Clinical Pediatrics: Open Access
Open Access
ISSN: 2572-0775
ISSN: 2572-0775
Image Article - (2024)Volume 9, Issue 4
The authors present a male child of 5 years-old with an autism spectrum disorder, who had several episodes of lameness and refusal to walk. Communication restrictions limited the interpretation and valuation of complaints. Through imaging exams, the diagnosis of Meyer's dysplasia was suggested, but the clinical case did not evolve to the complete resolution. This report intends to make aware of Meyer's dysplasia, a rare and little-known condition with a benign course. Knowledge of this clinical entity and its proper identification can decrease unnecessary treatments. However, clinical and radiological evolution is essential for its diagnosis [1]. A 5-year-old male born by c-section with birth weight 4085 g had a self-limited episode of right lameness and refusal to walk at 13 months. He had a new episode at 22 months, with no fever or previous infectious circumstances. Hip ultrasound showed fragmentation of the right femoral calcification nucleus, which was reinforced on radiography (Figure 1). On suspicion of avascular necrosis, the patient underwent nuclear magnetic resonance imaging, confirming fragmentation and flattening of the right femoral ossification nucleus, without loss of sphericity or congruence (Figure 2) [2].
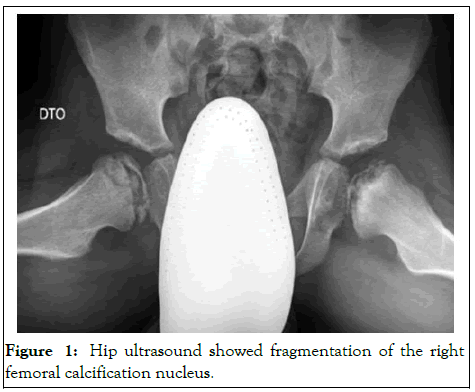
Figure 1: Hip ultrasound showed fragmentation of the right femoral calcification nucleus.
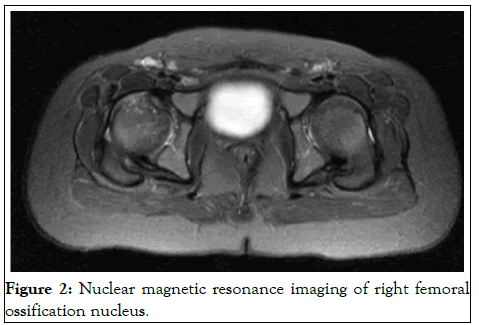
Figure 2: Nuclear magnetic resonance imaging of right femoral ossification nucleus.
Meyer's dysplasia diagnosis was done. However, the boy had experienced recurrent episodes of pain, difficult to value because of the disturbance of the autism spectrum that the child presents and had developed bilateral pathological changes with progressive flattening on the left side. Meyer Dysplasia (MD) or femoral epiphyseal dysplasia, is a modification of hip development, characterized by late and irregular ossification of the femoral epiphyseal nucleus. Usually, the normal process occurs between 4 and 11 months. It was described by Pedersen and Meyer, begins in the second year of life and usually resolves until six-years-old. It is more frequent in males, usually bilateral involvement, and has an incidence of 4.4%-10%.
The etiology of this condition is not clear and it may be asymptomatic, but pain, lameness or limitation of hip rotation and abduction may appear. The diagnosis is often a radiological finding.
It can be identified by little, fractured ossification nucleus or cystic changes of the epiphysis, but without fragmentation, reduction, subchondral fractures, subluxation or collapse of the femoral head. The nucleus has multiple ossification centers, which gradually increase and coalesce, maintaining the sphericity of the femoral head. These changes can be described as perthes disease, which has a different treatment and prognosis. Hypothyroidism, multiple epiphyseal dysplasia, spondylopiseal dysplasia and arthritis are differential diagnoses to consider. Progressive improvement of radiological imaging over three to four years is characteristic, there is no need for a specific treatment and the resolution leaves no sequelae [3].
Learning points
• Meyer's dysplasia is a rare and little-acknowledged condition
with a favorable progression.
• Awareness of this entity and its accurate identification can
decrease additional treatments.
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[crossref] [Google Scholar] [PubMed]
Citation: Lachado A, Martins R, Vieira C (2024) Atypical Avascular Necrosis in Children. Clin Pediatr. 09:272.
Received: 06-Jan-2020, Manuscript No. CPOA-24-3067; Editor assigned: 09-Jan-2020, Pre QC No. CPOA-24-3067 (PQ); Reviewed: 23-Jan-2020, QC No. CPOA-24-3067; Revised: 22-May-2024, Manuscript No. CPOA-24-3067 (R); Published: 19-Jul-2024 , DOI: 10.35248/2572-0775.24.09.272
Copyright: © 2024 Lachado A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.