International Journal of Physical Medicine & Rehabilitation
Open Access
ISSN: 2329-9096
ISSN: 2329-9096
Mini Review - (2022)
Avascular Necrosis of the Femoral Head (AVNFH) can have known causes, but many cases are idiopathic and are diagnostically challenging. Because early intervention vastly improves outcomes in AVNFH, it is important that we develop better means for identifying these cases. Here we present a case of an incidental finding of idiopathic AVNFH in a young woman and the methods used to preserve the femoral head and prevent or delay the need for total hip arthroplasty. We highlight key research findings to contextualize the case and the urgent need for early identification of idiopathic cases and better treatment options for young patients.
Avascular necrosis; Femoral head; Hip arthroplasty; Core decompression
A young female was diagnosed with idiopathic AVNFH with no relevant symptoms
A 31-year-old Caucasian female presented to the emergency room with intractable vomiting that she had been enduring for approximately 10 hours. A Computed Tomography (CT) scan of her abdomen revealed bilateral AVNFH. At the time of diagnosis, she had no hip pain, though pain developed shortly after diagnosis. The patient had no known risk factors for any form of AVNFH.
To save the femoral heads, core decompression was conducted. The patient subsequently underwent an outpatient rehabilitation program. Her bilateral hip pain significantly improved following the surgery. However, it is not clear how long necrotic processes were taking place before her condition was identified and addressed, and whether the femoral heads will eventually collapse and require full hip joint replacement. Photos of the femoral heads before, during and after core decompression are provided in Supplementary Figures 1-11.
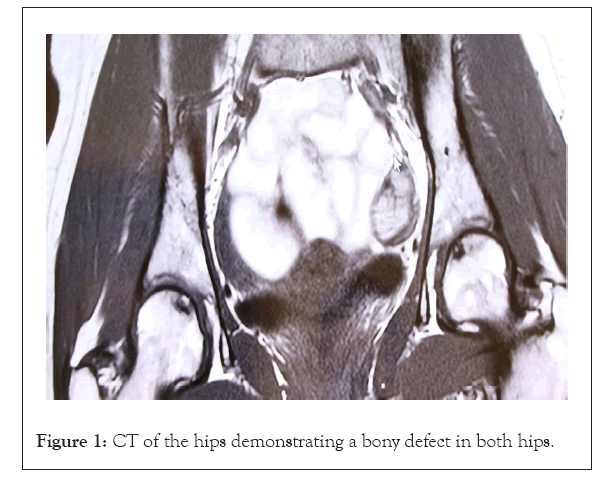
Figure 1: CT of the hips demonstrating a bony defect in both hips.
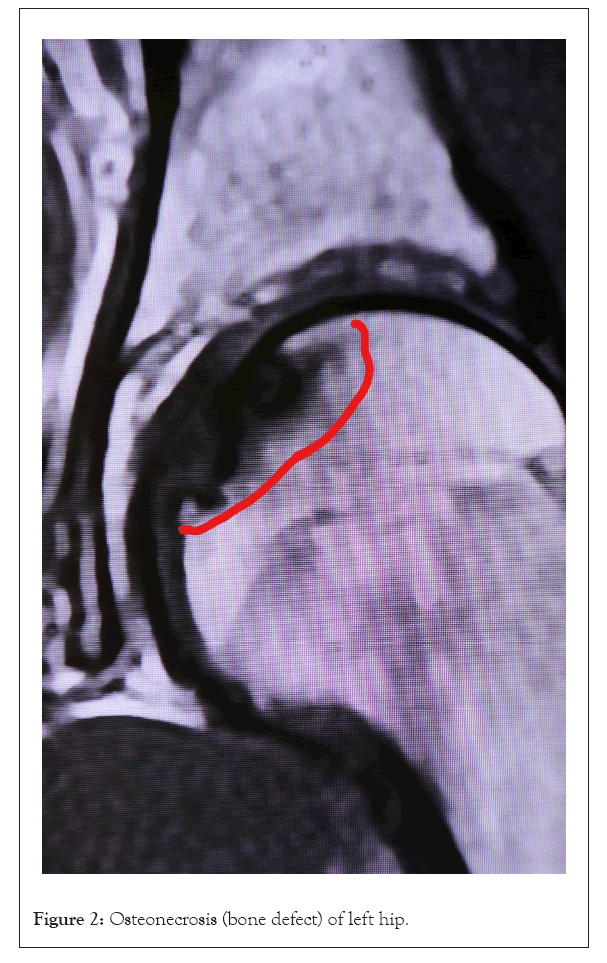
Figure 2: Osteonecrosis (bone defect) of left hip.
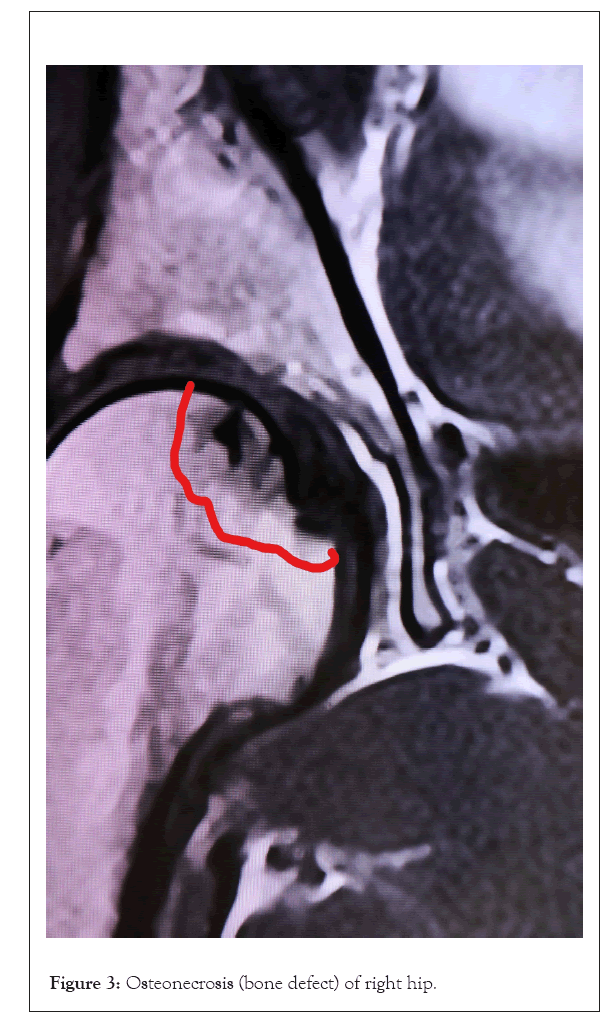
Figure 3: Osteonecrosis (bone defect) of right hip.
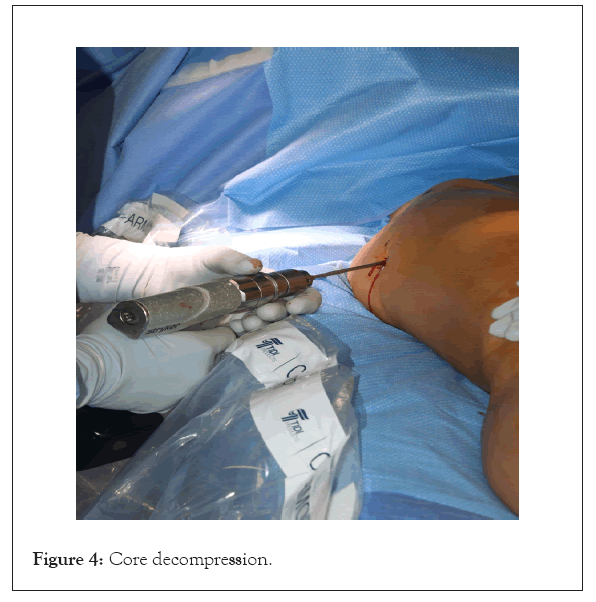
Figure 4: Core decompression.
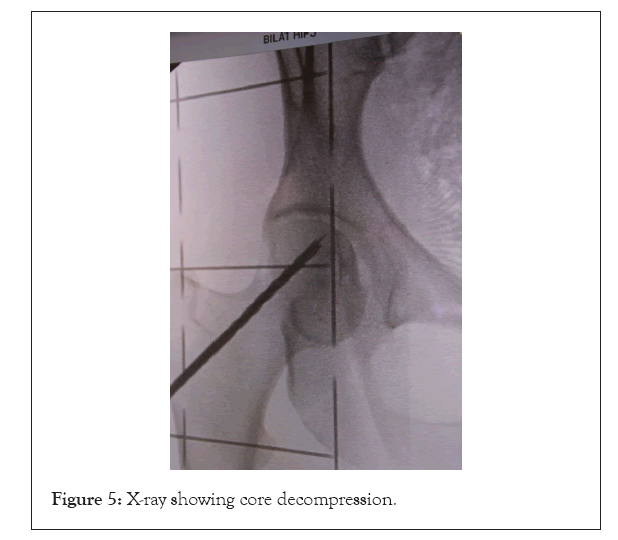
Figure 5: X-ray showing core decompression.
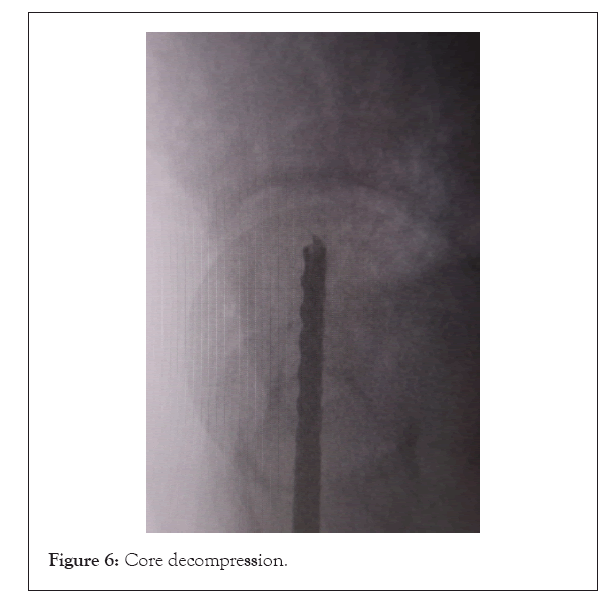
Figure 6: Core decompression.
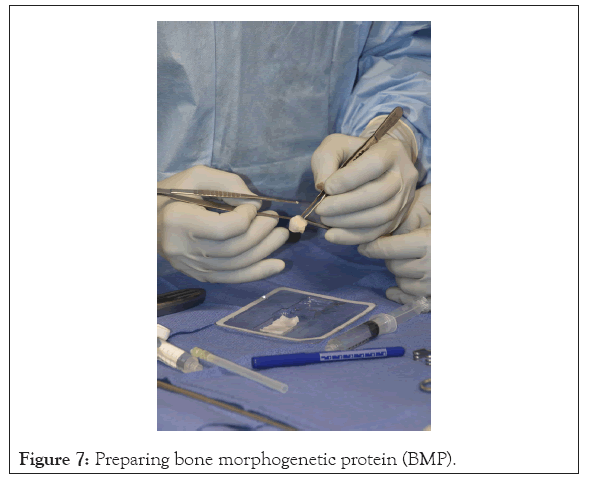
Figure 7: Preparing bone morphogenetic protein (BMP).
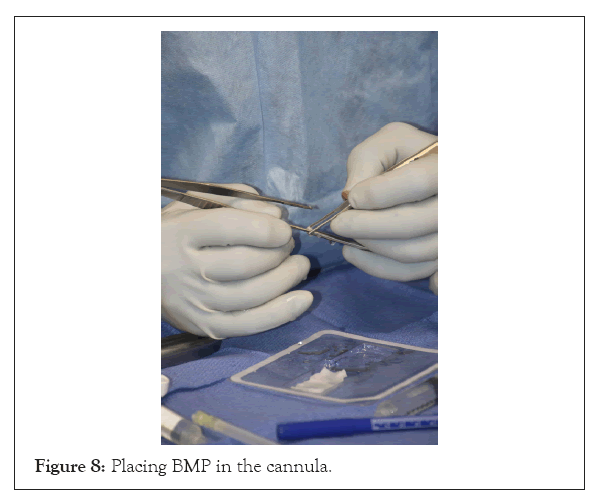
Figure 8: Placing BMP in the cannula.
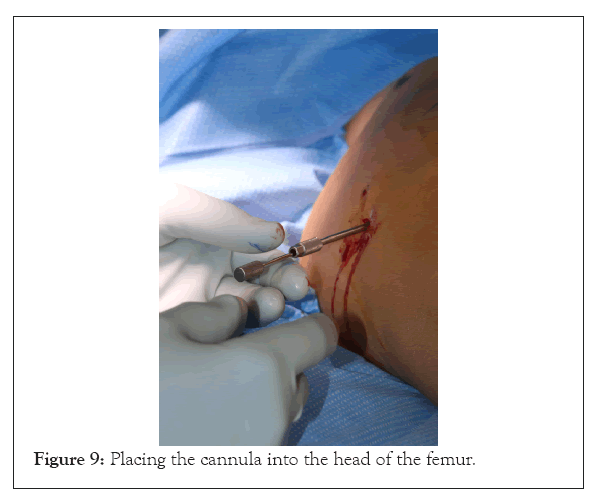
Figure 9: Placing the cannula into the head of the femur.
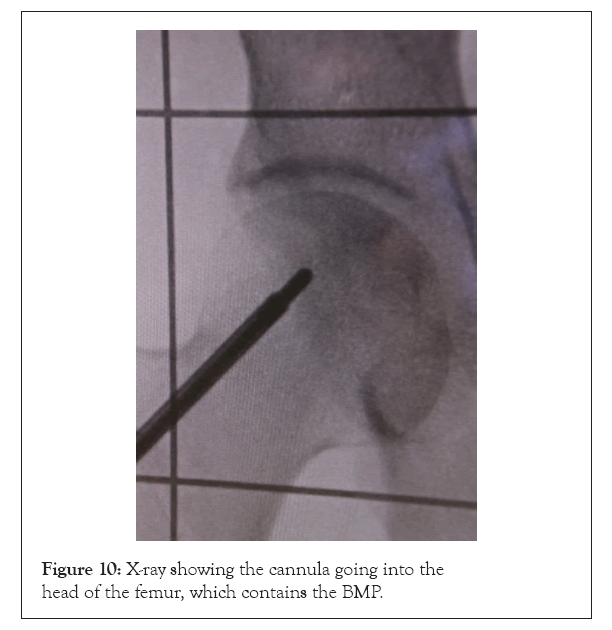
Figure 10: X-ray showing the cannula going into the head of the femur, which contains the BMP.
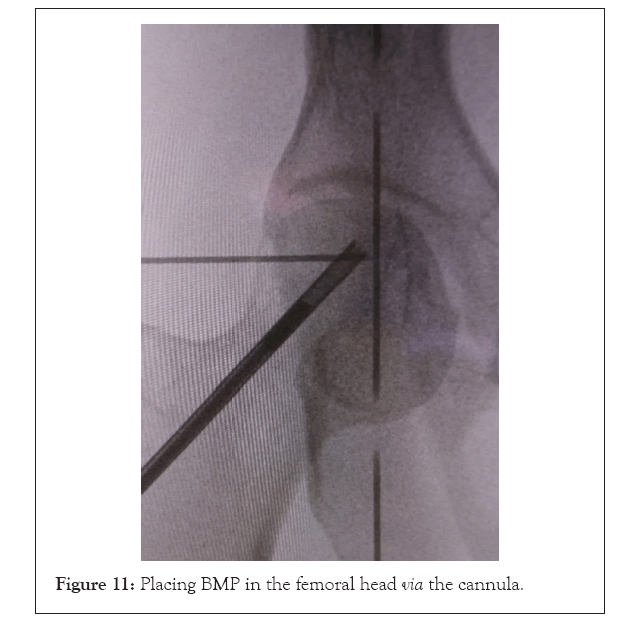
Figure 11: Placing BMP in the femoral head via the cannula.
While the specific protection afforded by core decompression in this case is not yet known, the literature on AVNFH suggests that early core decompression may be the best route for preventing femoral head collapse and the need for total hip arthroplasty. Nonetheless, this gap in our understanding of the causes of idiopathic AVNFH and the long-term influence of interventions must be addressed. Through concerted research efforts so that we can provide AVNFH patients with the most appropriate care that increases the chances of the best health outcomes.
AVNFH results from disruption of blood supply to the femoral head
AVNFH occurs largely because of blood perfusion impairment and enhancement of intraosseous pressure [1]. The femoral head normally receives blood through a branch of the obturator artery [9]. Vascularity of the femoral head depends on retinacular vessels, particularly the lateral epiphyseal artery, which supplies 70% to 80% of the vascular supply to the femoral head [10]. When the vascular supply to the femoral head is compromised, ischemia occurs, leading to necrosis.
The reason for necrosis, as well as the course of progression to end stage AVNFH varies across patients. While fractures cause vascular lesions that prime the femoral head for necrosis, fractures are not required for AVNFH to occur. Progression appears to rely primarily on five mechanisms [3]. These mechanisms include hypercoagulable conditions, suppression of angiogenesis, hyperadipogenesis, switching from bone remodeling to bone resorption, and genetic factors.
Blood supply to the femoral head can be compromised for known or unknown reasons
There are several risk factors that increase the likelihood of developing AVNFH, the knowledge of which can lead to earlier diagnosis and more effective follow-up and intervention [11]. Traumatic, atraumatic, and idiopathic cases of AVNFH are common.
Trauma: Trauma can lead to AVNFH. The most common injury associated with AVNFH is femoral neck fracture, though other injuries such as anterior hip dislocation can also result in AVNFH. In cases where the femoral neck has been fractured, femoral head collapse and arthritis are considered inevitable, with total hip replacement eventually being needed [12,13]. Up to 18% of the 250,000 patients who undergo hip arthroplasty in the U.S. each year due to osteoarthritis have developed their arthritis due to AVNFH [9,14,15].
Exposures: Steroids and alcohol increase the risk for AVNFH in a dose-dependent way [13]. However, even a single intra-articular injection of steroids has led to avascular necrosis [14,16,17]. Alcohol contributes to AVNFH by disrupting the metabolism of phospholipids and cytokines.
Hematologic disorders: Sickle cell disease is arguably the most recognized condition that is often observed in AVNFH. Research has shown that half of those who have suffered from sickle cell disease for 35 years develop bone necrosis [13]. When avascular necrosis occurs in this group, the femoral head is the most likely site to be involved [18].
Research on sickle cell disease patients has revealed that hemoglobin levels are elevated in the femoral head when AVNFH occurs. These findings suggest that high blood viscosity and hypoxia may contribute to the condition [11]. Other hematologic disorders like hemophilia, thalassemia, and polycythemia are also associated with AVNFH [19].
Other conditions: Other conditions associated with AVNFH include lupus erythematous, Caisson disease, Cushing’s disease, HIV, cancer, chronic renal failure, pancreatitis hypercholesterolemia, hyperparathyroidism, and pregnancy [19-22]. AVNFH is a rare complication observed in Hodgkin’s disease and has also been identified in the context of scleroderma [23,24].
Genetics: The observation that AVNFH sometimes occurs in twins as well as in familial clusters also suggests that genetic factors may contribute to the disorder [19] The progression to end-stage AVNFH may depend on the expression of genes that encode proteins involved in coagulation pathways, ischemia, angiogenesis, apoptosis, thrombus formation, lipid biosynthesis, and bone remodeling and help to explain differences in the timing and nature of progression of the disorder [13].
Treatment goals differ depending on the disease stage and patient age
According to the literature, total hip arthroplasty is the most effective treatment for AVNFH [1]. The studies on total hip arthroplasty in AVNFH demonstrate excellent long-term results, with revision rates of about 3%-comparable to what is observed in those with osteoarthritis [25]. While this intervention is appropriate and beneficial for elderly patients whose AVNFH likely resulted from trauma related to falls, it is not ideal for younger patients.
In the younger patient population, rather than replacing the joint, preserving the native joint and delaying the need for hip replacement is the critical goal of therapy [21]. Unfortunately, there is no consensus on what this optimal treatment is, largely owing to variability in reported success rates and a lack of randomized trials [20,21,25]. AVNFH is bilateral in 30% to 70% of patients, further compromising functioning and complicating recovery [4,21].
Nonsurgical treatment options for early pre-collapse stages of AVNFH have tended to be unsuccessful for managing the condition [2,20,26]. These interventions include pharmacotherapy (e.g. nonsteroidal anti-inflammatory drugs, bisphosphonates) and physiotherapy interventions such as weight bearing and electrostimulation. Surgical options to preserve the joint include core decompression, osteotomy, bone marrow grafting, and non-vascularized bone grafting techniques [25]. These surgical interventions have been shown to be more promising in preventing femoral head collapse and alleviating AVNFH symptoms over the long-term than nonsurgical options.
Core decompression is the first-line therapy for early stages of AVNFH
Despite no gold standard for treating AVNFH in younger patients, research suggests that core decompression, a minimally invasive surgical procedure, may currently be the most effective way to deal with AVNFH when the goal is to preserve the native joint [27]. Core decompression is therefore recommended as a first-line therapy for early AVNFH [4].
A recent meta-analysis on core decompression found that the treatment was both safe and effective [15,20]. Use of core decompression in the early stages of AVNFH has been demonstrated to reduce morbidity, but it has also been shown to provide significant long-term analgesic effects across all stages [4].
Core decompression works by reducing intraosseous pressure and restoring circulation in the femoral head [20]. By drilling holes into the femoral head, internal pressure is relieved, and space is created for new blood vessels. The technique has been shown to significantly reduce pain in AVNFH patients, regardless of age and sex [28,29]. Not only has core decompression been shown to delay progression in 80% of AVNFH cases, but unlike other surgical procedures aimed at preservation, it does not compromise procedures that may subsequently become necessary [27].
Early intervention is key for avoiding femoral head collapse and hip joint replacement
It is critically important to diagnose AVNFH at early stages when core decompression surgery can slow disease progression and prevent or delay total hip arthroplasty, a major surgery that can lead to health complications [4]. However, while imaging techniques are invaluable for AVNFH diagnosis and preoperative planning, they are often not deployed early enough to prevent progression because AVNFH tends to be asymptomatic until it progresses to the point that damage has occurred [9,12,30].
Often joint destruction is well underway before AVNFH is diagnosed [22]. By then, it is difficult or impossible to determine when ischemia began and to assess prognosis in cases where total hip arthroplasty is not immediately pursued [13]. Because idiopathic cases and cases occurring in young patients - which overlap significantly-require early intervention for optimal outcomes, there is a significant need for more reliable ways to identify AVNFH early.
In our case described above, had the young patient not suffered an illness that required imaging analysis that led to her incidental diagnosis, intervention would have been delayed and her prognosis likely much poorer. Had her AVNFH progressed to the point of femoral head collapse, she may have required a total hip arthroplasty at the age of 31, and thus likely required several major surgeries over the course of her lifetime [7,8].
Total hip arthroplasty is an effective therapeutic strategy for AVNFH in elderly patients. However, to avoid femoral head collapse and the need for total hip arthroplasty in younger patients, preservative techniques are recommended. Core decompression has been shown to be safe and effective for alleviating pain at all stages of AVNFH and for avoiding or delaying the need for total hip arthroplasty when performed in early stages.
While it is critically important that clinicians consider AVNFH as a differential diagnosis when relevant risk factors are present, idiopathic cases often occur with no known risk factors. In these cases, clinicians and patients are blind to the possibility of AVNFH, which points to the need for a better understanding of the causes and mechanistic drivers of the disease so that AVNFH can be more readily identified.
Fortunately, mechanisms underlying AVNFH are being elucidated through the research and contributing to our understanding of how best to treat the condition. For instance, data are beginning to show how the development of biomarkers could help to extend the treatment window and potentially reduce the frequency with which surgery is required. As more of this research is conducted and translated into clinically meaningful insights, we will become more equipped to identify AVNFH in cases like the idiopathic case described herein. Long-term data are needed to improve our understanding of the impact of specific interventions in idiopathic cases of AVNFH. As such, a follow-up paper will be published to clarify the clinical course and outcomes in the case described herein and to provide more detailed information on AVNFH prognosis as well as the appropriate classifications and corresponding treatments.
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] (All versions) [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
Citation: Lichtblau CH, Warburton C, Meli G, Gorman A (2022) Avascular Necrosis of the Femoral Head: The Challenge of Early Identification and Intervention in Idiopathic Cases. Int J Phys Med Rehabil. S20:001.
Received: 17-Oct-2022, Manuscript No. JPMR-22-19668; Editor assigned: 21-Oct-2022, Pre QC No. JPMR-22-19668 (PQ); Reviewed: 10-Nov-2022, QC No. JPMR-22-19668; Revised: 17-Nov-2022, Manuscript No. JPMR-22-19668 (R); Published: 28-Nov-2022 , DOI: 10.35248/2329-9096.22.S20.001
Copyright: © 2022 Lichtblau CH, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.