Journal of Clinical and Experimental Ophthalmology
Open Access
ISSN: 2155-9570
ISSN: 2155-9570
Case Report - (2023)Volume 14, Issue 6
Introduction: Ocular Ultrasonography (US) can be an important dynamic method in evaluating the inflammatory process of the vitreous humor and its complications in patients with arthritis.
Objectives: To detect uveal changes as well as complications by B-mode US and compare them with Optical Coherence Tomography (OCT) in a patient with Psoriatic Arthritis (PsA) using a soluble anti-Tumor Necrosis Factor (TNF) receptor.
Case presentation: This clinical case included a 64-year-old Caucasian female patient diagnosed with PsA. The patient reported that her visual acuity worsened 3 years ago, with tearing, a sensation of sand, ocular pain, with redness, bilaterally, using methotrexate and etanercept for 18 months. Biometry was used for ophthalmological clinical assessment, US with a 12 MHz high-frequency linear probe for semi-quantitative assessment of 0 to 3 vitreous echoes by Gray Scale (GS), changes in the thickness of the optic nerve sheath and structural damage to the retina by OCT.
Results: The patient presented biometry and US with total detachment of the left vitreous, along with grade 3 changes in vitreous echo by the GS, complications, such as detachment of the vitreous humor and changes in thickening of the optic nerve sheath, with mean 5.5 mm bilaterally. The OCT showed worse retinal thinning on the left in the foveal region, characterized by a decrease in central macular thickness of 212 μm, the presence of a hyper-reflective space at the level of the photoreceptor layer, suggestive of their rupture and worsening of vision.
Conclusion: US detected significant vitritis and complications, seen by GS and confirmed by OCT, through retinal structural damage. Thus, it demonstrated that a fusion protein of the human tumor necrosis factor p75 Fc receptor should also not be indicated for patients with a chronic inflammatory process in the posterior chamber.
B-mode; Ultrasonography; Vitritis; Uveitis
Patients with Psoriatic Arthritis (PsA) may present with more insidious uveitis at the beginning, later in 44%, it may become chronic and active bilaterally. This arthritis causes anterior uveitis, in which the inflammatory process extends to the vitreous chamber, highlighting the existence of the communication zone between the vitreous and the aqueous humor, through which propagation of the inflammatory elements. The inflammatory reaction occurs through floating cells in the vitreous chamber, causing a vitreous haze, in which collections of macrophages are seen in the lower vitreous base and close to the ora serrata, called snowballs, but can also appear as an inferior coalescing plaque of cells, like a fibrous material, called snowbankings [1,2]. Its evolution can lead to complications that include cystoid macular edema, increased intraocular pressure and posterior synechiae.
The diagnosis of intermediate uveitis often becomes difficult when examined by an ophthalmologist. There are some situations that cause opacification of the light-conducting environment, which may not show visualization of the posterior segment of the eyeball.
B-mode ultrasound can detect joint inflammatory processes and is considered very useful in mapping tissue lesions in patients with PsA. This tool has also been adding value in acute and chronic inflammatory tissue damage to the eyeball, answering many questions about the clinical manifestations that affect this important organ, being widely used by ophthalmologists for other situations such as hemorrhages, tumor lesions, detachment of the vitreous humor, etc. The US can show dynamic images with well- defined resolution of the anterior uvea, as well as the presence of exudate findings in the vitreous humor, characterizing findings of vitreous echoes in the posterior chamber, which may characterize intermediate uveitis [3].
The OCT is an examination that can be useful in a variety of eye diseases, in the assessment of damage established by pathological processes that affect the vitreous humor, retina and choroid. The possibility of the uvea being compromised throughout its entire length provides specific findings in each affected area, as well as general changes that can be transient or permanent. Currently, this test is not very accessible, being found more easily in large specialized centers, which makes it expensive for patients. Ocular ultrasound dynamically demonstrates these findings and due to the ease of access to this method, it can be considered useful and viable in the evaluation of this extra-articular manifestation [4].
The aim of this clinical case was to detect uveal changes as well as complications by B-mode US and compare them with OCT in a patient with psorasic arthritis using a soluble anti-TNF receptor.
Patients, clinical and laboratory characteristics and physical examination
This is the case of a 64-year-old white patient, a homemaker, diagnosed with psoriatic arthritis 18 years ago. For 3 years, there has been worsening of visual acuity, with tearing, a sensation of sand, eye pain, with redness, bilaterally, using methotrexate and etanercept for 18 years.
Clinical follow-up assessment was carried out by the Disease Activity in Psoriatic Arthritis (DAPSA) score, clinical skin assessment by the Psoriasis Area Severity Index (PASI). The laboratory tests presented by the patient at the initial consultation were negative rheumatoid factor, 4.36 mg/dl of uric acid; erythrocyte sedimentation rate of 2 mm, serology for hepatitis B, C, HIV, syphilis and the Mantoux test were negative and without changes on the chest x-ray. Joint clinical, ophthalmological and imaging assessments were blind.
Ophthalmological evaluation
Performed by anterior and fundus biomicroscopy, with slit lamp by an ophthalmologist specialized in uveitis. Standardization was carried out by describing the anatomical location and intensity of the uveitis, based on the classification of the Standardization of Uveitis Nomenclature (SUN) group [5].
Ultrasound evaluation
The patient signed the free and informed consent form at the Ultrasound Outpatient Clinic of the Rheumatology of Hospital PUC-Campinas. The patient's ultrasound evaluation was performed by a single rheumatologist with 16 years of experience in examinations. MyLab 50 ultrasound (EsaoteSpA, Sao Paulo, Brazil) with a 12 MHz high-frequency linear probe was used to evaluate the eyes. The ocular ultrasound evaluation was performed with the patient's eyes closed, covered with a large amount of gel and without exerting pressure on the ocular structures; the patient was asked to move their eyes laterally, medially, downwards and upwards; the probe was positioned longitudinally and transversely to the eyelids.
The ocular ultrasound evaluation followed a pre-determined sequence, lasting an average of 5 to 7 minutes, to evaluate all eye structures. Initially, a topographic assessment was performed to locate and determine the shape of any abnormalities. Subsequently, a quantitative assessment of vitreous echoes was carried out and finally a kinetic assessment, which determines the mobility of structures, pathological or not. The high gain in mode B, due to the decrease in dynamic range, is initially used for the purpose of visualizing the vitreous cavity, being reduced as necessary to evaluate the retina, choroid and solid lesions.
The classification of the intensity of the vitreous echoes followed the following classification, according to the presence of these findings in the vitreous humor are grade 0 is no change in the vitreous humor; grade 1 is discrete presence of concentric or diffuse vitreous echoes throughout the entire area of the vitreous humor, corresponding to ≤ 25% of the area, grade 2 is moderate presence of concentric or diffuse vitreous echoes throughout the entire area of the vitreous humor, corresponding to ≥ 50% of the area and grade 3 is intense presence of concentric or diffuse vitreous echoes throughout the entire area of the vitreous humor, corresponding to ≥ 75% of the area. The optic nerve sheath in static image was also measured, 3 mm behind the eyeball. The cutoff value used to consider thickening of the optic nerve was equal to or greater than 5 mm. All still and dynamic images were recorded on external hardware. Eye ultrasound was performed after 18 months of treatment [6].
Assessment by OCT
This imaging method is capable of representing ocular tissues through images resulting from the interference of two arms of light (reference arm and exploring arm), translated by the device as different brightness densities. One of the characteristics of acute inflammation is the increase in capillary permeability that results in the extravasation of inflammatory cells in the anterior chamber and vitreous cavity, which is identified and quantified on OCT through the intensity of the brightness and the presence of hyper reflective points in these locations. Furthermore, edema of the initial part of the optic nerve (neuritis), increased thickness of the choroid and changes in the layers of the inner and outer retina are evidence of acute disease, findings that can be identified by OCT. Another particularity of OCT is the evaluation of findings of chronic inflammation and its complications. These complications include cystoid macular edema and epiretinal membrane formation with or without retinal traction.
Clinical ophthalmological evaluation, without detection of inflammation in the anterior and posterior chamber or other findings for infectious, non-infectious, metabolic diseases. There was total vitreous detachment on the left, also with glaucoma on the left, but without retinal detachment and cataract surgery, bilaterally. There were no changes to the skin, nails or intestines. The assessment of clinical follow-up was carried out by DAPSA equal to 6.54, characterizing mild joint activity, PASI equal to 0. The US showed a significant reduction in floating hypoechoic images in the vitreous chamber of the left and right eyes, characterizing grade 3 of the vitritis, with detachment of the vitreous and increase in the right optic nerve sheath equal to 5.9 mm and left equal to 5.1 mm, respectively as shown in Figure 1. In evaluating the OCT of the right and left eyes, the vitreoretinal interface, it is not possible to observe the posterior hyaloid attached to the macula, the presence of discrete hyper reflective points in the vitreous adjacent to the retina, with a foveal depression present. No changes in the neurosensory and external retina, with slight hyper reflectivity at the level of the photoreceptor layer, suggestive of their disruption. The pigmented epithelium of the retina and choroid was unchanged. The presence of a hyper reflective space at the level of the photoreceptor layer suggests their disruption, worse on the left. In quantitative analysis, the central macular thickness is 247 μm in the right eye and 212 μm in the left eye as shown in Figure 2. At the conclusion of this examination, there was evidence of retinal thinning in the left eye as shown in Figure 3, in the foveal region, with loss greater than 5% and the presence of a mild vitreous inflammatory process (Figures 1-3) [7].
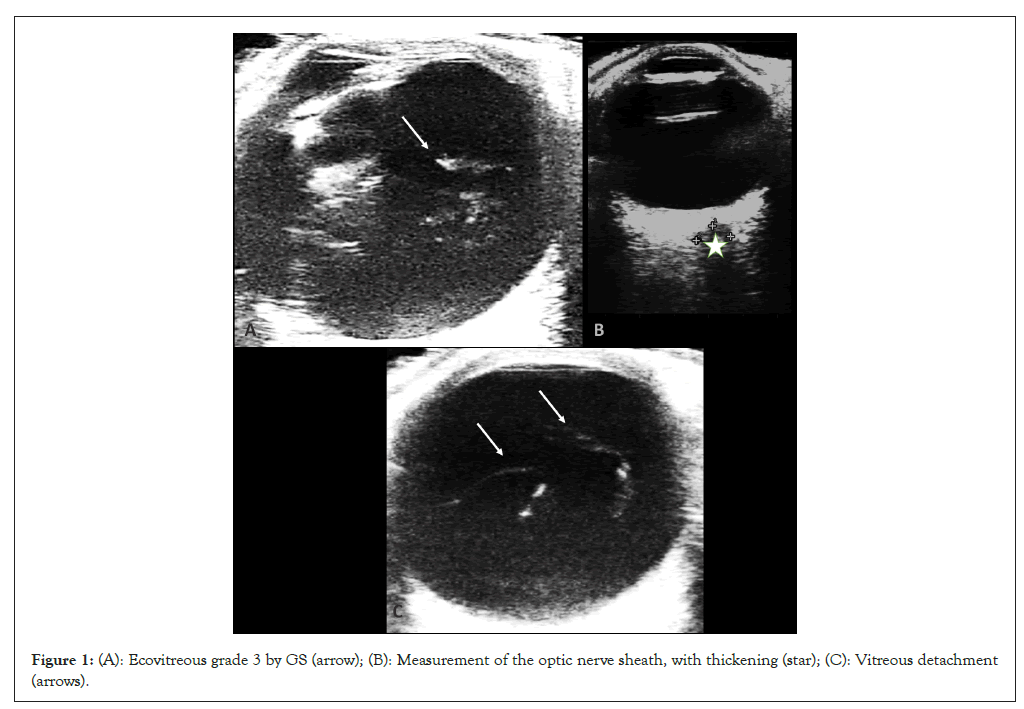
Figure 1: (A): Ecovitreous grade 3 by GS (arrow); (B): Measurement of the optic nerve sheath, with thickening (star); (C): Vitreous detachment (arrows).
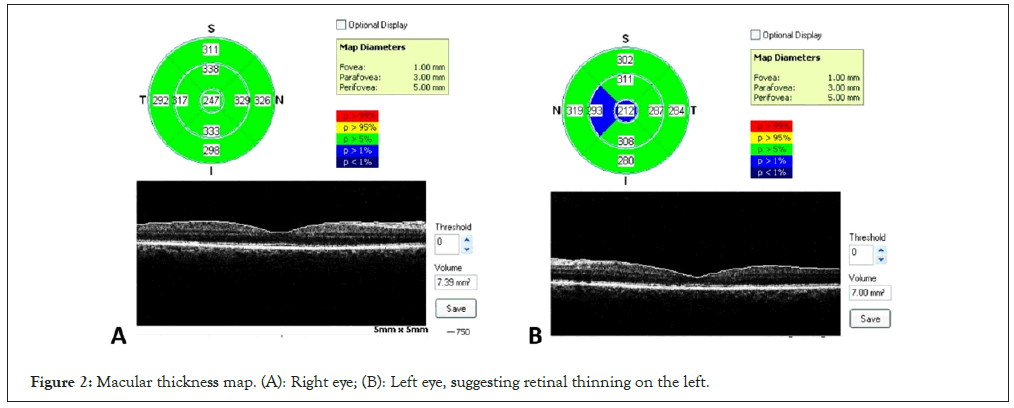
Figure 2: Macular thickness map. (A): Right eye; (B): Left eye, suggesting retinal thinning on the left.
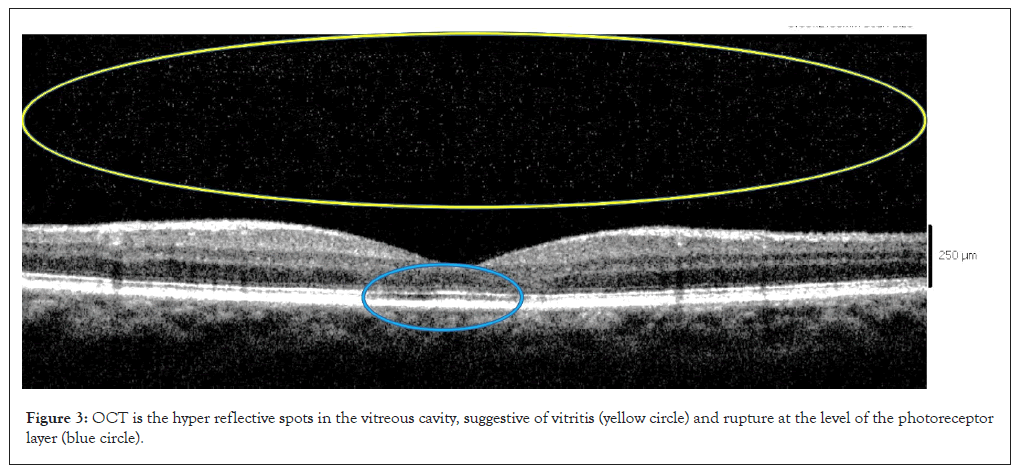
Figure 3: OCT is the hyper reflective spots in the vitreous cavity, suggestive of vitritis (yellow circle) and rupture at the level of the photoreceptor layer (blue circle).
Psoriatic arthritis presents different manifestations of joint involvement, such as oligoarticular in 15% to 40% of patients, polyarticular in 33% to 60%, distal interphalangeal in 8% to 16%, mutilating 5% and axial in 20%, often overlapping between the four groups. Ocular involvement also presents itself differently, as happens in the different joint clinical forms. Ankylosing spondylitis is typically associated with sudden-onset, recurrent anterior uveitis; in juvenile rheumatoid arthritis it is most often associated with a bilateral and insidious disease, with continuous anterior uveitis, in psoriatic arthritis and psoriasis there is a preference for females, with peripheral involvement and in men with axial involvement, the location may be in the anterior chamber or intermediate or posterior, bilateral, chronic and insidious onset. As a differential diagnosis, some causes can be highlighted such as Reiter's syndrome, inflammatory bowel disease, Behcet's disease, Lyme's disease, Whipple's disease, vasculitis, Kawasaki's disease, familial granulomatous uveitis, sarcoidosis, etc. Uveitis represents the third leading cause of vision loss and is responsible for approximately 15% of cases of preventable blindness. Our patient, in addition to presenting chronic ocular inflammation, also had mild joint inflammatory activity, in the same way that in the synovial fluid of the joint, there is the presence of the same cytokines such as TNF-alpha, subtypes of interleukin-17, interleukins 21, 22 and 23. In the aqueous humor and vitreous humor in patients with uveitis, this ocular and joint inflammatory association occurs, which has been studied to better understand the lack of improvement in the extra-articular manifestation, in patients without clinical remission of the joint inflammatory process [8,9]. Anterior uveitis represents very well the acute ocular inflammatory manifestations in patients with arthritis, as it is closely related to the inflammatory process of the joint synovium-enthesal complex, extending to the comparable insertional structure of the ciliary muscle of the ciliary body in relation to the iris, being hypothetically comparable to enthesis and the presence of inflammatory cells in the aqueous humor, which compiles the pathophysiological association between these structures of the eye and the joint. Embryogenesis explains the intimate connection of the ciliary body with the anterior and posterior chamber, in which it is responsible for forming the vitreous humor, through its non-pigmented cellular portion and together with the diffusion process, justified by the existence of a communication zone between the vitreous and aqueous humor. Thus, vitritis is characterized by cellular infiltration in the vitreous body, resulting from any primary inflammation of the vitreous humor or by extension of the inflammatory process originating from other parts of the eye. Manifesting through cells floating in the vitreous chamber, vitreous haze, collections of macrophages seen in the lower vitreous base, near the ora serrata, in the lower coalescent plate of cells and fibrous material.
The classic therapeutic indication by several studies followed by clinical ophthalmological examination of uveitis, is evidenced by the use of humanized monoclonal anti-TNFs, such as adalimumab, cerulizumab, infliximab, golimumab, which characterize the improvement of previous uveitis attacks. The use of an analogue of the tumor necrosis factor p75 Fc receptor, which consists of two soluble TNF receptors combined with the Fc portion of human immunoglobulin G in a way that binds indirectly to TNF and prevents its interaction with inflammatory cells, is not proved to be effective in the treatment of chronic and refractory uveitis, also demonstrated by our patient using this therapeutic class, etanercept, which is effective in arthritis, but not when there is an association with the uveal inflammatory process.
In the patient evaluated, the diagnosis of uveal inflammatory process was not seen at the slit lamp, a method that can be subjective, but it was seen at ultrasound, with greater severity, along with complications, such as detachment of the vitreous humor and changes in thickening of the optic nerve sheath, with mean 5.5 mm bilaterally, but with mild vitreous inflammatory change and chronic structural damage to the retina, reflecting a worsening of left vision, confirmed by OCT. Ocular ultrasound evaluation is a cheap, dynamic and more accessible method than OCT, which can add value in the evaluation of acute and chronic ocular inflammatory processes, such as vitritis, combined with inflammatory arthropathy, as we see in some studies such as clinical cases, observational and systematic review [10].
OCT may be a promising proposal in the future, but there is great difficulty in accessing this method. The US with a linear probe can help in evaluating findings of chronic inflammation in the vitreous humor in patients with arthritis. We know that there are several factors that can mimic an ocular inflammatory condition, such as infections, advanced age that alter the cellularity of the vitreous humor, specialization in the application of ocular ultrasound is of fundamental importance to add value to this tool in patients with arthritis. In this clinical case, the patient is female, with peripheral arthritis and findings of chronic and bilateral uveitis, diagnosed by ultrasound and OCT, together with complications such as glaucoma of the left eye and previous cataract surgery in both eyes, with worsening vision [11].
This clinical case showed for the first time the benefit of B-mode ultrasound in diagnosing a patient with PsA with vitritis and complications, without being in remission of the joint inflammatory process, confirming the OCT findings, adding value to the clinical ophthalmological examination, in treatment failure due to the use of a soluble anti-TNF receptor. There is a great need for new studies, highlighting the complementary use of ultrasound, in relation to clinical ophthalmological examination, mainly adding value to posterior chamber findings, in patients with treatment failure using a soluble immunobiological receptor.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Mendonca JA, Coelho VFN, Nogueira HS, Biselli LG, Nucci LB (2023) Assessment of Uveitis and Complications by Ultrasound in Comparison with Optical Coherence Tomography in Psoriatic Arthritis using Etanercept. J Clin Exp Ophthalmol. 14:964.
Received: 30-Oct-2023, Manuscript No. JCEO-23-28217; Editor assigned: 01-Nov-2023, Pre QC No. JCEO-23-28217 (PQ); Reviewed: 15-Nov-2023, QC No. JCEO-23-28217; Revised: 22-Nov-2023, Manuscript No. JCEO-23-28217 (R); Published: 01-Dec-2023 , DOI: 10.35248/2155-9570.23.14.964
Copyright: © 2023 Mendonca JA, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.