
Journal of Clinical Trials
Open Access
ISSN: 2167-0870

ISSN: 2167-0870
Research Article - (2021)
Aim: Early recognition of high-risk malnourished patients is important for optimization of nutritional status leading to better outcomes. The accurate recording of Malnutrition Universal Screening Tool (MUST) results is vital in this regard. This Quality Improvement Project (QIP) aimed to review the quality of nutritional assessment of emergency laparotomy patients against the National Institute for Health and Care Excellence (NICE) guidelines and outline area of improvement.
Methods: The QIP was conducted at Royal Oldham Hospital in 2019-2020 over a seven-month period. Fifty random patients were included in the first audit cycle over a 4-month period, followed by implementation of recommended changes and a reaudit of 30 patients over a 2-month period. The initial MUST scores which were calculated and documented by nursing staff were identified as the Nursing Staff MUST Score (NSMS). To assess the accuracy of NSMS, we developed a MUST rescoring method which was performed by a senior member of the medical team and was identified as the Medical Team MUST Rescore (MTMR).
Results: The initial audit showed a significant difference between NSMS and MTMR scores. According to MTMR, 23 patients (46%) had an inaccurate MUST score assessment by the nursing staff. A multidisciplinary approach using a standard online calculator was recommended. The second phase of the QIP showed an obvious improvement in the accuracy of MUST assessment. Our interventions improved the accuracy rate of MUST scores significantly (27, 54% vs. 29, 96.6%, P=0.00005).
Conclusion: A multidisciplinary team approach and online calculator are useful in improving the accuracy of MUST assessment in emergency laparotomy patients. This helped early involvement of the dietitian leading to improvement in morbidity and mortality.
Nutritional assessment; Malnutrtion; Nutrtion screening tool; Emergency lapaprotomy
The moment any patient with acute intra-abdominal surgical pathology is admitted to the hospital for treatment; their surgical journey is commenced. This involves clinical assessment followed by delivery of high standard quality care. The aim is always to end this journey with an excellent clinical outcome. Literature review highlights the important role of the Nutritional support in this regard [1].
Nutrition is considered as a significant factor that needs to be assessed and optimized early in surgical patients to ensure high quality care. Most patients who require emergency laparotomy are at a risk of malnutrition, especially the elderly. Nutritional assessment is often unrecognized and under-estimated; this can lead to significant morbidity and mortality. Therefore, early identification of these patients can help to timely refer these patients to the dietitian with consequent improved nutritional status.
The Malnutrition Universal Screening Tool (MUST) is used across the UK for all hospital admissions. Malnutrition Advisory Group and The British Association of Parenteral and Enteral Nutrition (BAPEN) published a report in 2018 which confirmed that MUST could detect malnutrition early and guide action to promote multidisciplinary care with consequent improvement in clinical outcome [2]. The National Institute for Health and Care Excellence (NICE) 2013 Guidelines recommend the use of MUST as a nutritional screening tool in hospitals, primary care and care homes to aid in implementation of the NICE Quality Standard for Nutritional Support of Adults [3].
The sixth report of the National Emergency Laparotomy Audit (NELA) showed that 24,832 laparotomies were performed in England and Wales between December 2018 and November 2019 [4]. All these patients underwent emergency operations for acute surgical pathology such as small bowel obstruction, intraabdominal infection, cancers and bowel ischemia [4]. Majority of these patients fall in the medium to high-risk malnutrition criteria. Emergency laparotomy places a significant physiological stress on the patient. NELA data analysis showed that 75% patients were over 65 and 27% were over 65 and were frail [4].
Acute intra-abdominal surgical pathology can lead to malnutrition which contributes to macronutrient (protein and fat) and micronutrient (vitamin and mineral) deficiencies and sarcopenia [5]. Malnutrition in surgical patients can lead to worse surgical outcomes, increase in the length of stay, in turn increasing the mortality rate [6]. Therefore, early identification and management of the nutritional concerns can improve the surgical outcomes and ultimately reduce the length of stay [7,8].
Despite all the national efforts across UK hospitals to ensure routine nutritional screening is performed on all admissions, National Audit of Small Bowel Obstruction (NASBO) identified that the level of nutritional support remains low [9]. This raises the question of whether malnutrition still appears to be overlooked and not considered as a sufficient medical priority [10].
The aim of this study was to conduct a Quality Improvement Project (QIP) in the form of clinical audit cycle to review our quality of nutritional assessment for emergency laparotomy patients against NICE guidelines and outline areas of improvement. The primary outcome was the assessment of our compliance in completing MUST accurately for all emergency laparotomy patients. The secondary outcome was to assess if our implemented changes could identify and support emergency laparotomy patients who fall in the medium and high-risk criteria of malnutrition.
Standards and guidelines
The NICE guidelines and BAPEN recommendations for screening the risk of malnutrition and management were used for this project. NICE states that screening should assess three variables- Body Mass Index (BMI), percentage of recent unintentional weight loss and acute disease effect. MUST have been approved by NICE as a valid screening tool (Figure 1). In cases where it is not possible to obtain the height and weight measurements, the use of alternative measurements and subjective criteria is recommended [11]. Screening should be repeated weekly for all in-patients.
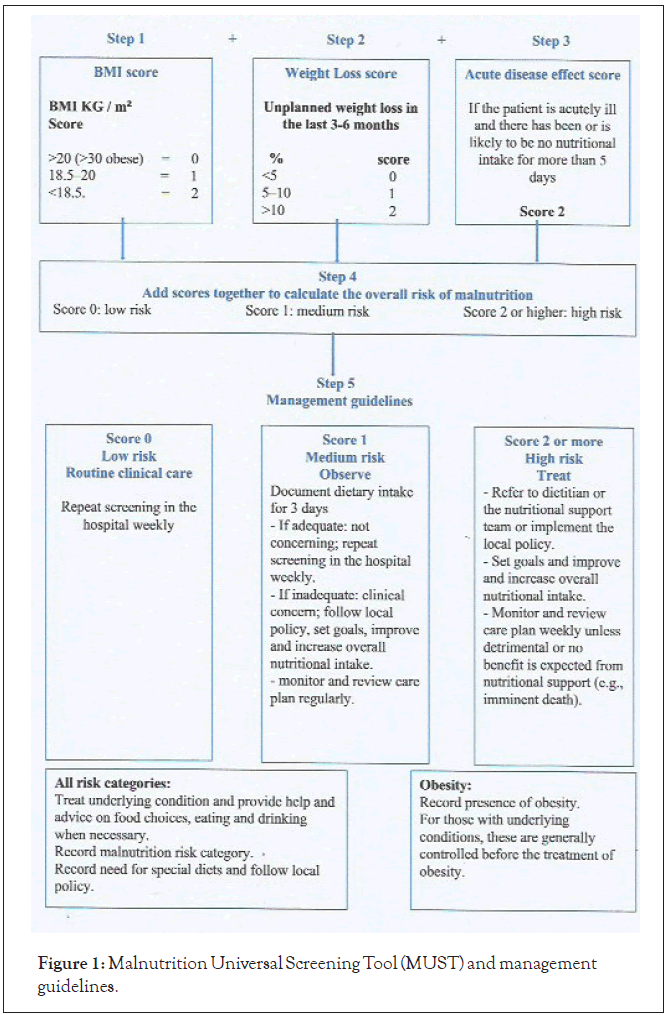
Figure 1: Malnutrition Universal Screening Tool (MUST) and management guidelines.
All patients who underwent emergency laparotomies were included. Fifty consecutive patients were included in the first cycle of this QIP over a 4-month period (1 July 2020-31 Oct 2020), and 30 patients were included in the second cycle over a 2-month period (1 Dec 2020-31 Jan 2021). Data were collected retrospectively using the prospectively maintained NELA Database. Patient demographics were identified and compared between the two cycles.
The primary and secondary outcomes were analyzed by assessing our compliance for each variable of MUST for all patients. The initial MUST scores were recorded by the nursing staff identified as the nursing staff MUST score (NSMS). To assess the accuracy of NSMS, we developed a MUST rescoring method which was performed by a senior member of the medical team and was identified as the medical team MUST rescore (MTMR). The MTMR was used to assess the accuracy of NSMS. We compared the results of both cycles using the appropriate statistical analysis which was performed using SPSS/Excel. Various tests were applied for analysis with a statistically significant p value of 0.05.
This QIP project was registered and approved by the audit department of the Royal Oldham Hospital, UK (Registration Number: 2020 372).
Patient demographics including age, sex, weight, height, BMI, ASA, surgical pathology and type of operation were examined in both cycles, and there was no significant difference between the two groups (Table 1). Interestingly, the results showed that bowel obstruction was the most common surgical pathology that required emergency laparotomy in both groups.
| First cycle | Closed cycle | P-value | |
|---|---|---|---|
| Age (Mean) | 64.1 | 62.1 | P=0.7205 |
| ASA | |||
| ASA 1 | 5 | 3 | P=1 |
| ASA 2 | 22 | 12 | |
| ASA 3 | 15 | 15 | |
| ASA 4 | 8 | 0 | |
| M:F ratio | 21:29 | 11:19 | P=0.6373 |
| Smoking | P=0.7464 | ||
| Smoker | 7 | 5 | |
| Non-smoker | 43 | 25 | |
| Weight (Mean) | 66.4 | 73.4 | |
| Height (Mean) | 164.7 | 163 | |
| BMI (Mean) | 24.5 | 27 | P=0.0777 |
| >20 | 43 | 20 | |
| 18.5-20 | 3 | 6 | |
| <18.5 | 4 | 4 | |
| Surgical pathology | |||
| SBO | 21 | 12 | P=0.8603 |
| LBO | 15 | 5 | P=0.1824 |
| Lower GI perf | 5 | 6 | |
| IBD | 5 | 4 | |
| Upper GI perf | 1 | 2 | |
| Bowel ischemia | 2 | 0 | |
| Intra-abdominal bleeding | 1 | 0 | |
| Necrotising fasciitis | 0 | 1 | |
| Laparotomies | 50 | 30 | |
| Large bowel resection | 24 | 15 | P=0.8624 |
| Adhesiolysis +/- hernia repair | 15 | 7 | P=0.5179 |
| Small bowel resection | 7 | 3 | |
| Per DU repair | 1 | 2 | |
| GS ileus | 1 | 2 | |
| Bleeding control | 1 | 0 | |
| Jejunostomy | 1 | 0 | |
| Debridement and laparotomy | 0 | 1 | |
Table 1: Patient demographics.
First audit cycle
The results showed that our compliance in completing MUST was excellent (100%). Patients were classified into three main categories according to NSMS results: low risk, medium risk and high risk ((12, 24%), (22, 44%) and (16, 32%), respectively).
The medical team examined the accuracy of each variable of the MUST assessment and re-scored the MUST results for all 50 patients using MTMR. The MTMR results were compared to the NSMS results, and this showed that the accuracy rate of height, weight and BMI scores was 100%. In contrast, the weight loss score by the nursing staff was not accurate for 20 patients (40%), either there was no weight loss history taken properly or incorrect assessment was calculated. Moreover, a significant number of patients had their acute disease effect score assessed incorrectly by the nursing staff (23, 46%).
Significant differences between NSMS and MTMR were noted in the first cycle. According to MTMR results, 23 (46%) patients had inaccurate MUST score assessments completed by the nursing staff. Out of these, the malnutrition risk criteria of 15 patients were changed from low or medium to high risk (Table 2). This was demonstrated as the number of patients in the high-risk group increased from 16 (31%) to 31 (62%) based on the results of NSMS and MTMR, respectively. First audit cycle showed significant difference in accuracy of MUST between NSMS and MTMR. (Figure 2). This difference was statistically significant (P=0.00265).
| NSMS | MTMR | |
|---|---|---|
| 1 | 0 (low risk) | 2 (high risk) |
| 2 | 1 (medium risk) | 4 (high risk) |
| 3 | 1 (medium risk) | 2 (high risk) |
| 4 | 0 (low risk) | 2 (high risk) |
| 5 | 1 (medium risk) | 4 (high risk) |
| 6 | 1 (medium risk) | 3 (high risk) |
| 7 | 1 (medium risk) | 3 (high risk) |
| 8 | 0 (low risk) | 3 (high risk) |
| 9 | 0 (low risk) | 2 (high risk) |
| 10 | 1 (medium risk) | 2 (high risk) |
| 11 | 1 (medium risk) | 4 (high risk) |
| 12 | 1 (medium risk) | 2 (high risk) |
| 13 | 1 (Medium risk) | 2 (High risk) |
| 14 | 1 (medium risk) | 2 (High risk) |
| 15 | 1 (Medium risk) | 2 (High risk) |
| 16 | 2 (High risk) | 3 (High risk) |
| 17 | 2 (High risk) | 4 (High risk) |
| 18 | 3 (High risk) | 4 (High risk) |
| 19 | 2 (High risk) | 3 (High risk) |
| 20 | 3 (High risk) | 4 (High risk) |
| 21 | 3 (High risk) | 6 (High risk) |
| 22 | 3 (High risk) | 6 (High risk) |
| 23 | 2 (High risk) | 4 (High risk) |
Table 2: First audit cycle demonstrates difference between NSMS and MTM.
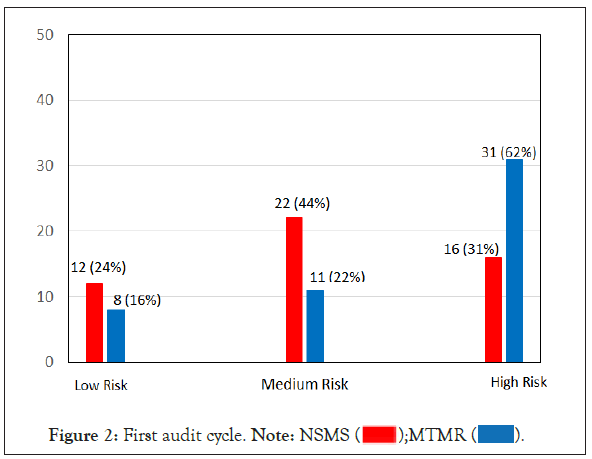
Figure 2: First audit cycle. Note: NSMS
On further assessment, we noticed that all patients who required nutritional support were referred to a dietitian (42 patients, 84%). However, only four patients (8%) were referred to a dietitian before the operation (Mean: 4 days pre-operation) based on the admission MUST score, whereas the remaining patients were referred post- operation (Mean: 3.5 days post-operation). The statistical analysis showed a significant difference between the two groups with a significant delay in referrals to dieticians (95% Confidence Interval: 5.71-9.29, P=0.0001).
Recommendations: Following the first cycle the results were presented at the departmental governance meeting. It was recommended to regularly use the online BAPEN MUST calculator as an assessment tool. An online training session was organized for the clinical staff including doctors to ensure accurate use of the calculator and avoid any bias. Another recommendation was to initiate a multidisciplinary team (nursing staff, medical team and dietitians) approach in screening in the emergency laparotomy patients. These interventions were implemented within 2 weeks.
QIP (Re-audit cycle)
One month after implementing the changes in practice, the second phase of the QIP was performed by closing the audit loop. The results showed that our compliance in completing the MUST assessment remained at 100%. Out of 30 patients, 27 were at a high risk for malnutrition (27, 90%) and only three (3, 10%) patients were at a medium risk.
All initial NSMS scores were completed with input from the medical team using the multidisciplinary approach and the online MUST calculator. Same methodology was followed for assessing the accuracy of MUST scores by re-examining and re-scoring each variable of MUST for all 30 patients.
The results showed that the accuracy rate of height, weight and BMI scores was 100%. There was a significant improvement in the accuracy of the weight loss score as only one patient did not have an accurate assessment (3.3%). In addition, the accuracy of the acute disease effect scores significantly improved as the reassessment showed that there were no patients in this cycle that had an incorrect acute disease score.
The results of this cycle showed an obvious improvement in the accuracy of MUST assessment as there was no significant difference between the NSMS and MTMR results. Only one patient had an inaccurate MUST score assessment. However, there were no patients whose malnutrition risk criteria changed. Second audit cycle showed no significant difference in accuracy of MUST between NSMS and MTMR (Figure 3).
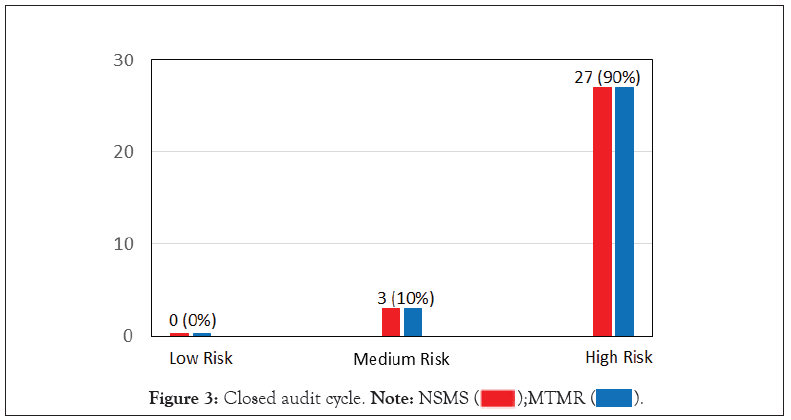
Figure 3: Closed audit cycle. Note: NSMS
On further assessment, 16 patients (53.3%) were referred pre- operatively to a dietitian (Mean: 2.67 days pre-operation), whereas 14 patients (46.7%) were referred post-operatively (Mean: 1.29- day post-operation). The statistical analysis showed a significant improvement in early peri-operative referrals to dieticians (95% Confidence Interval: 3.00-4.91, P=0.00001).
Malnutrition remains a significant problem encountered by a proportion of surgical patients and may directly affect or even complicate their inpatient stay [12,13]. Hospitalised patients, regardless of their Body Mass Index (BMI), typically suffer from malnutrition because of their propensity for reduced food intake due to illness-induced poor appetite, gastrointestinal symptoms, reduced ability to chew or swallow or nil by mouth status for diagnostic and therapeutic procedures [14].
Inadequate nutritional support has been shown to be associated with worse clinical outcomes in malnourished surgical patients [15- 17], thus highlighting the importance of screening and identifying those patients who are at risk of malnutrition at admission. Early identification and nutritional assessment coupled with adequate and timely implementation of nutritional support have shown to positively affect the functional conditioning of the surgical patient [18-20].
Patients requiring emergency laparotomy who are admitted acutely often have had periods of malnourishment in their peri- operative period due to their underlying surgical pathology. The stress response to surgery encompasses derangements of metabolic and physiological processes that induce perturbations in the inflammatory, acute phase, hormonal and genomic responses [21]. Hypermetabolism and hyper-catabolism occur, leading to muscle wasting, impaired immune function and wound healing, organ failure and death [21].
Our QIP demonstrated that the appropriate utilization and accurate scoring using the malnutrition risk assessment tool in patients undergoing emergency laparotomy could aid in their post-operative recovery and reduction of surgical complications rate by helping the surgical team identify patients who are at risk of malnutrition early and ensuring their nutritional optimization peri-operatively.
There are multiple scoring tools that can be used to assess the nutritional status of a surgical patient, such as MUST, malnutrition screening tool (MST), short nutritional assessment questionnaire (SNAQ) and nutritional risk screening 2002 (NRS-2002). All these screening tools show satisfactory performance and similar accuracy in identifying patients at nutritional risk [22,23]. MUST was developed to identify malnourished individuals in all care settings including primary care, hospitals, nursing homes and care homes, where it has been found to have excellent inter-rater reliability, concurrent validity with other tools and predictive validity [23].
Literature review shows that the use of the MUST screening tool increases the dietician referrals by 30-40% and is subsequently validated by the dietician’s assessments of malnutrition [24]. Moreover, it is an easy and reproducible tool to assess the patient’s nutritional status. In addition, the European Society of Clinical Nutrition and Metabolism (ESPEN) highlighted the importance of using a multi-disciplinary approach in the nutrition screening process which involves hospital management, physicians, nurses, dieticians and logistics and IT personnel [25].
The MUST scores at admission predict the requirement for any in-hospital nutritional support. Clinicians have a responsibility to ensure accurate nutritional assessments are undertaken throughout hospital admission to identify those at risk and institute the appropriate nutritional treatment [26]. The results of this project demonstrated the high prevalence of perioperative poor nutritional status in patients undergoing emergency laparotomy which was not adequately highlighted on admission, this may have resulted in a more complicated hospital journey. Following our recommendations and interventions in the current practice; the accuracy rate of MUST scores has significantly improved between the two cycles (27, 54% vs. 29, 96.6%, P=0.00005). This led to a marked improvement in the average referral time to the nutritional support team; with 53.3% being referred before the laparotomy to the dietitian in the second cycle, whereas only 8% were referred in the first. This difference was statistically significant (P=0.00001).
Our audit is a reflection of how a slight adjustment in the team work can lead to a significant improvement in the quality and accuracy of the MUST score at admission after introducing a multi- disciplinary approach to complete the assessment using the online BAPEN MUST calculator. This improvement led to early dietician referral in our practice, and ultimately, optimal nutrition support starting peri-operatively.
Enteral feeding is considered to be associated with better recovery and less complications and is more cost effective than parenteral nutrition. Therefore, enteral feeding is the most desirable form for surgical patients and critically ill patients [27]. A meta-analysis showed that oral nutritional support during the peri-operative period is associated with a 35% reduction in total surgical complications, which was found to be cost effective [18]. Early enteral nutrition is recommended for critically ill patients. If enteral nutrition is insufficient or fails, parenteral nutrition should be instituted [28].
There are around 30,000 emergency admissions for small bowel obstruction in the UK every year [29]. Our study showed that bowel obstruction is the most common indication for laparotomy, this is consistent with NELA report 2020. These patients are at a very high risk of malnutrition as the majority have reduced oral intake for several days prior to admission, and enteral feeding is contraindicated due to bowel obstruction.
The use of early parenteral nutrition is still debatable. The ESPEN guidelines recommend that practitioners consider initiating parenteral nutrition within 2 days after admission to the intensive care unit (ICU) for patients who cannot be adequately fed enterally [30]. In contrast, the American and Canadian guidelines recommend early initiation of enteral nutrition but suggest that parenteral nutrition not to be initiated concomitantly and be withheld for 1 week [31,32].
A large randomized controlled multicenter trial compared early versus late parenteral nutrition in critically ill adults and showed that patients for whom early enteral nutrition was surgically contraindicated appeared to have a greater benefit from late initiation of parenteral nutrition than other patients [33]. However, other observational studies showed that early achievement of nutritional targets improves the outcome for critically ill patients [34-36].
The results of this QIP confirm that MUST assessment is not only a task for the nursing staff, but also for every healthcare personnel who is looking after the surgical patient. Therefore, a multidisciplinary approach should be used to ensure MUST is completed accurately. Once we perform accurate screening on admission, peri-operative nutrition support can be started and optimised even before the patient undergoes emergency laparotomy. This will lead to our ultimate goal with better surgical outcome.
Finally, we believe that incorporating a malnutrition screening tool such as MUST into the NELA risk assessment calculator will ensure that laparotomy patients receive optimal nutritional support early during admission.
Charef Raslan has leaded the study (designed the study, analysed data including statistical analysis and wrote the article). Feras Tomalieh and Omar Lasheen were involved in data collection. Khurram Siddique has reviewed and edited the article. All authors read and approved the final manuscript.
Funding
No funding was obtained for this research.
Acknowledgements
Not applicable.
Availability of data and material
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Ethics approval/Consent to participate/Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Citation: Raslan C, Tomalieh F, Lasheen O, Siddique K (2021) Assessment of Malnutrition in Emergency Laparotomy Patients: A QIP Highlights Simple Measures to Improve Early Recognition and Optimization of High-Risk Patients. J Clin Trials. S12:005.
Received: 30-Jul-2021 Accepted: 13-Aug-2021 Published: 20-Aug-2021 , DOI: 10.35248/2167-0870.21.s12.005
Copyright: © 2021 Raslan C, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.