn deaths are preventable, with 73% occurring within seven days of birth, and requires many of the corresponding investments in health systems that are needed to improve maternal health outcomes [14]. Early identification of new born danger signs by caregivers with prompt and appropriate referral serves as backbone of the programs aiming at reduction in neonatal mortality [15].
Although, Ethiopian Demographic Health Survey 2016 [16] showing improvement in under-five child mortality, the knowledge of mothers and caregivers on newborn illness is low and different studies focus mostly on the prevalence of neonatal death and newborn care practice disregard of mothers/caregivers knowledge of neonatal danger sign and their health care seeking behavior which is one of the critical delays for newborn survival.
The newborn cannot explain or express their discomfort and therefore identification as well as diagnosis of illness may be delayed if parents are not intelligent, observant, and concerned. Early detection of neonatal illness is an important step towards improving newborn survival. Maternal recognition of neonatal illness, one of major barriers for optimal care-seeking among neonates during the early neonatal period, was also poor [13].
Mothers are the primary caregivers of the newborn. Consequently, the knowledge of the mothers regarding newborn danger signs has a great influence on the health of the newborn [17]. Expansion of Community Based Newborn Care (CBNC) by health extension workers (hews) in Ethiopia is ongoing and expected to contribute to a decrease in neonatal mortality. However, there is still a gap in availing quality health services such as counseling for newborns health in many facilities and at each service [18].
In Ethiopia, the ministry of health has integrated mother and child information in one booklet (family health card) which is provided to the mother during antenatal clinic and hews use for health education. Information on danger signs have been in cooperated in the family health card for the care provider to advice the mothers and also for the mothers to read. However, various studies in developing countries have demonstrated that despite availability of information on neonatal danger signs on family health card maternal knowledge on the equivalent remain very low [19,20].
Generally neonates and young infants often present with nonspecific symptoms and signs that indicates severe illness. These signs might be present at or after delivery or in a newborn presenting to hospital or develop during hospital stay. Since most babies are born at home or are discharged from the hospital in the first 24 hours, increasing community awareness of the danger signs of newborn and improving care seeking of newborn care is of critical importance for improving newborn survival.
In Ethiopian mothers were recognized as caretakers for the majority of neonates [16], and mothers need to know the danger signs of sick newborn. They can explain these signs to others or family member in a simple language so as to enable them to identify the danger signs and to seek early and prompt medical help. Therefore, improving maternal knowledge concerning neonatal danger sign is a key entry point.
Early determination of health care seeking behaviors of mothers on neonatal danger signs could save the new-born during life threatening complications. Therefore, understanding the factors related to health care seeking behavior for neonatal danger signs are critical for countries like Ethiopia with alarmingly high neonatal mortality. Despite the fact that health-seeking behavior plays a critical role in reducing neonatal morbidity and mortality, studies on the area are limited and inconsistent. Hence, this study was carried out to assess mothers’ knowledge and health care seeking behavior about neonatal danger signs.
New born danger Signs
The “WHO recognized dangers signs” based on WHO definition were categorized as follows: i) Not feeding since birth or stopped feeding; ii) Convulsion; iii) Respiratory rate of 60 or more (fast breathing); iv) Severe chest in drawing (difficulty in breathing); v) Temperature of ≥ 37.5 degree centigrade (fever/hot to touch); vi) Temperature ≤ 35.5 degree centigrade (hypothermia/cold to touch); vii) Only moves when stimulated or not even when stimulated (weakness or lethargy); viii) Yellow soles/yellowness (sign of jaundice); ix) Umbilicus redness or draining pus, skin boils, or eyes draining pus (sign of local infection) [21].
In a full-term baby poor sucking/stopped feeding well, especially in an infant who was feeding well earlier, are very important and sensitive indicators of neonatal illness. Temperature instability is a very important danger signs in neonates. Convulsions happen because of sudden, abnormal electrical activity in the brain. Breathing difficulties indicate serious illness in the new born. An increased respiratory rate (more than 60 per minute) and chest retractions indicate a serious problem. It could be due to pneumonia, hyaline membrane disease, heart failure or malformation. Jaundice in the newborn may be physiological, but when it appears on the first day of life or the skin staining is up to palms and soles or it persists beyond 2 weeks of life, needs investigation and appropriate treatment. Hyper-bilirubinemia in the first week could lead to kernicterus and severe disabilities [9].
Knowledge about neonatal danger signs
Mother’s knowledge of the danger signs of newborn complications is an essential step in the recognition of complications and a way towards reducing neonatal mortality. It is very important to check the newborn for the danger signs of illness as the actions taken to help the newborn are crucial to ensure prompt and safe care. It is also need to teach the mother to look for these signs in the newborn and advise her to seek care promptly if she observes any one of the danger signs [22].
Studies in different countries reported the inconsistency of finding related to level of mothers’ knowledge and related factors about neonatal danger signs. Study done in Tamil, Nadu India shows, 18% of the women were not aware of even one danger sign of new born [23] while other studies shows three and above neonatal danger signs were mentioned among 13.9%, 28.1% and 29.3% of mothers included in the study from India [12,19,24] and four regions of Ethiopia respectively [25].
A study conducted in Uganda on inadequate knowledge of neonatal danger signs among recently delivered women showed that knowledge of at least one of the defined key danger signs was present in 58.3% of all women: however, only 14.8% could name at least two signs. “Fast or difficulty breathing” was the most commonly known danger sign and referred to by almost 30% of the women [20]. Poor suckling or feeding and fever were the newborn danger signs that were frequently mentioned. The knowledge levels on the rest of the danger signs among the respondents were very low [19,20]. The least known danger signs were “convulsions”, “movement only when stimulated” and “hypothermia”, stated by less than 5% of the respondents [20,24].
The study done in Kenya shows majority of mothers 84.5% identified less than three neonatal danger signs. Hotness of the body (fever) was the commonly recognized danger sign by 74.9% postnatal mothers, and 46.6%, 40.1%, 35.3% and 5.8% identified difficulty in breathing, poor sucking, jaundice and lethargy/ unconsciousness as new born danger signs respectively. Only 11.1% and 9.7% identified convulsion and hypothermia as new born danger signs respectively [26].
A study conducted in South-East Nigeria reported that knowledge of more than three of the nine WHO recognized danger sign was poor (30.3%). Majority of the mothers had knowledge of one (i.e. Fever) WHO recognized danger sign (95.2%). Cough, diarrhea and the excessive crying were the most perceived and experienced non- WHO recognized dangers signs among respondents [27].
According to study conducted in Mangalore, India on knowledge on warning signs of newborn illness among 70 mothers, reported that it was found that 62% had good knowledge and 36% of the samples had average knowledge. One percent of the samples had excellent knowledge and one percent of samples had poor knowledge [28].
A study conducted in Northern India on the perception of care giver and health worker about the danger signs of neonatal illness with 200 mothers reported that more than one-third of the caregivers recognized fever, irritability, weakness, abdominal distension/vomiting, slow breathing and diarrhea as danger signs in neonates. Seventy-nine (39.5%) of the caregivers had seen a sick neonate in their own family in the past 2 years. Continuous crying was reported as a common manifestation of neonatal illness and this was supported by the findings of eight key informant interviews with caregivers who had experienced adverse neonatal events [12].
Study conducted in rural Wardha India and peri-urban Wardha, India reported the awareness of mothers regarding newborn danger signs was found to be poor. About 67.2% mothers knew at least one newborn danger signs. Poor sucking, low birth weight, lethargy/ unconsciousness, rapid/difficulty in breathing were known as danger signs to 34.4%, 25.8%, 25.5%, 10.3% mothers respectively, while hypothermia and convulsions were referred as danger signs by only 10.3% and 8.6% mothers respectively [24].
Although Ethiopia has taken great initiative to empower the community to improve neonatal and infant health services at the grass root level, maternal knowledge level about neonatal danger signs, which is a key entry point to improve neonatal health, was found to be low (18.2%). This indicates that nearly 80% of mothers were more likely to delay in deciding to seek care which could intern fires the death of neonates [29].
Factors associated with mother’s knowledge about neonatal danger signs
Home-based neonatal health interventions have promoted recognition of danger signs through prenatal interventions [1,30,31], and Community Health Workers (CHWs) assessed neonates using IMCI algorithms through post-natal routine home visits [30,32].
The high mortality and morbidity rates have been attributed to a significant break in the continuum of care in the service-delivery strategy after delivery. Care during post natal clinic is critical for both the mother and baby to provide the mother with important information on how to care for herself and her child [33].
The study done in Kenya shows, information on neonatal dangers was not provided to 57.2% of the postnatal mothers during their antenatal clinic attendance by the health care providers while education level, PNC accompaniment by spouse, danger signs information to mother, explanation of MCH booklet by care provider during ANC and mother read MCH Booklet were factors positively associated with improved knowledge of neonatal danger sign [26].
Study in the East Mamprusi district of the Northern Region of Ghana, which sought to explore women knowledge of neonatal danger signs, revealed that the poor knowledge was due to the high illiteracy rate among women, and probably explains why neonatal mortality is still high. This study suggests that as part of health education and sensitization, women should be taken through danger signs prior to their discharge from hospital so that they can easily detect signs and rush to health care facilities as and when necessary [19].
These studies from Uganda, Ghana, and India reported the positive effect of birth preparedness, exposure to TV/Radio, and older age of mother to improve the knowledge of maternal and newborn key danger signs [20,24,34]. Women were more knowledgeable than men [35]. In contrast, studies elsewhere have shown that there had been absence of relationship between educational status of mother, birth order, and place of birth, ANC, access for skilled birth attendance, wealth, and parity [20,28].
Furthermore, study conducted in Uganda on inadequate knowledge of neonatal danger signs among recently delivered women and a study conducted in South-East Nigeria on knowledge of the WHO signs showed that there is no significant association seen between knowing at least one danger sign and any socio-demographic characteristic were found [20,27].
Along with, the utilization of the MCH booklet was found to be insufficient by the mothers attending well baby clinic and only 59% of them were explained the contents of the booklet by the health care providers and up to 33.5% of the mothers did not read the instructions in the MCH booklet [26].
The study done in North West Ethiopia reports that the odds of having good knowledge was positively associated with mother’s (AOR=3.41, 95% CI 1.37, 8.52) and father’s (AOR=3.91, 95% CI 1.23, 12.36) higher educational achievement. Similarly, the odds of having good knowledge about neonatal danger signs was higher among antenatal care (AOR=2.28, 95% CI 1.05, 4.95) and postnatal care attendant mothers (AOR=2.08, 95% CI 1.22, 3.54). Besides, access to television was also associated with mothers’ good knowledge about neonatal danger signs (AOR=3.49, 95% CI 1.30, 9.39) [29].
Health care seeking for neonatal danger signs
Health care seeking behavior is not only a matter of knowledge about the cause and treatment of the disease, but also of perceived seriousness and duration, cultural practices and socio-economic status. Delay in recognition of the problem and the decision to seek care is one of the three delays in maternal and newborn health care. Physical distance, financial and cultural barriers to seeking care are compounded when there is a delay in recognizing illness and taking the decision to seek care, especially in rural settings [36]. Such a delay, even if short, can be fatal because neonatal illness generally presents less obviously and progresses more quickly than in older infants [31].
A study in South-East Nigeria reported that healthcare seeking behavior was significantly determined by knowledge of at least one WHO recognized danger sign (OR 4.6 CI 1.1-18.7). The study also revealed that less than half (47.7%) presented to the hospital immediately these signs were noticed and about one in four (23%) did not present to the hospital at all following the delays at the household level [27].
Poor care seeking contribute significantly to high neonatal mortality in developing countries. A study conducted to identify care-seeking patterns for sick newborns in rural Rajasthan, India, reported that 70% of mothers mentioned at least one medical condition during the neonatal period that would have required medical care. However, only 63 (31%) newborns with any reported illness were taken to consult a care provider outside home, while about half of these to an unqualified modern or traditional care provider. In response to hypothetical situations of neonatal illness, families preferred home treatment as the first course of action for almost all conditions, followed by modern treatment if the child did not get better. For babies born small and before time, however, the majority of families did not seem to have any preference for seeking modern treatment even as a secondary course of action [37].
A study conducted in Northern India on the perception of care giver and health worker about the danger signs of neonatal illness shows 23% of respondents sought health care and administered medicines for neonatal illness. According to the study the preferred health-care provider was either a local medical doctor (60.7%), followed by a traditional healer (19.6%) while the remainders were treated with home remedies. Modern medicines were administered to 78.3%, while the rest used indigenous medicine and traditional homemade medicines, either alone or in combination with modern medicine [12].
Study conducted in Wardha India also showed that majority of mothers (87.4%) responded that the sick child should be immediately taken to the doctor but only 41.8% of such sick newborns got treatment either from government hospital 21.8% or from private hospital 20% and 46.1% of sick babies received no treatment [24].
However, a study conducted in peri-urban Wardha, India reported that all sick newborns with danger signs were taken to the doctor and only two mothers consulted faith healer for treatment [24].
Study conducted in Southern Tanzania and study in South Asia Bangladesh reported that mothers discuss issues related to childcare with their female friends, husbands, aunts and other close female relatives. Traditional healers are widely believed to be able to heal sick neonates and are therefore often consulted. Unlike most health facilities they treat on credit, accept payment in kind (exchange of goods for services) and payment rates can be negotiated. Babies with pneumonia, convulsions and any illness associated with spirits and witchcraft are usually taken to traditional healers. Evil spirits were reported as a source of childhood illness in nearly all FGD and in-depth interviews [34,38,39]. Only after these remedies have failed to alleviate the problem do they seek care from health facilities [34].
Factors associated with health care seeking for neonatal danger signs
The most effective strategies to reduce mortality are those that treat the causes of early mortality. Various factors influence the women ability to seek care for their neonates. It has been noted that women’s utilization of maternal and neonatal health services are often influenced by perceived socio-cultural, economic and health system factors operating at the community, household and individual level as well as within the larger social and political environments and health care infrastructure [40].
In a multicenter study by Young Infants Clinical Signs Study Group (YICSG) it was noted that assessment of danger signs resulted in a high overall sensitivity and specificity for predicting the need for hospitalization of a new born in the first week of life and recognizing the occurrence of these signs will results in high overall sensitivity and specificity to predict the need for seeking treatment of the new born [2].
A study conducted in rural Rajasthan, India showed that perceptions of ‘smallness’, not appreciating the conditions as severe, ascribing the conditions to the goddess or to evil eye, and fatalism regarding surviving newborn period were the major reasons for the families’ decision to seek care. Mothers were often not involved in taking this critical decision, especially first-time mothers. Decision to seek care outside home almost always involved the fathers or another male member. Primary care providers (qualified or unqualified) do not feel competent to deal with the newborns [37].
Healthcare-seeking behavior for the newborn is influenced by many factors [7,32]. Common barriers discouraging seeking care for the newborn from formal health facilities include lack of money and lack of reliable transport to the facility [24,38], faith in supernatural causes and remedy was sought from traditional faith healer, ignorance of parents [24] and abusive language by health personnel were mentioned as barriers to neonatal care-seeking [38]. In other study areas, seclusion (restriction) of both mother and baby was reported to be 40 days and families often perceive this as way to protect the child against witchcraft [38].
Furthermore, study in South Asia shows that the reasons families seek initial care from locally available unqualified practitioners, such as traditional healers are traditional beliefs (for example, the influence of evil spirits and harmful effects of allopathic treatments), lack of understanding of the problem, costs of treatment and perceived lack of quality of health services [34].
However, a study done in Lusaka, Zambia on access to a health facility and care-seeking for danger signs in children: before and after a community-based intervention shows long distance to the health facility and low-household income negatively influenced caregivers’ appropriate and timely care-seeking practices at baseline, but 3 years later, after the implementation of a community-based intervention, distance and household income were not significantly related to caregivers’ care-seeking practices [41].
Improving newborn care and newborn health outcomes in Ethiopia will likely require a multifaceted approach. Given low facility delivery rates, community-based promotion of preventive newborn care practices, which has been effective in other settings, is an important strategy. For this strategy to be successful, the coverage of counseling delivered by HEWs and other community volunteers should be increased [25].
In Ethiopia, regarding care seeking for newborns, the problem gets more pronounced. There are multiple cultural attitudes and practices that make care seeking for newborn more challenging e.g. low awareness and knowledge about newborn danger signs, seclusion of mother and newborn influenced by traditional beliefs that they require protection from cold, wind, direct sunlight and evil eye, and also seclusion of the newborn until spiritual blessing and naming by a spiritual leader will occur through the ritual known as ‘hamechisa’ (East Shewa). Local conceptions of newborn illnesses, inadequate recognition of danger signs, utilization of traditional therapy, and lack of financial resources, transportation and appropriate treatment constrain or delay utilization of health facilities for newborn illnesses [42].
According to the study on assessment of ICCM implementation strength and quality of care in Oromia, Ethiopia reasons given by HEWs for why caretakers do no seek appropriate care for newborn illness, 30% mentioned that the community is not aware of services in nearby health post; 23% cited distance from the health post as the reason; 13% wanted injections (they did not know HEWs give curative ICCM/CBNC); and 11% stated that the health post was not always open [8,43]. Moreover, other study in Gedeo zone of SNNP shows residences, educational status of the respondent; delivery and family size were predictors of treatment seeking behavior of mother’s from health center to new born [44].
Conceptual framework
This is the conceptual frame work constructed specifically for this study by the investigator through reviewing and adopting related different literatures.
Study area and period
The study was conducted in Gasera district, Bale zone, Ethiopia from March 12 to April 10 2017. Gasera district is located in the south eastern part of Ethiopia at 484 km away from the capital Addis Ababa and 54 km from Robe Town. It is one of the eighteen districts found in the zone. Currently, the district has 21 rural and 3 urban kebeles (the smallest administrative units) with total households of 20,826 and total population of 99,963 of which 48,724 were female. Based on Gasera district health office report, estimated total number of women of reproductive age (15-49 years) and pregnant women in the district were 22,092 and 3,469, respectively. There are estimated total number of 3,469 and 3,219 live births and surviving infants respectively. A total of 34 health institutions were available in the district: 24 government health facilities (5 health centers, and 19 functional health posts), 8 private clinics and 2 private pharmacy/drug shop (unpublished Gasera District health office report, 2016/17).
Study design
Community based cross sectional study design was conducted.
Source population
Source populations were all mothers of less than one year child in Gasera district
Study population
The study populations were sampled mothers of children less than one year of age during data collection period in selected kebeles of Gasera district.
Sampling unit
List of all household who had mother or caregivers of less than one year child in the kebele.
Study units
Study units were selected mothers or caregivers of less than one year old child in the households.
Inclusion and exclusion criteria
Mothers or caregivers those who were not mentally and physically capable of being interviewed were excluded.
Sample Size Determination and Sampling Procedure
Quantitative study: Sample size was determined by using single population proportion formula. Where, N= minimum sample size required for the study, Z=standard normal distribution (Z=1.96) with confidence interval of 95% and α=0.05, P= prevalence/ population proportion D=design effect (D=1.5), E=is a tolerable margin of error (E=0.05).
Sample size for first objective: Based on the following assumptions: 95% confidence level, finding 29.3% mothers who had knowledge of three or more neonatal danger signs (good knowledge) from previous study done in 4 regions of Ethiopia [25] and a 5% margin of error.
N1=(1.96)2 * 0.293 *(1-0.293) =318, (0.05)2
Multiplying with 1.5 design effect the minimum sample required for first objective was 477. Taking, 5% non-response rate N1 =501.
Sample size for Second objective: Using 95% confidence level, finding proportion of 20% mothers who were decided to seek medical care immediately for neonatal illness from previous study done in Northwest Ethiopia [29] and a 5% margin of error.
N1= (1.96)2 * 0.20 *(1-0.20) =246, (0.05)2
With the above inputs, multiplying with 1.5 design effect the minimum sample required for second objective was 369. Taking, 5% non-response rate N2 =387.
Taking the largest sample size from the first objective, the minimum sample required for quantitative study was Nf=501
Qualitative study
The sample size of qualitative method was determined at saturation of idea.
Sampling technique and procedure
Sampling procedure of quantitative study: All Kebele of Gasera district was stratified into urban (n=3) and rural ones (n=21). Roughly half of the Kebele in each stratum, i.e. one urban and eleven rural Kebele were selected by simple random sampling. The district was implementing Community Health Information System (CHIS) and existing Health Post Family Folder (family-centered tool designed for HEW to be used for data collection, documentation, and management) was used to identify households with mothers or caregivers who had child less than one year prior to the survey. Finally 501 mothers who had child less than one year were selected using the Health Post Family Folder (sampling frame) through the simple random sampling technique with proportionate allocation to size. Data collectors used name of Kebele, their house numbers, and health extension workers for guidance.
Sampling procedure of qualitative Study: For the qualitative study purposive sampling technique was used to select participants for the in-depth interview and focus group discussion (FGD). The participants for in-depth interview were 6 tradition birth attendants and 17 mothers who had experienced neonatal illness in the last one year. The maximum numbers of participants for in-depth interview was decided at the idea saturation. A series of four focus group discussions were carried out among purposefully selected community health workers (health development arms), mothers of small baby and elderly women with eight to ten participants in each group. The focus group discussions kept on till new ideas mentioned and were stopped as repetition of idea occurs
Variables in the study
Dependent variables: Knowledge about neonatal danger signs
Neonatal illness health care seeking behavior of mothers/caregivers
Independent variable:
Socio-demographic and economic factors
• Age of mother and child
• Place of residence
• Maternal marital status
• Occupation of mother and father,
• Family income
• Ethnicity and Religion
• Mother and Father educational level
• Distance from the nearest health facility
• Source of information (exposure to Media)
Health service utilization factors
• Number of children (parity)
• Birth preparedness
• Place and assistant of delivery
• ANC follow-ups and PNC services
• ANC follow-ups and PNC services accompaniment by spouse
• HEWs home to home visit
• Know about nearby HEWs treat newborn illness
• Mother’s awareness about free of charge CBNC treatment by HEWs at HP
• Family health booklet availability and accessibility
• Decision making
Operational definition
• Neonatal period: refers to the first 28 days of life (divided into early neonatal period (first 7 days) and late neonatal period (days 8-28).
• Neonatal danger signs: refer to the presence of WHO recognized neonatal clinical signs that would indicate high risk of neonatal morbidity and the need for early therapeutic intervention.
• Health care seeking behavior for neonatal illness: Mother's/ caregiver's first response for visiting health institutions for medical treatment when their newborn has got neonatal illness. It was measured by looking for answers to health care seeking questions and then categorized as having health care seeking behavior (if participants necessitate seeking care at the health facility) or not having health care seeking behavior (if participants do not initiate care at the health facility.
• Mother or caregiver: Mother of the baby or caregiver of the baby.
• Knowledgeable on key danger signs of newborn: In this research a mother was considered knowledgeable (had good knowledge) if she can mention at least the three WHO recognized nine danger signs for newborn spontaneously [2,33].
• Not knowledgeable on key danger signs of newborn: Mother who did mention less than three WHO recognized nine danger signs for newborn spontaneously [2,33].
• Well birth prepared: defined as having taken at least 3 of the 4 actions (bought childbirth materials, saved money, identified transport, identified skilled provider or health facility).
Data collection instrument and procedure
Data collection instrument: Quantitative data supplemented with qualitative data was used. Quantitative data was collected from selected kebeles starting from March up to April, 2017 by using a structured interview-administered pre-tested Afan Oromo questionnaire. Structured questionnaire was prepared using literatures used in this study and related studies done in different countries. The questionnaire was prepared in English language and then translated to Afan Oromo (local language) and re-translated back to English to check for any inconsistencies. It includes five main segments: - socio-demographic factors, obstetric characteristics, maternal and child health service utilization status, knowledge on neonatal danger signs and health care seeking behavior for neonatal illness.
For qualitative data a semi-structured interview guide and discussion guide consisting of specific questions that was used to gather as much information as possible was designed and used to conduct an in-depth interview and focus group discussion. Semistructured Afan Oromo interview guide and discussion guide was used and translated back to English. Eleven elements of interview guide and eight components for FGD were used.
Data collection procedure
Quantitative data: The purpose of the study was briefly introduced for each of the study participants and data were collected after obtaining a verbal informed consent. The data were collected by trained twelve diploma graduate nurses who are fluent in speaking local language and two public health degree supervisors. Two visits were made for absences in the first visit. The data were collected in the quietest corner of mother’s house where there was no noise and disturbance. The data collection process had taken an average of 20 minutes.
Qualitative data: A discussion guide was prepared, consisting of specific questions that were used to gather as much information as possible. The investigator conducted the in-depth interview using a simple checklist questions to be covered to collect the suggestion of the participants. The points were manually written.
For FGDs the investigator was the moderator, and accompanied by two assistants (2 health professionals for each FGD) who were the note taker and recorder. Sitting arrangement was in a circular manner to allow all participants see each other during focus group discussion. The moderator had introduced himself as well as the note taker and recorder. After the introduction, the discussion was begun. All participants were encouraged to air their views and were treated equally. Each discussion was stopped at the point of idea saturation.
Data quality control
Data quality was assured through careful questionnaire design, pretest and training. One day training about the purpose of the study, the questionnaire in detail, the data collection procedure, the data collection setting and the rights of study participants in detail was given for the data collectors and supervisors. The questionnaire was prepared in English version and translated in to Afan Oromo version and back to English version to check its consistency. After each day of data collection, the collected data were checked for completeness and consistency by holding a meeting with the data collectors. The questionnaire was pre-tested on 5% of the total sample size in Sambitu kebele, Sinana district, which had similar socio-demographic characteristics with Gasera district to minimize ambiguity of words applicability to the local context. Finally, the completeness of the questionnaire was checked before entering data into computer software program and before analysis and interpretation.
Data analysis
Data were entered to Epi Data version 3.1 and then exported to SPSS version 20.0 for analysis. The completeness and consistency of the data were checked and cleaned. Descriptive statistics was used to describe the study population in relation to relevant variables and measures of central tendency were also determined. Bivariate and multivariable logistic regression was done to assess any significant relationship between each independent variable and outcome variable. Crude and adjusted odds ratios were used to ascertain any associations between the dependent and independent variables while significance were determined using a 95% confidence interval. For not losing the most important variables, independent variables with a p-value of less than 0.25 at the bivariate level were included in a multivariable logistic regression model. However, any significant association was determined at a p-value of less than 0.05 in the multivariable logistic regression model controlling for potential confounding variables. The results were presented as odds ratios (OR) with 95% confidence intervals (CI). Finally results were compiled and presented using tables, graphs and texts.
Qualitative data which were from an in-depth interview and FDG were transcribed by arranging the record according to forwarded questions and translated to English. Then thematic data analysis method was used. The notes and the transcribed tape recorded audio data were compiled and coded. The coded data were organized into themes and when necessary the information was presented verbatim in the results. Subsequently comparison was done on the responses of different respondents to identify similarities and differences. Finally, information was linked to its congruence with data obtained from quantitative findings.
Ethical consideration
Prior to data collection appropriate ethical clearance was obtained from the Ethical Review Committee of Madda Walabu University Goba Referal Hospital. Letter of permission was obtained from Gasera district administrative and health office. The participants were informed about the right not to participate or withdraw at any time. Confidentiality of information was maintained by omitting any personal identifier from the questionnaires. Finally, verbal consent was requested from every study participant included in the study during data collection time after explaining the objectives of the study. For this very purpose, a one page consent letter was attached to the cover page of each questionnaire stating about the general objective of the study and issues of confidentiality which were discussed by the data collectors before proceeding with the interview.
Five hundred-one mothers consented to participate in this study out of which 497 were successfully interviewed giving a recruitment fraction of 99.2%.
Socio-demographic characteristics
Of the total respondents, 449 (90.3%) were rural resident and 48 (9.7%) were urban resident. The mean age of respondents was 25.34 (SD ± 5.1) years and the mean age of infants was 16.1 (SD ± 12.8) weeks. Majority of the respondents 415 (83.5%) were Oromo by ethnicity, 317 (63.8%) Muslim, 437 (87.9%) currently in marital union, 380 (76.5%) were house wife, 184 (37.0%) were attended elementary school. Regarding respondent’s husband, 181 (36.4%) and 351 (70.6%) were educated to elementary and occupationally farmers, respectively. The mean of the estimated monthly family income of the participants was 1734.56 (SD ± 1387.70) ETB. Less than half, 42.9% and 19.9% of the mothers had access to a radio and the television, respectively (Table 1).
| Variable | Frequency | Percent | |
|---|---|---|---|
| Residence | |||
| Urban | 48 | 9.7 | |
| Rural | 449 | 90.3 | |
| Mother Age (years) | |||
| ≤20 | 101 | 20.3 | |
| 21-25 | 166 | 33.4 | |
| 26-30 | 152 | 30.6 | |
| >30 | 78 | 15.7 | |
| Child Age (weeks) | |||
| <4 weeks | 119 | 23.9 | |
| 5-24 weeks | 246 | 49.5 | |
| >24 weeks | 132 | 26.6 | |
| Child Sex | |||
| Male | 245 | 49.3 | |
| Female | 252 | 50.7 | |
| Religion | |||
| Orthodox | 174 | 35.0 | |
| Muslim | 317 | 63.8 | |
| Protestant | 6 | 1.2 | |
| Ethnicity | |||
| Oromo | 415 | 83.5 | |
| Amhara | 80 | 16.1 | |
| Others* | 2 | 0.4 | |
| Marital Status | |||
| Married | 437 | 87.9 | |
| Not married | 16 | 3.2 | |
| Divorced/separated | 34 | 6.8 | |
| Widowed | 10 | 2.0 | |
| Educational Status of the Mother | |||
| Unable to read and write | 175 | 35.3 | |
| Read and write | 82 | 16.5 | |
| Grade1-8 | 184 | 37.0 | |
| Grade 9-12 | 25 | 5.0 | |
| College and above | 31 | 6.2 | |
| Educational Status of the Father | |||
| Unable to read and write | 122 | 24.6 | |
| Read and write | 109 | 21.9 | |
| Grade1-8 | 181 | 36.4 | |
| Grade 9-12 | 38 | 7.6 | |
| College and above | 47 | 9.5 | |
| Occupation of the Mother | |||
| Housewife | 380 | 76.4 | |
| Farmer | 44 | 8.9 | |
| Government employee | 45 | 9.1 | |
| Private employee | 11 | 2.2 | |
| Merchant | 15 | 3.0 | |
| Others** | 2 | 0.4 | |
| Occupation of the Father | |||
| Farmer | 351 | 70.6 | |
| Government employee | 71 | 14.3 | |
| Private employee | 18 | 3.6 | |
| Merchant | 50 | 10.1 | |
| Daily labor | 5 | 1.0 | |
| Others*** | 2 | 0.4 | |
| Total Family Income (ETB), (n=459) | |||
| ≤1500 | 285 | 62.1 | |
| >1500 | 174 | 37.9 | |
| Radio | |||
| Yes | 213 | 42.9 | |
| No | 284 | 57.1 | |
| Radio Listening Frequency (n=213) | |||
| Always | 15 | 7.0 | |
| Often | 39 | 18.3 | |
| Sometimes | 102 | 47.9 | |
| Rarely | 36 | 16.9 | |
| Never | 21 | 9.9 | |
| Television | |||
| Yes | 99 | 19.9 | |
| No | 398 | 80.1 | |
| Television Listening Frequency (n=99) | |||
| Always | 41 | 41.4 | |
| Often | 46 | 46.5 | |
| Sometimes | 12 | 12.1 | |
| Distance from Nearest Health Facility | |||
| <1 hr | 232 | 46.7 | |
| ≥1 hr | 265 | 53.3 | |
Table 1: Socio-demographic characteristics of the respondents in Gasera District, Ethiopia, (n=497) March 12 to April 10.
Obstetric and maternal health service characteristics
Among the interviewees, majority, 452 (90.9%) were attended ANC for their last pregnancy, of whom, 336 (74.4%) attended four and greater than four times. Nearly, more than half (54.3%) mothers were gave their last child birth at home and 130 (48.1%) were attended by traditional birth attendants, while the rest, 140 (51.9%) were by their families. Mothers who lost their children were 76 (15.3%) of whom, more than half 43 (56.6%) were lost at neonatal age. Majority, 360 (72.4) of mother had four and less children with 26.2% being first time mothers. Less than half, (41.0%) of the mothers were well birth prepared whereas only 17.5% were accompanied by their spouses to the antenatal and/ or postnatal care clinic. Only one fourth of the mothers were got health extension worker home to home visit during their last pregnancy and/or post-natal period (Tables 2 and 3).
| Variable | Frequency | Percent |
|---|---|---|
| Age at First Pregnancy (year) | ||
| <20 | 328 | 66.0 |
| 20-29 | 167 | 33.6 |
| ≥30 | 2 | 0.4 |
| Number of Pregnancy | ||
| 1 | 121 | 24.3 |
| 2-4 | 209 | 42.1 |
| ≥5 | 167 | 33.6 |
| History of Abortion | ||
| Yes | 48 | 9.7 |
| No | 449 | 90.3 |
| Parity | ||
| 1 | 130 | 26.2 |
| 2-4 | 204 | 41.0 |
| ≥5 | 163 | 32.8 |
| History of Still Birth | ||
| Yes | 25 | 5.0 |
| No | 472 | 95.0 |
| Total Number of Children | ||
| ≤4 | 360 | 72.4 |
| >4 | 137 | 27.6 |
| Experienced Child Death (loss) | ||
| Yes | 76 | 15.3 |
| No | 421 | 84.7 |
| Age of Child at Death (n=76) | ||
| Within 1 month | 43 | 56.6 |
| Between 1 and 11 month | 19 | 25.0 |
| Between 12 month and 5 years | 14 | 18.4 |
| Planned Pregnancy of Last Child | ||
| Yes | 296 | 59.6 |
| No | 201 | 40.4 |
Table 2: Obstetric characteristic of mothers in Gasera District, Ethiopia, (n=497) March 12 to April 10.
| Variable | Frequency | Percent |
|---|---|---|
| ANC Follow Up | ||
| Yes | 452 | 90.9 |
| No | 45 | 9.1 |
| ANC Visit Frequency (n=452) | ||
| <4 visit | 116 | 25.6 |
| ≥4 visit | 336 | 74.4 |
| Place of Delivery | ||
| Health center | 201 | 40.4 |
| Hospital | 26 | 5.3 |
| Home delivery | 270 | 54.3 |
| Home Delivery Assistant (n=270) | ||
| TBA | 130 | 48.1 |
| Family | 140 | 51.9 |
| PNC Follow Up | ||
| Yes | 225 | 45.3 |
| No | 272 | 54.7 |
| PNC Visit Frequency (n=225) | ||
| <3 visit | 194 | 86.2 |
| ≥3 visit | 31 | 13.8 |
| ANC and/ or PNC Accompanied by Spouse | ||
| Yes | 87 | 17.5 |
| No | 410 | 82.5 |
| Birth Preparedness Practices* | ||
| Saved money | 196 | 39.4 |
| Arranged transportation | 267 | 53.7 |
| Identified skilled birth attendant | 287 | 57.7 |
| Buying delivery materials | 347 | 69.8 |
| Not birth prepared | 77 | 15.5 |
| Birth Preparedness Status | ||
| Well birth prepared | 204 | 41.0 |
| Not well birth prepared | 293 | 59.0 |
| HEW Home to Home Visit | ||
| Yes | 126 | 25.4 |
| No | 371 | 74.6 |
Table 3: Maternal and child health (MCH) service utilization status of mothers in Gasera District, Ethiopia, (n=497) March 12 to April 10.
Access and utilization of family health booklet
Mothers were asked whether they had ever got family health booklet and the presence of the booklet at the home was observed. Only 131 (26.4) mothers had been provided with the standard family health booklet of whom, majority, 92 (70.3%) received during the ANC clinic. However, only 88 (67.2%) of them were explained the contents of the booklet by the health care providers and only 89 (17.9%) of them did read the instructions in their family health booklet. Among the mothers only up to 23.5% were ever informed about neonatal danger signs by care providers (Table 4).
| Variable | Frequency | Percent |
|---|---|---|
| Received Family Health Booklet | 131 | 26.4 |
| Time Family Health Booklet Received (n=131) | ||
| During ANC | 92 | 70.3 |
| During delivery | 13 | 9.9 |
| During PNC | 26 | 19.8 |
| Explanation received on content of family heath booklet from the care provider (n=131) | 88 | 67.2 |
| Read all the instructions in the family health booklet (n=131) | 89 | 17.9 |
| Received information on neonatal danger signs from care providers | 117 | 23.5 |
| Time Information Received on Neonatal Danger Signs from Care Providers (n=117) | ||
| During ANC | 70 | 59.8 |
| During delivery | 19 | 16.3 |
| During PNC | 22 | 18.8 |
| Other* | 6 | 5.1 |
Table 4: Family Health Booklet availability and utilization for mothers in Gasera District, Ethiopia, (n=497) March 12 to April 10.
Maternal knowledge about neonatal danger signs
Of the total respondents, only 129 (26.0%) mothers were knowledgeable about neonatal danger sign.
When asked to list those signs, 88 (17.7%) had no knowledge of any and listed none. One hundred-fifty (30.2%) of the mothers listed correctly at least one of the WHO recognized danger signs. Two, three, four and five danger signs were correctly listed by 130 (26.2%), 79 (15.9%), 32 (6.4%) and 16 (3.2%) of the respondents, respectively while only 2 (0.4%) correctly listed up to six WHO recognized danger signs (Table 5).
| Variable | Frequency | Percent |
|---|---|---|
| Source of Information about Neonatal Danger Sign* | ||
| Health Extension Worker (HEW) | 97 | 32.4 |
| Other health professionals** | 74 | 24.7 |
| Reading family health booklet and/or posters | 63 | 21.1 |
| Mass media | 75 | 25.1 |
| Family/neighbor/friends | 120 | 40.1 |
| Community health worker (health development army) | 64 | 21.4 |
| Others*** | 3 | 1.0 |
| Knowledge Level of Newborn Danger Signs | ||
| None | 88 | 17.7 |
| One | 150 | 30.2 |
| Two | 130 | 26.2 |
| Three | 79 | 15.9 |
| Four | 32 | 6.4 |
| Five | 16 | 3.2 |
| Six | 2 | 0.4 |
| Seven | 0 | - |
| Eight | 0 | - |
| Nine | 0 | - |
| Perceived Cause of Neonatal Illnesses* | ||
| Poor hygiene | 170 | 34.2 |
| Hunger | 57 | 11.5 |
| Coldness | 209 | 42.1 |
| Evil spirit(eye),devil | 338 | 68.0 |
| Trauma/injury | 118 | 23.7 |
| Others**** | 110 | 22.1 |
| Don’t know | 83 | 16.7 |
| Nearby HEW’s Treat Newborn Illness | ||
| Yes | 81 | 16.3 |
| No | 416 | 83.7 |
| Nearby HEW’s Treat Newborn Illness Free of Charge | ||
| Yes | 51 | 63.0 |
| No | 30 | 37.0 |
Table 5: Knowledge about neonatal danger signs among mothers in Gasera District, Ethiopia, (n=497) March 12 to April 10.
Fever and poor feeding (unable to suckle) were the most commonly mentioned neonatal danger signs 247 (49.7%) and 186 (37.4%), respectively whereas coldness (hypothermia) and jaundice were the least known danger signs 16 (3.2%) and 17 (3.4%), respectively (Figures 1 and 2). Mothers also mentioned signs perceived as dangers signs which are not WHO recognized. They include but were not limited to diarrhea, frequent crying, vomiting, cough and abdominal colic.
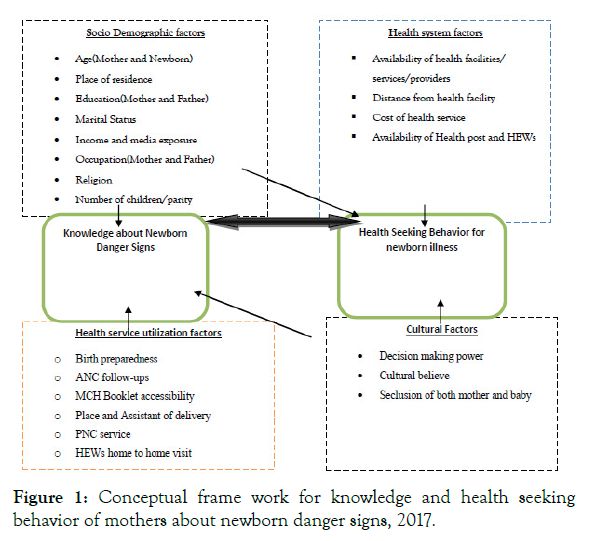
Figure 1: Conceptual frame work for knowledge and health seeking behavior of mothers about newborn danger signs, 2017.
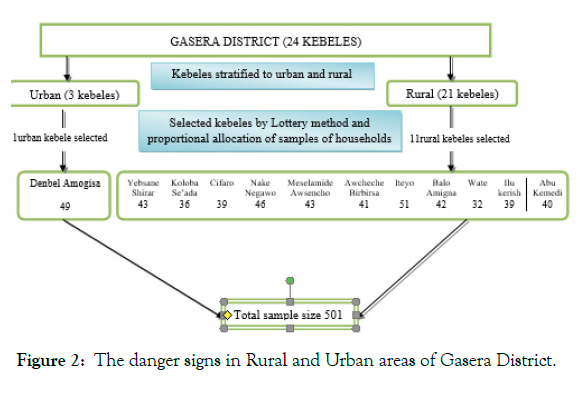
Figure 2: The danger signs in Rural and Urban areas of Gasera District.
Most of the in-depth interview participants mentioned fever, diarrhea, abdominal distension, abdominal colic, tonsillitis, headache, persistent vomiting, unable to suck, fast breathing, frequent crying and cough, as the neonatal danger signs.
A 28 years old mother said that “newborn only express its hunger, pain, and discomfort by crying, therefore, crying is a major sign of any problem the newborn developed”. In addition, a 41 years old traditional birth attendant said that “the newborn baby frequently cry because of abdominal colicky pain which is, beginning, from maternal sickness (ameba) and as well if something left in baby’s abdomen immediately after birth”.
The most common reported source of information (57.1%) was health professionals (health extension workers plus other health professionals) followed by family and friends (40.1%). Majority, of the mothers 338 (68.0%) responded that the cause of neonatal illness was evil spirit (eye) or devil and followed by 209 (42.1%) coldness and 170 (34.2%) lack of hygiene (Figure 3). Only 81 (16.3%) of the respondents know that nearby health extension worker treat and refer neonatal illness, of whom 30 (37.0%) did not know that treatment by health extension worker is free of charge. Majority, of the focus group discussants besides mentioned lack of cleanliness, mother’s health condition, amount of breast milk mother produce, giving other foods or drinks other than breast milk, lack of care and warmth, exposure to cold weather, home delivery, inappropriate positioning and holding a newborn, birth defect and keeping in the sun (hotness) as cause for neonatal illness. A 29 years old mother said that “newborn need care unless they easily develop diseases.” The other, old aged (66 years old), mother said that “evil spirit (eye) and/or devil, bad odor, if mother eat leafy vegetables, if baby stay in the blood during birth and if something left in the baby abdomen after birth the baby became ill.”
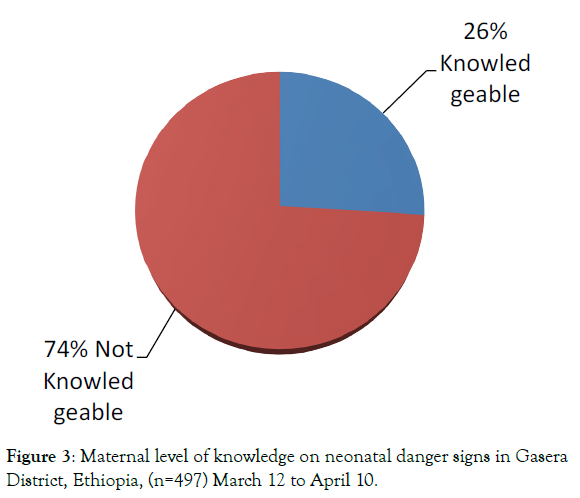
Figure 3: Maternal level of knowledge on neonatal danger signs in Gasera District, Ethiopia, (n=497) March 12 to April 10.
Neonatal danger signs health care seeking behaviors
Three hundred and twenty six (65.6%) of the respondent had previously noticed one or more of the danger signs in their current newborns or children when they were neonates.
Of the 326 mothers who have experienced the perceived and WHO recognized danger signs in their newborns only 182 (55.8%) mothers took their child to the nearby health institution for medical treatment immediately without any home intervention (Figure 4). Only 7 (3.8%) got initial neonatal treatment and referral from nearby health extension workers while majority 107 (58.8%) go treatment from health center and/or government hospital. For those who sought medical treatment, majority 125 (68.7%) were presented delayed to the health facility more than 24 hours after recognition of the danger signs.
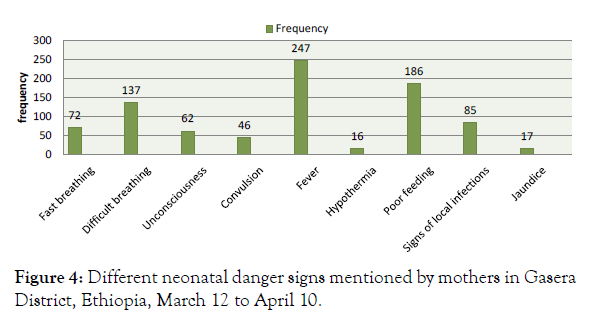
Figure 4: Different neonatal danger signs mentioned by mothers in Gasera District, Ethiopia, March 12 to April 10.
Most FGD and in-depth interview participants label the newborn illness as ‘mitch’, and massage them with a local herb and have them inhale the smoke from burning the leaves, rather than seeking medical care. A 27 year old mother of small baby said that “babies experiencing breathing problems and difficult of passing stool have collapsed intestines from either fallen or not being carried properly and would take to ‘wogesha’ for treatment”.
Among the 144 (44.2%) mothers who did not present to the health facility at all, the most frequent reasons for not taking newborn to the health facility given by the respondents included; perceived no effective treatment is available at health institution (43.1%), thought symptoms is not serious (poor recognition of signs of illness) (31.9%), symptoms resolved without treatment (23.6%), lack of money (15.3%) and long distance or lack of transportation (12.55%). Others include perceived fear of evil eye or devil (9.0%), seclusion of both mother and baby with believe/culture/traditional and/or religious faith (7.6%), and lack of decision autonomy to seek healthcare for newborn (3.5%) (Table 6).
| Variable | Frequency | Percent | ||
|---|---|---|---|---|
| Experienced Neonatal Illness with the Current Child | 326 | 65.6 | ||
| Neonatal Illness Experienced* (n=326) | ||||
| Fever(hot to touch)a | 143 | 43.9 | ||
| Diarrhea/loose stool | 49 | 15.0 | ||
| Continuous excessive crying | 60 | 18.4 | ||
| Breathing difficultya/cough | 86 | 26.4 | ||
| Fast breathingª | 29 | 8.9 | ||
| Lethargy/unconsciousness/weaknessa | 18 | 5.5 | ||
| Inability to feed/sucklea | 73 | 22.4 | ||
| Vomiting | 68 | 20.8 | ||
| Abdominal colic | 30 | 9.2 | ||
| Skin pustule/boil/rasha | 55 | 16.9 | ||
| Convulsiona | 14 | 4.3 | ||
| Tonsillitis | 14 | 4.3 | ||
| LBW/prematurity | 2 | 0.6 | ||
| Abdominal distention | 6 | 1.8 | ||
| Cold bodya | 1 | 0.3 | ||
| Jaundicea | 1 | 0.3 | ||
| Bulging fontanel | 1 | 0.3 | ||
| Source of Medical Treatment (n=182) | ||||
| Government health institution (health center or hospital) | 107 | 58.8 | ||
| Health post | 7 | 3.8 | ||
| Private clinic | 56 | 30.8 | ||
| Pharmacy/drug store | 12 | 6.6 | ||
| Reason for Not Seeking Medical Treatment* (n=144) | ||||
| Perceived sickness is incurable | 7 | 4.9 | ||
| Symptoms is not serious (poor recognition of signs of illness) | 46 | 31.9 | ||
| Symptom resolved without treatment | 34 | 23.6 | ||
| Do not know where it could be treated | 5 | 3.5 | ||
| No effective treatment is available at health institution | 62 | 43.1 | ||
| Perceived lack ability of primary care providers in the health centers in treating newborn illness | 11 | 7.6 | ||
| Lack of money (cost) | 22 | 15.3 | ||
| Long distance/lack of transportation | 18 | 12.5 | ||
| Seclusion of both mother and baby due to fear of evil eye or devil and culture | 24 | 16.6 | ||
| Decision making problem | 5 | 3.5 | ||
| Other*** | 14 | 9.7 | ||
| Time Took to Seek Medical Treatment for Sick Newborn (n=182) | ||||
| Within 24 hr | 57 | 31.3 | ||
| More than 24 hr | 125 | 68.7 | ||
| Reason for Delayed Health Care Seeking for Newborn* (n=125) | ||||
| Did not know that it is a danger sign (poor recognition of signs of illness) | 37 | 29.6 | ||
| Health facility is far and/or lack of transportation | 32 | 25.6 | ||
| Lacked money | 16 | 12.8 | ||
| Thought the child would get better | 89 | 71.2 | ||
| Wanted to try home remedies first | 16 | 12.8 | ||
| Absence of responsible person at the home | 7 | 5.6 | ||
| Newborn didn’t taken to outside in believe/cultural | 8 | 6.4 | ||
Table 6: Neonatal illness health care-seeking behavior of respondents in Gasera District, Ethiopia, March 12 to April 10.
Most of the in-depth interview participants and focus group discussant mentioned major reason for delay for health care seeking was newborn cannot be given any medication, the new born would be got better, lack of awareness about neonatal illness, use home treatments and use of culturally believed treatments. A 26 years old mother said that “I will never take my sick newborn for medical treatment except it is get worse because the small baby can’t abile to take injection”.
A number of FGD discussants mentioned seclusion of both mother and baby up to 40 days due to the norm so called “ulma”. Accordingly, the mother wouldn’t go out of home further up 40 days even if she and/or her baby become ill.
Factors associated with maternal knowledge about neonatal danger signs
After controlling for other socio demographic factors, health service utilization status, and maternal obstetric factors; husband educational status, PNC follow up, birth preparedness, health extension worker home to home visit, receiving family health booklet and mothers’ access for television service were the factors that significantly affect maternal knowledge.
Husband’s with formal education was about 2.33 times (AOR=2.33, 95% CI 1.24, 4.35) more likely to mention at least three neonatal danger signs as compared to husbands with no formal education. PNC service utilization was another statistically significant independent variable for knowledge about neonatal danger signs. A mother having at least one PNC service was about 2.52 times more likely to know danger signs occurring in newborn (AOR=2.52, 95% CI 1.30- 4.92). Similarly, mothers who got health extension worker home to home visit during their ANC and/or PNC were more likely (AOR= 5.45, 95% CI 2.78, 10.70) knowledgeable compared to their counterparts. ‟Before health extension program had started; the community had poor knowledge and attitude towards newborn; for example there was bad attitude that if newborn died we say no matter don’t worry the GOD took itself and it will give again the other health extension worker bought a great deal improvement especially during home to home visit…..”. (In-depth interviewee, TBA).
Moreover, mothers well birth preparedness, receiving family health booklet from health providers and access to television had positive influence on maternal knowledge of newborn danger sign. Those who were well birth prepared during their last pregnancy were three times more likely (AOR=3.04, 95% CI 1.68, 5.52) had knowledge about neonatal danger signs as compared to their complements. Correspondingly, mothers who had received family health booklet from health providers were 7.52 times (AOR=7.52, 95% CI 4.10, 13.82) more likely had good knowledge about neonatal danger signs as compared to those who did not received. As well, mothers’ access to television increased their knowledge about neonatal danger signs nearly by three times (AOR=3.15, 95% CI 1.55, 6.40) (Table 7).
| Factor Variables | Knowledge of Neonatal Danger Sign | COR (95% CI) | AOR(95% CI) | |
|---|---|---|---|---|
| Knowledgeable | Not knowledgeable | |||
| Mother Age (years) | ||||
| ≤20 | 12 | 89 | 0.23 (0.11, 0.49) | 0.32 (0.11,1.01) |
| 21-25 | 43 | 123 | 0.59 (0.33, 1.05) | 0.54 (0.22,1.35) |
| 26-30 | 45 | 107 | 0.71 (0.40, 1.26) | 0.72 (0.29,1.77) |
| >30 | 29 | 49 | 1.00 | 1.00 |
| Mother Education | ||||
| Not formal education | 48 | 209 | 1.00 | 1.00 |
| Formal education | 81 | 159 | 2.22 (1.47,3.35) | 1.28 (0.52,3.13) |
| Father Education | ||||
| Not formal education | 37 | 194 | 1.00 | 1.00 |
| Formal education | 92 | 174 | 2.77 (1.79,4.27) | 2.33 (1.24,4.35)** |
| Television Access | ||||
| Yes | 63 | 36 | 8.80(5.41,14.33) | 3.15 (1.55,6.40)** |
| No | 66 | 332 | 1.00 | 1.00 |
| Distance from Nearest Health Facility | ||||
| <1 hr | 76 | 156 | 1.95 (1.30, 2.93) | 1.15 (0.61,2.17) |
| ≥1 hr | 53 | 212 | 1.00 | 1.00 |
| ANC Follow Up | ||||
| Yes | 117 | 335 | 6.25(1.48,26.45) | 1.11 (0.19,6.58) |
| No | 12 | 33 | 1.00 | 1.00 |
| Place of Delivery | ||||
| Home | 24 | 246 | 1.00 | 1.00 |
| Health facility | 105 | 122 | 8.82(5.38,14.45) | 1.62 (0.65,4.04) |
| PNC Follow Up | ||||
| Yes | 105 | 120 | 9.04(5.52,14.82) | 2.52(1.30,4.92)** |
| No | 24 | 248 | 1.00 | 1.00 |
| Birth Preparedness | ||||
| Well prepared | 91 | 113 | 5.40 (3.48, 8.38) | 3.0 (1.68, 5.52)** |
| Not well prepared | 38 | 255 | 1.00 | 1.00 |
| HEW Home Visit | ||||
| Yes | 79 | 47 | 10.79(6.75,17.2) | 5.45(2.78,10.7)** |
| No | 50 | 321 | 1.00 | 1.00 |
| Received Family Health Booklet | ||||
| Yes | 92 | 39 | 20.9 (12.6,34.7) | 7.52(4.1,13.82)** |
| No | 37 | 329 | 1.00 | 1.00 |
Table 7: Factors associated with mother’s good knowledge about neonatal danger signs, Gasera District, Ethiopia, March 12 to April 10.
Factors associated with health care seeking behavior for newborn danger signs
The independent variable child sex was statistically significant for neonatal illness medical health care seeking; as compared to a woman having female child, a woman having male child was more likely (AOR=1.86, 95% CI 1.09, 3.17) seek medical care. Mothers who had PNC follow up were more likely to seek medical care for newborn illness than those who cannot had PNC during their last child (AOR=2.24, 95% CI 1.24, 4.05). Similarly, mothers who received family health booklet from health care providers were three times (AOR=3.04, 95% CI 1.38, 6.70) likely to seek neonatal medical health care than their counterparts. Furthermore, neonatal danger sign knowledgeable mothers were nearly three times (AOR=2.56, 95% CI 1.18, 5.54) more prone for neonatal illness medical care seeking than not neonatal danger sign knowledgeable counterparts. Also, family monthly income has positive significant association with health care seeking (Table 8).
| Factor Variables | Medical Health Seeking Behavior | COR (95% CI) | AOR (95% CI) | |
|---|---|---|---|---|
| Treatment Sought | Not Treatment Sought | |||
| Child Sex | ||||
| Female | 80 | 84 | 1.00 | 1.00 |
| Male | 102 | 60 | 1.78 (1.15,2.77) | 1.86 (1.09, 3.17)** |
| Mother Education | ||||
| No formal education | 84 | 91 | 1.00 | 1.00 |
| Formal education | 98 | 53 | 2.00 (1.28,3.13) | 1.42 (0.67,2.97) |
| Father Education | ||||
| No formal education | 75 | 79 | 1.00 | 1.00 |
| Formal education | 107 | 65 | 1.73 (1.11,2.79) | 0.76 (0.44,1.32) |
| Total Income | ||||
| ≤1500 | 89 | 104 | 1.00 | 1.00 |
| >1500 | 79 | 28 | 0.30 (0.18,0.51) | 2.10 (1.15, 3.81)** |
| Television | ||||
| Yes | 79 | 27 | 3.32 (1.99,5.54) | 1.71 (0.93,3.15) |
| No | 103 | 117 | 1.00 | 1.00 |
| PNC Follow Up | ||||
| Yes | 149 | 82 | 3.41 (2.07, 5.63) | 2.24 (1.24, 4.05)** |
| No | 33 | 62 | 1.00 | 1.00 |
| Planned Pregnancy | ||||
| Yes | 139 | 100 | 1.42 (0.87, 2.32) | 0.88 (0.47, 1.67) |
| No | 43 | 44 | 1.00 | 1.00 |
| Place of Delivery | ||||
| Home | 35 | 66 | 1.00 | 1.00 |
| Health facility | 147 | 78 | 3.55 (2.17, 5.82) | 1.46 (0.58, 3.67) |
| Birth Preparedness | ||||
| Not well prepared | 90 | 100 | 1.00 | 1.00 |
| Well prepared | 92 | 44 | 2.32 (1.47, 3.67) | 0.48 (0.44, 1.59) |
| Distance from HF | ||||
| <1 hr | 92 | 53 | 1.75 (1.12, 2.74) | 0.96 (0.55, 1.68) |
| ≥1 hr | 90 | 91 | 1.00 | 1.00 |
| HEW Home Visit | ||||
| Yes | 66 | 14 | 5.28 (2.82, 9.90) | 1.34 (0.58, 3.09) |
| No | 116 | 130 | 1.00 | 1.00 |
| Received Family Health Booklet | ||||
| Yes | 75 | 16 | 5.60(3.08, 10.19 | 3.04 (1.38, 6.70)** |
| No | 107 | 128 | 1.00 | 1.00 |
| Received Information on Danger Signs | ||||
| Yes | 65 | 11 | 6.71(3.38, 13.33 | 1.53 (0.45, 5.49) |
| No | 117 | 133 | 1.00 | 1.00 |
| Know Nearby HEW’s Treat Newborn Illness | ||||
| Yes | 45 | 8 | 5.58(2.54, 12.29 | 0.64 (0.17, 2.38) |
| No | 137 | 136 | 1.00 | 1.00 |
| Knowledge Status of Newborn Danger Signs | ||||
| Not knowledgeable | 110 | 130 | 1.00 | 1.00 |
| Knowledgeable | 72 | 14 | 6.07(3.24, 11.36 | 2.56 (1.18, 5.54)** |
Table 8: Factors associated with respondent’s healthcare seeking behavior for newborn with danger signs, Gasera District, March 12 to April 10. (n=326).
This study was tried to assess mother’s knowledge about danger signs of neonatal illness and their health seeking behavior towards neonatal illness. Accordingly, only 26.0% of the participants had knowledge about newborn danger signs. This finding is slightly lower than the finding from community based study conducted in South-East Nigeria [27], in which knowledge of three and more newborn danger signs was (30.3%). This discrepancy could be attributed to difference in setting. When asked to list those signs, 88 (17.7%) had no knowledge of any and listed none, which was consistent with the study done in Nadu India, where 18% of the women were not aware of even one danger sign [23].
Even though, the Ethiopia Ministry of Health has integrated family health card (booklet) which incorporate information on neonatal danger signs for the care provider to advice the mothers and also for the mothers to read, efforts to increase awareness of the danger signs among health care givers and the parents, this study showed that only 131 (26.4%) mothers received it of whom only 89 (17.9%) read all the instructions on the booklet. The reasons for low (26.0%) maternal knowledge on newborn danger signs in the study area could also be due to small number of mothers received and read instructions on the booklet. This finding is also supported by other studies where despite availability of information on neonatal danger signs on family health booklet maternal knowledge on the equivalent remain very low [19,20].
In this study majority of the mothers (76.5%) had not received any information from the health care workers any time else regarding neonatal dangers signs and this is in line with the study done in Kenya [26], where only 42.8% received information on neonatal danger signs from care provider during ANC follow up.
In the present study the awareness of mothers in Gasera district regarding new born danger signs was found to be poor which is in line with neonatal danger signs knowledge level reported in Tamil Nadu, India [23]. However, compared to previous studies conducted in four regions of Ethiopia [25] and Ghana [19], it is lower although it is higher than the level reported in India [24], Northern Ethiopia [29] and Kenya [26]. The discrepancy might be because of most of the previous studies considered other WHO recognized neonatal danger signs in their studies where as in the current study only the nine WHO recognized neonatal danger signs answered by a mother were used to assess knowledge status which might be the reason for this discrepancy, and also possibly it could be because of time, study setting and cultural differences.
The study further showed that husband education was a significant predictor of mothers’ knowledge about neonatal danger signs. The odds of knowledge about neonatal danger signs were nearly two times good among mothers whose husbands attended formal education and this finding is consistent with study done in Northern Ethiopia [29]. This might be due to the fact that males are decision makers so that if they had education, they can make or support mothers to seek care for newborns by which mothers know newborn danger signs. Whereas, study in Uganda [20] and Kenya [26] shows dissimilarity, possibly due to the cultural differences.
The study also recognized that health extension workers home to home visit creates a good opportunity for the mother to have good knowledge towards neonatal danger signs. Health extension home to home visited mothers were outlying about five times more likely to mention at least three neonatal danger signs as compared to their counterparts. Indeed, this positive association was what the Ethiopia's health policy expects from health extension workers by implementing integrated health extension package for routine home to home visit especially visit for pregnant mother and newborn child. Thus, this finding further strengthens the argument that HEWs contribution at community level improves newborn survival.
Absence of association between maternal education and increased knowledge of newborn danger signs in this study was unanticipated. Besides, in previous studies this particular absence of association was noticed in the study conducted in Uganda [39] and Kenya [26]. On the contrary, most of the previous studies found knowledge of neonatal danger signs was significantly higher among educated women [27] and [29]. The possible explanation for this inconsistency is that the overall understanding of newborn health in this community is very low (26.0%), which does not give more educated mothers much of an advantage.
The study also confirmed that PNC follow up practice creates a good opportunity for the mother to have good knowledge towards neonatal danger sign. Postnatal care attendant mothers were two times more likely to mention at least three neonatal danger sign as compared to their counterparts. However, this finding is different from the study conducted in Uganda [20]. The possible reason for the discrepancy could be PNC packages contain information about neonatal danger signs.
Surprisingly, despite a high ANC attendance and health facility delivery among study participants, increased knowledge of newborn danger signs was not detected neither among women attending the recommended number of ANC visits nor among women using skilled birth attendant at delivery. This finding is in line with the studies done in India [28]. This gives rise to great concern; as previous studies conducted in Northern Ethiopia [29] indicates, by providing structured counseling during ANC and advice during delivery, knowledge of events and danger signs in all phases of pregnancy and neonatal period improved. In view of this finding, the extent and quality of the information given to women at ANC and/or delivery with regard to newborn’s health and what danger signs to look needs significant improvement. This study adds further concerns about the quality of ANC service in study area.
Furthermore, knowing at least three of those signs was significantly associated with being well prepared for birth. This is consistent with the study done on inadequate knowledge of neonatal danger signs among recently delivered women in Rural Uganda [20].
This study also shows significant association between neonatal danger sign knowledge and receiving family health booklet. An increased exposure to media especially television was also increased the knowledge of mothers on neonatal danger signs. Mothers those who had television access were three times more likely knowledgeable than their counterpart and this supports the study conducted in Northern Ethiopia [29] and Ghana [45]. This could be television contains a segment of airtime devoted to teach the community about health issue of mothers and children.
This study also showed that, out of 326 mothers who experienced neonatal danger signs, about 55.8% of mothers sought medical care for their newborn danger signs. This finding was higher than the study done in Enugu state, Nigeria (47.7%) [27] lower than studies in peri-urban of India (92%) [46] and Pakistan (81.1%) [47]. These discrepancies might be due to the difference in social environment that does not encourage health care seeking behavior towards neonatal danger signs and differences in accessibility of health facilities.
The study revealed that knowledge of at least three danger signs in the newborn considerably increased the likelihood of mother to seek care in health facilities nearly three times. This is aligned with the study done in Nigeria [27]. However this study shows only 31.3% of mothers with sick newborn sought medical treatment immediately within 24 hr. The implication of poor knowledge was reflected in the fraction of mothers with experience of these signs in their sick newborn who sought care in health facilities immediately the danger signs were observed in this study.
Mothers who had PNC follow up were 2.24 times more likely to seek medical care for newborn illness than those who cannot have PNC during their last child. Thus, this finding further strengthens the argument that increasing PNC improves mother’s health care seeking behavior towards neonatal illnesses. Strength and limitation of the study.
Strength of the Study
• This study tried to minimize selection bias by employing community based study with probability sampling method.
• As this study is conducted at community level, it has the opportunity to collect the opinion of participants at grass root level and device mechanism to improve the services to the satisfaction of the community.
• Moreover this study includes qualitative method basically to support quantitative method to come about with details of the problems.
• Recall bias may be introduced due to study participants were mothers with <12 month infants.
• Even though the community-based nature of the study improves the generalizability of the study, its cross-sectional nature affects the establishment of the cause and effect relationship between maternal knowledge, health seeking behavior regarding the danger signs and the factors that were identified.
This study showed low level of knowledge about neonatal danger signs among women in Gasera district. Along with, it reviled that the main predictors of knowledge about neonatal dangers sign were husband educational status, postnatal care follow up, health extension workers home visit, birth preparedness, receiving family health card and accessibility of television. More than half of the mothers sought medical treatment for their newborn, while only one third sought immediate medical treatment within 24 hour. Knowledge of at least three danger sign, income of the respondent, PNC follow up and receiving family health booklet were predictors of treatment seeking behavior of mother’s from health facility to new born.
Citation: Wanamo TE, Dessalegn FN, Debebe W (2021) Assess the Level of Knowledge and Health-Care Seeking Behavior about Who Recognized Neonatal Danger Signs and Associated Factors among Mothers in Gasera District, Ethiopia. J Adv Dairy 9:583.
Received: 09-Sep-2021 Accepted: 25-Sep-2021 Published: 30-Dec-2022 , DOI: 10.35248/2329-888X.21.9.583
Copyright: © 2021 Wanamo TE, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.