International Journal of Physical Medicine & Rehabilitation
Open Access
ISSN: 2329-9096
ISSN: 2329-9096
Research Article - (2021)
Preventing frailty, sarcopenia, and locomotive syndrome is an important public health issue. Walking exercise has been recommended for the prevention of several diseases and to increase physical activity. We conducted a narrative review of the association between walking exercise and physical function in older community-dwelling individuals in a systematic search of the MEDLINE database for studies in English and CiNii articles in Japanese, published in 2004– 2020. Twenty-five papers were extracted. Our analyses revealed that walking exercise was related to comprehensive physical function, muscle strength, gait speed, physical balance, and exercise capacity. Further investigations are needed to determine the independent associations between walking exercise and frailty, sarcopenia, and locomotive syndrome and to explore the optimal type, frequency, time, duration, and intensity of walking exercise.
Frailty; Sarcopenia; Locomotive syndrome; Physical function
The prevalence of people aged ≥ 65 years is increasing worldwide and is expected to continue to increase [1]. Japan is aging ahead of the rest of the world. According to an announcement by Japan’s Cabinet Office in 2020, it is estimated that social security benefits including pensions, medical care, and welfare are also rising due to the aging [2]. As a countermeasure to this problem, Japan’s Ministry of Health, Labor and Welfare is aiming to extend healthy life expectancy and is promoting long-term care prevention and frailty prevention to prevent decreases in the physical function of Japanese and prevent deterioration to severe illnesses and disorders [3].
Frailty is characterized by a decline in functioning across multiple physiological systems, accompanied by an increased vulnerability to stressors [4]. It can be diagnosed based on the Cardiovascular Health Study (CHS) criteria (five items: muscle weakness, decrease of walking speed, weight loss, lower activity and fatigue) [5]. Frailty is defined as corresponding to 3 out of 5 items. Robust is defined as not having any of the five items. Frailty is six times higher for 3-year survival rate than robust [5]. Frailty is also associated with various risk factors for a poor prognosis, such as an increased risk of falls and fractures, increased loneliness, a decreased quality of life, an increased incidence of depression, decreased cognitive function, an increased risk of hospitalization, and increased likelihood of admission to nursing homes [4].
Sarcopenia, defined as an age-related loss of skeletal muscle mass and muscle weakness and/or a decrease in physical fitness, was reported to significantly increase the limitation of individuals’ physical function for the subsequent 4 years, decrease the walking speed for 7 years, and increase the risk of death for 10 years [6]. ‘Locomotive syndrome’ as described by the Japanese Orthopedic Association has been shown to be a syndrome among middle- aged to elderly individuals that is associated with a high risk of requiring medical services due to decreases in muscle strength and balance associated with aging and locomotor disorders [7]. The prevention of frailty, sarcopenia, and locomotive syndrome in the elderly is thus an important public health issue. Toward this goal, community-dwelling older people need to make efforts to maintain and improve their physical functions as much as possible.
The Health Japan 21 program (now in its second term) recommends physical activity of 10 metabolic equivalents (METs)/hr or more per week for elderly people aged ≥ 65 years to reduce the risk of lifestyle-related diseases, locomotive syndrome, and dementia [8]. The World Health Organization recommends at least 150–300 min of moderate-intensity aerobic physical activity per week or at least 75–300 min vigorous-intensity aerobic physical activity per week [9]. Among community-dwelling older people, those who walk for ≥ 1 hr every day had a lower mortality rate during a 2-year follow-up compared to those who walked for <1 hr/ day [10]. Interventional studies have demonstrated that aerobic exercise (including walking exercise ≥ 2 × /week) for 8–12 weeks by community-dwelling older people had the effects of reducing inflammatory and oxidative gene expressions and improving carotid artery compliance. In other words, walking exercise helps prevent degenerative changes in blood vessels, leading to the prevention of cerebrovascular disease, cardiovascular disease, and premature death [11-13].
In addition, walking is an important exercise for the elderly as it increases the step count number and the amount of activity. Muscle strength training, which is one of the anaerobic exercises, is sometimes difficult to perform for the elderly, because the optimal intensity differs among individuals. Balance exercise is one of the factors that helps increase the risk of falls. As an aerobic exercise, walking can be performed effectively and safely by older individuals if the optimal time and frequency are determined. Walking is easy to spread in all generations.
Building on previous studies targeting community-dwelling older people, we conducted the present review to investigate (1) the precise relationship between walking habits and physical function, (2) the efficacy of walking intervention for improving physical function, and (3) the necessity for walking exercise. We speculated that by identifying the optimal values of parameters such as the type, frequency, and time of walking exercise, it would be possible to determine the most effective walking exercise for older individuals. Our review summarizes the findings of previous research on the relationship between walking exercise and physical functions affecting frailty, sarcopenia, and locomotive syndrome in older people.
The extraction of studies in the Japanese language
We surmised that since the aging of Japan’s society is one of the most significant worldwide, there would be many studies of walking and physical function conducted in Japan. We therefore conducted a literature search of papers in the Japanese language. The database ‘CiNii Articles’ was used as the search database for this purpose. We extracted papers published until October 24, 2020. As the search terms of walking exercise, we used ‘walking’ and ‘exercise and walking,’ and for physical function we used ‘physical function,’ ‘motor function,’ ‘frail,’ ‘sarcopenia,’ and ‘locomotive syndrome.’ As the search term for community- dwelling elderly people, we used ‘community-dwelling elderly people’ or ‘healthy and elderly’ (Figure 1). The extraction of papers was carried out in October 2020, and 506 papers were extracted.
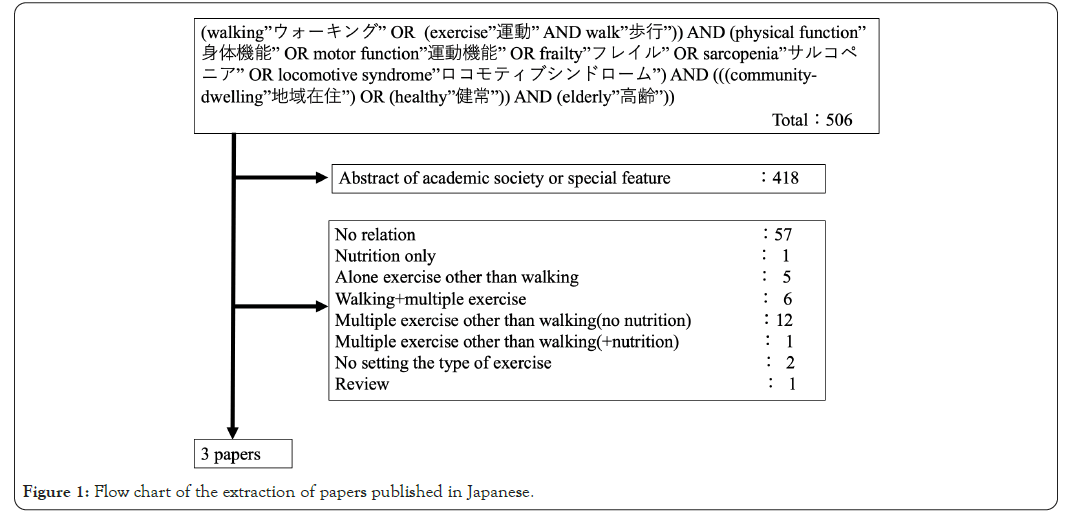
Figure 1: Flow chart of the extraction of papers published in Japanese.
The extraction of studies in the English language
MEDLINE was used as the search database for studies in English. We extracted papers in the PubMed interface of MEDLINE as of October 24, 2020. The search terms used for walking exercise were ‘walking habit,’ ‘habitual walking,’ and ‘exercise and walk’. The search terms for physical function were ‘physical function,’ ‘motor function,’ ‘frail,’ ‘sarcopenia,’ ‘locomotive syndrome,’ and ‘healthy’ or ‘community.’ The search was performed by filtering ‘65 years old and over’ and ‘English only’ (Figure 2). The extraction of papers was carried out in October 2020, and 753 papers were extracted. We included (1) the subjects of the study were community-dwelling older people who were capable of independently performing Activities of Daily Living (ADLs), and (2) the study exposure was only an examination of walking habits or intervention by walking exercise only. Moreover, we exclude (1) the exposure or intervention was a comprehensive exercise intervention that included something other than walking, (2) the outcome was not physical function, and (3) the paper was a review.
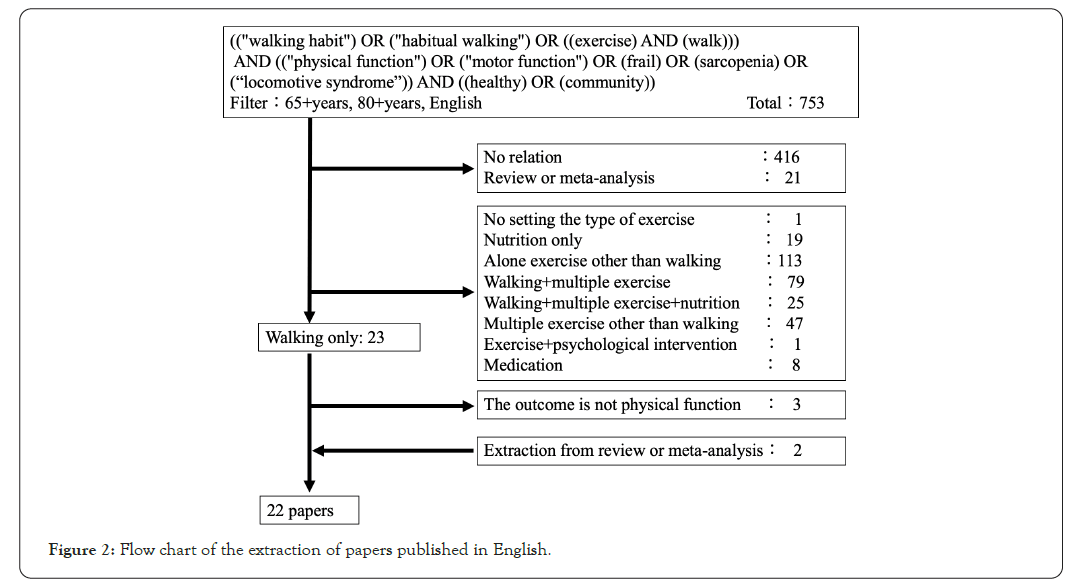
Figure 2: Flow chart of the extraction of papers published in English.
We reviewed cross-sectional studies investigating the relationship between walking habits and physical function (n=5) and 21 longitudinal studies investigating the effects of walking intervention on physical function (including eight randomized controlled trials and one case report).
Outcome measures
The outcomes of the extracted papers included the Medical Outcome Study 36-Item Short-Form Health Survey (SF-36), the SF-12® Health Survey (SF-12), the RAND-36 Health Related Quality of Life (RAND-36 QOL), the Continuous Scale Physical Functional Performance Test (CS-PEP10), and the Short Physical Performance Battery (SPPB), which measure comprehensive physical functions. Other outcomes were muscle strength, walking speed, balance/fall risk, and exercise capacity.
Composition of walking exercise
As shown in Figure 3, the environment settings for walking exercise were outdoor walking in 20 papers (brisk walking, n=2; Nordic walking, n=2) and treadmill walking in six papers. The frequencies of walking exercise were as follows: 1 day/week (n=1), 2 days/week (n=2), 3 days/week (n=10), 4 days/week (n=2), 5 days/week (n=3), daily (n=2), and no settings (n=6). The time per walking session among the papers were as follows: 25 min (n=1), 30 min (n=9), 40 min (n=3), 45 min (n=2), 60 min (n=3), and no settings (n=8). Regarding the walking intensity, 13 papers described an intensity level, and 13 did not. The intervention period was as follows: 3–4 weeks (n=2), 6–8 weeks (n=4), 12 weeks (n=6), 16 weeks (n=2), 20–24 weeks (n=5), and no setting (n=7).
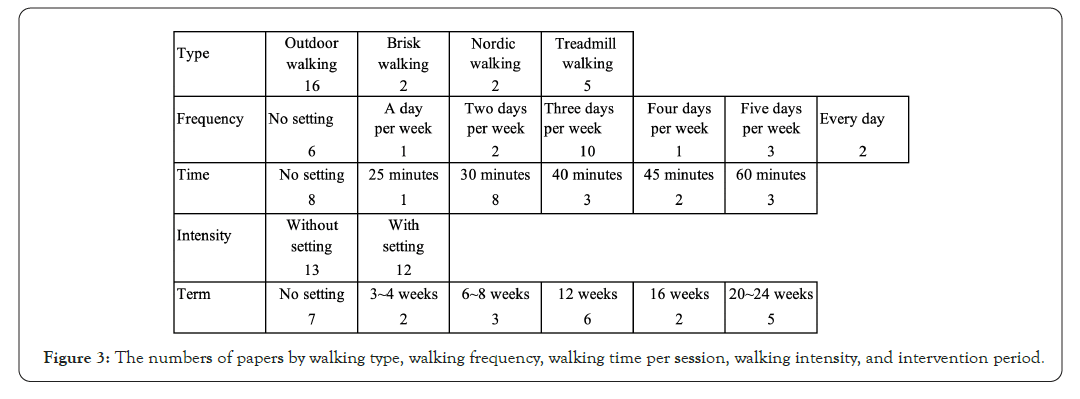
Figure 3: The numbers of papers by walking type, walking frequency, walking time per session, walking intensity, and intervention period.
Frailty, sarcopenia, locomotive syndrome
To the best of our knowledge, there have been relatively few investigations of the association between walking exercise and sarcopenia or locomotive syndrome. Regarding frailty, a single cross-sectional study comparing exercise habits in robust subjects and individuals with pre-frailty was extracted in the present review: Fujiwara et al. reported that the amount of time spent exercising per week was significantly longer in the group of robust subjects compared to the subjects with pre-frailty, and the frequency of engaging in exercise/sports in the prior 1–2 years tended to be significantly higher in the robust group [14]. In addition, the frequency of light walking (‘sampo’ in Japanese) and that of walking exercise (almost never or 1 × /week vs. 2–3 × /week or every day) were not significantly different between the robust and pre-frailty groups [14].
Comprehensive physical function
Three cross-sectional studies reported an association between walking habits and physical function, and seven longitudinal studies described the effects of walking intervention.
The SF-36 measures the Quality of Life (QOL) of the person tested, based on eight items: physical function, daily role function (body), physical pain, overall health, vitality, social life function, daily role function (mental), and mental health [15]. Two research groups reported that the physical function scores on the SF-36 were higher for their subjects who walked daily, and higher for the group of subjects with longer walking times per week [16,17] The SF-12, which is a short version of the SF-36, is a QOL evaluation method that is also based on eight items: physical function, daily role function (physical), physical pain, overall health, vitality, social life function, daily role function (mental), and mental health [18]. Of these, physical function is an item related to ADLs such as bathing and changing clothes, and daily role function (physical) is an item that whether the person tested has experienced problems with their work and/or ADLs due to physical causes in the prior month. Fisher et al. reported that the physical function score on the SF-12 was improved by outdoor walking for 6 months [19].
The RAND-36 QOL questionnaire, another QOL evaluation method, is based on the following eight items: daily role function (physical), daily role function (mental), vitality, mental health, social function, physical pain, and general health [20]. Jyvakorpi et al. reported that the physical function score on the RAND-36 QOL was higher for their subjects whose daily walking involved longer distances [21]. The CS-PEP10 measures physical function based on 10 items including the transportation of heavy objects, housework, climbing stairs, and walking [22]. Moore-Harrison et al. reported that walking exercise for 8 weeks improved their subjects’ scores on the CS-PEP10 [23].
The SPPB evaluates a person’s physical function based on three items: standing balance, 5-times stand-up speed, and 4-m walking speed [24]. Chmelo et al. conducted a 5-month treadmill-walking intervention for community- dwelling obese people, applying gradually increased time and intensity; their subjects’ SPPB scores improved [25]. Improved SPPB scores were also achieved by community- dwelling elderly people after they participated in a 6-week walking intervention in a study by Marsh et al. [26]. It was reported that subjects’ SPPB scores were improved when they received instructions and guidance by telephone and counseling (e.g., about increasing their step-count number) and by an outdoor walking intervention [27]. Nicklas et al. conducted a 12-week walking intervention that involved an increase in the subjects’ walking speed and dynamic walking in a population of community-dwelling older people with limited physical function, and as a result, the subjects’ SPPB scores improved significantly [28].
Muscle strength
Among the papers extracted in this review, six longitudinal studies showed that walking interventions were effective in improving muscle strength. Walking exercise improved the participants’ stand-up speed in a study of treadmill walking for 6 weeks, 25 an investigation of outdoor walking for 16 weeks, [29] and a study comparing a walking exercise group with a balance exercise group [30]. Bieler et al. conducted a 12-month Nordic walking intervention for community- dwelling individuals with Osteoarthritis (OA), and the subjects’ 30-sec chair stand-up test results improved with this intervention [31]. Another study’s 8-week outdoor walking program improved the subjects’ muscle strength in their upper and lower limbs [23].
Gait speed
One cross-sectional study, one case series, and ten longitudinal studies showed that walking interventions were effective in improving gait speed. In the cross- sectional study, it was reported that the subjects who had walking habit of ≥ 2 days/week had a large stride for comfortable walking and a higher maximum gait speed [32] The subjects’ walking speeds were improved by a 16- week self-paced outdoor walking intervention, [29] an 8-week treadmill-walking regimen (in four subjects), and a 6-week treadmill walking program [25,33]. An interesting interventional study of three groups of participants (Nordic walking, nutritional intervention, and Nordic walking+nutritional intervention) observed gait speed improvement only in the Nordic walking-only group [34]. A 3-month-long intervention study with a walking group and a walking+balance exercise group revealed that the gait speed was improved in both groups [30].
Moore et al. started a treadmill-walking intervention for community-dwelling stroke patients immediately after their discharge, and the patients’ usual gait speed was improved by the intervention [35]. The gait speed of subacute stroke patients was improved by a 30%-40% weight-unloaded treadmill walking exercise for 3 weeks in a study by Mao et al. [36] In papers concerning community-dwelling individuals with Parkinson disease, a 6-month walking intervention and a 6-week walking+app management program improved gait speed [37,38]. In other reports, walking exercise improved the gait speed of community-dwelling persons with OA [39] and elderly community-dwelling people with limited physical function [28].
Balance and fall risk
Seven longitudinal studies showed that walking interventions are effective for improving balance. In one cross-sectional study, there was a negative association between walking habit and fall history. In a Randomized Controlled Trial (RCT), the walking intervention was effective for lessening the subjects’ fall risk.
A 16-week outdoor walking intervention improved the extension distance of the participants’ functional reach [29] Outdoor walking exercise has also been reported to improve tandem standing balance [23,30]. Chatterjee et al. stated that Nordic walking for 12 weeks improved the balance score evaluated by the Berg Balance Scale (BBS) [34]. Subjects’ scores on the Timed Up-And-Go (TUG) test improved in a study of community-dwelling OA patients who engaged in a 12-month Nordic walking program, [31] in a study of community-dwelling stroke patients who began a treadmill walking regimen immediately after their discharge, [35] and a study of elderly community-dwelling subjects with limited physical function who was guided walking intervention for 12 weeks [28] In the above-cited study by Mao et al., 3 weeks of treadmill walking with 30%– 40% weight unloading improved the Brunel Balance Rating Scale (BBRS) scores of subacute stroke patients [36] Ginis et al. provided a 6-week program of walking+app management for community-dwelling patients with Parkinson disease, and their scores on the Mini-Balance Evaluation Systems Test (MiniBESTest) improved [38].
Regarding the risk of falls, Okubo et al. [40] reported that a brisk-walking intervention plus walking exercise at home for 12 weeks reduced their subjects’ fall rate and improved their gait ability to avoid obstacles. In that study, the walking exercise was also more effective than balance training. Moreover, in a cross-sectional study, the subjects who had a walking habit for <30 min/day had a high history of falls [41].
Exercise capacity
One cross-sectional study and nine longitudinal studies reported an association between walking habit or walking intervention and exercise capacity. The cross-sectional study reported that the participants who had walking habits of ≥ 2 days/week had a longer 6-min walk distance [32]. In intervention studies, a walking exercise performed ≥ 3 ×/week at comfortable speed [42] and a brisk-walking intervention+ walking exercise performed at home improved the subjects’ 6-min walk distance [40] Treadmill walking for 6 weeks or 24 weeks improved the exercisers’ maximal oxygen uptake and 400-m fast-walk time [25,43].
Bieler et al. supervised a 12-month Nordic walking program for community-dwelling patients with OA and reported that the patients’ 6-min walk distance improved [31] In their study of a 12-week walking intervention with increased walking speed and dynamic walking by older community- dwelling subjects with limited physical function, Nicklas et al. reported that the subjects’ 6-min walk distance improved significantly [28]. Elderly community-dwelling individuals performed a walking intervention for 6 weeks in a study by Marsh et al., and their 400-m walk distances improved [26]. Moore et al. started a 4-week treadmill-walking intervention immediately after discharge for community-dwelling stroke patients, and the patients’ maximum treadmill walking speed improved [35]. The max VO2 of community-dwelling Parkinson disease patients was improved by a 6-month walking intervention in a study reported by Uc et al. [37] (Table 1).
| 1st author [ref] yr | No. of subjects | Age | Subject | Composition of walking | Adjusted factor | Association with physical function | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| Type | Frequency per wk | Time per session | Intensity | Period | ||||||
| Fujiwara [14] 2017 | 114 | â?¥ 60 yrs | Community-dwelling people | Walking habits | Rare, 1, 2â??3, 7 | â?? | â?? | â?? | â?? | In non-flail, the amount of exercise time/wk and the frequency of sports or exercise over the past 1â??2 yrs were significantly higher. The frequency of walking was not significantly different between robust and pre-flail. |
| Bogen [16]Â 2017 | 46 | â?¥ 65 yrs | Community-dwelling people | Walking habits | 7 | â?? | â?? | â?? | Age, sex | Step count per day associated with SF 36-PF. |
| Loh [17]Â 2018 | 5167 | â?¥ 45 yrs | Community-dwelling people | Walking | 0 min, 1â??149 min and â?¥ 150 min/wk | â?? | â?? | Age, education, occupation, income | The time spent walking was associated with physical function score in SF-36. | |
| Fisher [19]Â 2004 | 56 | â?¥ 65 yrs | Community-dwelling people | Walking | 3 | 40 min | â?? | 24 weeks | Age, sex, education, income and race | Physical function score in SF-12 improved. |
| Jyvakorpi [21] 2018 | 394 | â?¥ 82 yrs | Community-dwelling people | Walking habits | 7 | None/<1 km/1â??3 km/ â?¥ 3 km | â?? | â?? | â?? | Walking habit was positively associated with physical function of RAND-36 QOL. |
| Moore-Harrison [23] 2008 | 26 | â?¥ 60 yrs | Community-dwelling people | Walking | 3 | 40 min | 60%â??75% heart rate max RPE12-14 |
16 wks | â?? | Physical function score in CS-PEP 10, upper and lower limb muscle strength, balance of tandem standing position and peak oxygen uptake improved. |
| Chmelo [25] 2015 | 95 | â?¥ 65 yrs | Community-dwelling obese people | Treadmill walking | 4 | 30 min | 65%â??70% heart rate reserve | 6 wks | â?? | Gait speed of 400 m, usual gait speed, stand-up speed, SPPB and peak oxygen uptake improved. |
| Marsh [26] 2009 | 31 | 65ã??85 yrs | Community-dwelling people | Walking | 3 | 25 min | Borg scale 11â??13 | 6 wks | Age, BMI, history of education, marriage, comorbidities, race | 400-m gait distance and SPPB improved. |
| Rosenberg [27] 2012 | 87 | â?¥ 65 yrs | Community-dwelling people | Walking (Instruction to increase step count) |
â?? | mean 3171 steps | â?? | â?? | age, step count, sex, BMI, SPPB and gait ability at baseline | Step count/day, ADLs and SPPB improved. |
| Nicklas [28] 2020 | 49 | Mean 77.7 yrs | Community-dwelling limited function people | Walking (increased gradually, dynamic) |
2 | 60 min | â?? | 12 wks | â?? | 6-min walk distance, SPPB, TUG and usual gait speed improved. |
| Li [29]Â 2005 | 108 | â?¥ 60 yrs | Community-dwelling people | Walking | â?? | Gradually increased from 6 to 30 min | Borg scale 11â??13 | 16 wks | Age, sex, education and health condition | Functional reach test, stand-up speed and gait speed of 50 ft improved. |
| Minett [30]Â 2020 | 85 | â?¥ 70 yrs | Community-dwelling people | Walking | 5 | 30 min | â?? | 12 wks | Age, sex, height and weigt | TUG, gait speed, stand-up speed and balance of tandem standing position improved. Muscular cross-sectional area did not improve. |
| Bieler [31]Â 2016 | 152 | â?¥ 60 yrs | Community-dwelling hip osteoarthritis | Nordic walking | 3 | 60 min | Borg scale 12â??14 | 12 mos | Age, sex | 30-sec chair stand-up test, stair climbing, TUG test and 6-min walk test improved in Nordic walking group. |
| Arai [32]Â 2011 | 51 | â?¥ 65 yrs | Community-dwelling people | Walking habits | â?¥ 2 | â?? | â?? | â?? | â?? | Walking group of â?¥ 2Ã?/wk had a larger stride for comfortable walking, faster max. walking speed, and longer walking distance for 6 min than <2Ã?/wk. |
| Oh-Park [33] 2011 | 4 | â?¥ 70 yrs | Community-dwelling people | Treadmill walking | 3 | 30 min | Borg scale 12â??14 | 8 wks | â?? | Gait speed and step distance improved in all subjects. Knee extensor muscle strength improved in only one. |
| Chatterjee [34] 2018 | 66 | â?¥ 60 yrs | Community-dwelling people | Nordic walking | 3 | 60 min | â?? | 12 wks | â?? | Gait speed, ADLs, IADL, the rate of transition to frailty, and BBS score improved. |
| Moore [35] 2010 | 58 | 50 ± 15 yrs | Community-dwelling stroke | Treadmill walking | 2â??5 | â?? | 80%â??85% heart rate max. and Borg scale 17 | 4 wks | â?? | Peak oxygen uptake, 12-min gait distance, TUG and maximal treadmill gait speed improved. |
| Mao [36]Â 2015 | 24 | Weight unloading treadmill walking group: 59.55 yrs, Walking group: 60.82 yrs |
Subacute stroke patients | Weight unloading treadmill walking | 5 | Gradually increased from 20 to 40 min | 30%â??40% unloaded, Gradually increased from 0.5 mph to 2.5 mph |
3 wks | â?? | FMA-LE and BBRS improved between the groups, and there was no difference between two groups. Gait speed improved in weight unloading treadmill walking group only. |
| Uc [37]Â 2014 | 43 | 50â??80 yrs | Community-dwelling parkinson disease | Walking | 3 | 45 min | 70%â??80% heart rate max. | 6 mos | Training methods, age at intervention | Max. oxygen uptake and 7-m gait speed improved, and functional reach test did not improve. |
| Ginis [38]Â 2016 | 38 | Intervention group: 67.30 yrs, Control group: 66.11 yrs |
Community-dwelling Parkinson disease | Walking+app management | 3 | 30 min | â?? | 6 wks | â?? | The walking speed and 2-min walk test improved in both groups, and there was no difference between the groups. MiniBESTest improved in intervention group only. |
| Wallis [39]Â 2017 | 16 | â?¥ 50 yrs | Community-dwelling knee osteoarthritis | Walking | â?¥ 10 min in a row and 70 min/wk | Borg 3 | 12 wks | Age, sex, occupation, BMI, coronary risk factor, severity of osteoarthritis, part of osteoarthritis and medication | 40-m gait speed improved in walking group significantly compared with control group. WOMAC, QOL, 30-sec chair stand up test did not differ between the two groups. |
|
| Okubo [40]Â 2015 | 75 | â?¥ 65 yrs | Community-dwelling people | Brisk walking | 1Ã?/wk and 3â??5Ã?/wk at home | â?? | â?? | 12 wks | Sex and history of falls | Walking group was lower the rate of falls and more the rate of trips. Obstacle avoidance walking, 6-min walk test, the rate of falls and step count per day improved. |
| Papiol [41]Â 2016 | 126 | â?¥ 74 yrs | Community-dwelling people | Walking habits | â?? | 30 min | â?? | â?? | â?? | Walking habits was associated with decrease of muscle strength, history of falls, walking time per day and ADL. |
| Murata [42] | 59 | â?¥ 65 yrs | Community-dwelling people | Walking | 3 | 30 min | Comfortable speed | 12 wks | ï¼ | 6-min walk distance and objective health feelings improved. Handgrip strength, knee extensor muscle strength, the time of one leg standing position and usual gait speed did not improve. |
| Markofski [43] 2019 | 45 | â?¥ 65 yrs | Community-dwelling people | Treadmill walking | 3 | 45 min | 70% heart rate reserve | 24 wks | Sex | Peak oxygen uptake and 400-m gait speed improved. Knee extensor muscle strength improved in the group of walking exercise plus BCAA only. |
NOTE: ADL: Activities of Daily Living; BBRS: Brunel Balance Rating Scale, BBS: Berg Balance Scale; BMI: Body Mass Index; CS-PEP10: Continuous Scale-Physical Functional Performance Test; FMA-LE: Fugl-Meyer Lower Extremity Assessment; MiniBESTest: Mini-Balance Evaluation Systems Test; Mos: Months; PF: Physical Function; QOL: Quality of Life; RAND-36 QOL: RAND-36 Health Related Quality of Life; SF 12: SF-12 Health Survey; SF 36: MOS 36-Item Short-Form Health Survey; SPPB: Short Physical Performance Battery; TUG: Timed Up-And-Go Test; Wks: Weeks; WOMAC: Western Ontario and McMaster Universities Osteoarthritis Index; Yrs: Years.
Table 1: Studies of the association between walking exercise and physical function in a community-dwelling older people.
Our literature search and inclusion/exclusion criteria resulted in the extraction of 25 papers in English or Japanese that examined the association between walking exercise and physical function in community-dwelling older people. Our review demonstrated that walking exercise contributed to comprehensive physical function, muscle strength, walking speed, balance/fall risk, and exercise capacity.
Regarding the settings of the walking exercise in the extracted studies, most of the settings were outdoors; however, there were also intervention studies in which the walking intensity was increased by brisk walking or adjusted by treadmill walking. The exercise type varied. The most common walking frequency was 3 days/week; the most common time per session was 30 min, and the most frequently used intervention period was 12 weeks. These conditions provide a more-frequent schedule compared to the standard for an exercise habit defined in the National Nutrition Survey in Japan, i.e., 2 days/week and 30 min per session [44]. In the cross-sectional identified in the present review, the relationship between walking and physical function was investigated by setting only the frequency or the time of walking habits. Future studies should examine the precise effects of a walking habit based on set conditions of walking frequency, walking time per session, and intervention period. In addition, because the walking frequency and time parameters of the existing walking intervention studies vary, it is necessary to continue to search for the optimal exercise conditions (including intensity).
There was no association between the frequency of light walking (sampo) or walking in subjects who were robust or in those with pre-frailty [14]. However, we think that it is necessary to further investigate that result by defining the walking time per session and the intervention period, with a larger number of subjects, including those with frailty. Moreover, in robust subjects the exercise time per week tends to be significantly longer, and the frequency of exercise/sports tends to be significantly higher; in other words, it is possible that the influence of exercise and sports other than walking is strong. It is thus necessary to accumulate further evidence about the relationship between walking exercise and both sarcopenia and locomotive syndrome.
Regarding the relationship between walking habit or walking intervention and comprehensive physical function, most of the studies in this review used questionnaires evaluating QOL as a measure of comprehensive physical function. In all of those studies, the subjects with walking habits had higher physical function, and the walking intervention improved physical function. The objective comprehensive evaluation of physical function, i.e., the SPPB, also confirmed that walking exercise was effective for improving physical function. It was reported that the SPPB scores improved in patients with OA and patients with limited physical function. Most studies reported the increment SPPB score instructed the intensity or speed of walking such as a track field walking, on a treadmill walking, the perceived walking (using Borg scale 11–14), and the instructed step-count numbers.
It should thus be noted that these studies’ findings were obtained with set values for the walking intensity.The guidelines of the American Society of Sports Medicine recommend that most individuals’ physical fitness should be improved by exercising at an intensity equivalent to 60%–70% or more of their maximum physical fitness for >30 min per day, >4 days/week for 6 months [45]. The intensity is an important factor for effective exercise. However, the intensity of walking exercise performed by community-dwelling people at their own pace has been predicted to be low, and it is thus necessary to take measures to help community-dwelling people improve the intensity to the optimum level for walking exercise.
We also observed study findings indicating beneficial effects of walking for improving muscle strength in the upper and lower limbs. Only one study showed improvement in upper limb muscle strength, and most of the studies used improvement in lower limb muscle strength as an outcome. The conclusion is inconsistent, because some studies observed that walking exercise was not associated with increased muscle strength in the upper and lower limbs. The walking intervention provided by Minett et al. did not significantly improve the muscle cross-sectional area [30]. It has been speculated that the reason why muscle strength and muscle mass were not related in walking interventions is that walking exercise is not an exercise that uses predominantly fast-fiber muscle [46]. Interval walking is more effective than normal walking for improving muscle strength and muscle mass, suggesting that walking exercise with increased speeds may be useful for preventing sarcopenia [47]. In addition, in the reviewed studies that indicated an association between walking exercise and muscle strength, three studies set the walking frequency, walking time per session and duration, but they did not exclude the effects of confounding factors. The other three studies adjusted their analyses by age, gender, height, weight, and educational history, but the effects of exercise and physical activity other than walking were not considered. In other words, the direct relationship between walking exercise and muscle strength remains unclear.
Among the investigations that used gait speed as an outcome, about half set the intensity of the walking exercise, and the gait speed was improved by having the subjects engage in a walking habit or self-paced walking with a certain frequency, time or period. The positive effect was also observed in patients with stroke, Parkinson disease, knee OA, and low physical fitness. Gait speed is one of the evaluation indices used for frailty syndrome and sarcopenia, because it is suggested that walking exercise is effective for preventing and improving frailty and sarcopenia.
Walking exercise involves the movement of the body’s center of gravity in the standing position, and the walking movement is performed via alternating one-leg standing over the walking cycle, which leads to the improvement of balance ability and is related to the prevention of falls. With a single exception, the studies of walking and balance identified in our review examined outdoor walking exercise, which may include slopes and rough terrain compared to indoor walking and treadmill walking.
This may account for the findings that outdoor walking exercise helped improve balance ability. The remaining study was of stroke patients, whose balance ability was improved by walking on a treadmill with unloading. A walking intervention did not improve the functional reach test results of patients with Parkinson disease, [37] and it thus appears that Parkinson disease is characterized by postural retention disorders that could be improved by both walking exercise and balance exercise.
Regarding the relationship between walking exercise and exercise capacity, walking is a type of aerobic exercise, and continuous moderate-intensity walking led to an improvement of exercise capacity in the studies we reviewed. Among the studies in which an improvement in maximal oxygen uptake was observed, many studies set intensity by the Heart Rate Reserve method. It is thus considered important to walk at the optimum intensity. Additionally, even individuals with OA and those with low physical function have been gain improved exercise capacity by walking in response to subjective fatigue. The exercise capacity affects the feeling of fatigue that is one of the items of the CHS criteria [5]. It was reported that peak oxygen uptake was associated with the usual gait speed in elderly subjects, suggesting that walking exercise may be effective for preventing frailty [48].
Low-intensity endurance exercise, such as walking exercise, activates Sirtuin 1, a histone deacetylase that is important for preventing cell death and maintaining muscle function [49,50]. Therefore, walking exercise is important for older people at the cellular and tissue levels. Walking exercise helps prevent the onset of various diseases, and it was reported that among older people, those who reported walking for >1 hr each day had a significantly lower 2-year mortality rate than those who walked <1 hr [10-13]. Hospitalization due to illness or injury may cause environmental changes and decreased activity, resulting in secondary physical and cognitive declines and deconditioning. A systematic review reported that a hospitalization-related decline of physical and cognitive function was present in >30% of elderly inpatients [51]. Therefore, regarding the cross-sectional study in the present review that showed a relationship between walking habits and physical function, the management of diseases and the prevention of hospitalization are also factors.
Challenges for the future
There are no reports of a direct association between walking exercise and frailty, sarcopenia, or locomotive syndrome. However, walking exercise has the effect of improving muscle strength, flexibility, balance, walking speed, and exercise capacity and leads to the improvement of comprehensive physical function. Walking exercise would thus also be an important exercise for individuals who have or are at risk of developing frailty and sarcopenia.
It remains necessary to examine frailty syndrome, sarcopenia, and locomotive syndrome as outcomes of walking interventions, clarify the relationship between these disorders and walking exercise, and confirm the precise effects of walking interventions.
We found no study that considered the effect of the subjects’ physical activity aside from the walking intervention. We suspect that a direct relationship between walking exercise and frailty will be revealed by considering the effect of high physical activity other than walking. In addition, the types of intervention and the walking frequencies, time, duration, and intensity differed among the reviewed studies, and it remains necessary to identify the optimal parameters of walking exercise for various populations. It is also necessary to conduct environmental research that allows community-dwelling individuals to take the initiative in continuing walking exercise.
A walking habit and walking exercise contribute to the maintenance and improvement of physical function in older community-dwelling people.
This study was supported in part by Grants-in-Aid for Scientific Research (B) (20H04016) from the Ministry of Education, Culture, Sports, Science and Technology of Japan.
Tsubasa Yokote reports no disclosures related to this work.
Hiro Kishimoto, PhD reports no disclosures related to this work.
The authors thank the students, researchers and staff of laboratory for their cooperation in this review.
Citation: Yokote T, Kishimoto H (2021) Association between Walking Exercise and Physical Function: In Community-Dwelling Older People. Int J Phys Med Rehabil. S7:005.
Received: 02-Jun-2021 Accepted: 16-Jun-2021 Published: 23-Jun-2021 , DOI: 10.35248/2329-9096.21.s7.005
Copyright: © 2021 Yokote T, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.