Emergency Medicine: Open Access
Open Access
ISSN: 2165-7548
ISSN: 2165-7548
Research Article - (2022)Volume 12, Issue 7
Background: Despite the importance of Evidence Based Medicine (EBM) in improving the quality of healthcare, many barriers hamper its successful implementation. Evidence on these barriers could facilitate interventions and health policy directions aimed at optimizing best clinical practices. This study aimed to identify the barriers to EBM implementation in Ethiopia through a systematic Study of the literature.
Methods: PubMed, EBSCO, Google Scholar, and Semantic Scholar were searched for relevant articles. Peer-Reviewed primary studies were eligible for inclusion if they assessed barriers to EBM in Ethiopia. The Qualsyst tool was used to assess the quality of included studies. The barriers identified in the included studies were analyzed based on their frequency of occurrence among the studies.
Results: This systematic Study summarized the results of 11 empirical studies and identified 20 barriers to EBM in Ethiopia. The most common barriers reported in these studies were a lack of EBM knowledge, inadequate resources, inadequate time, lack of EBM training, difficulty in interpreting research findings, lack of management support, overloading of patients, and negative attitudes towards EBM.
Conclusion: This Study identified a variety of potential barriers to EBM implementation in Ethiopia. Providing short-term EBM training or incorporating EBM into the medical curriculum, time-management workshops, resource provision, and adequate support are needed to facilitate EBM implementation in Ethiopia. Further studies should build on this evidence and focus on developing a context-specific EBM implementation framework.
Evidence-based medicine; Implementation; Barriers; Interventions
EBM: Evidence Based Medicine.
Evidence Based Medicine (EBM) is the integration of clinical expertise with the best available evidence from scientific studies and individual patient opinions, concerns, and expectations [1]. EBM implementation involves five stages: creating clinical questions that can be answered, searching and obtaining evidence, critically appraising the evidence, applying evidence, and evaluating performance. EBM is considered one of the most important milestones in modern medicine [2-4].It provides well-recognized support for high-quality, personalized, cost-effective care for patients [5,6]. Worldwide, EBM principles are used to develop and apply clinical practice guidelines that help clinicians make the right decisions for their patient's health issues. In addition, improved outcomes were observed in patients receiving evidence-based medical care [7]. EBM is important in developing countries for its cost-effectiveness and efficient use of healthcare resources [8].
Despite great advances in knowledge production for EBM, healthcare organizations continue to face significant implementation failures or challenges [9]. In developing countries, where resource scarcity and disease burden are high, health care practice should be based on high-quality, up-to-date research findings [10]. However, despite the growing body of research that considers the best evidence available to inform clinical decision-making, the uptake of research findings into clinical practice remains poor [11-13]. Researchers have found several barriers to EBM implementation in low-resource settings. Major barriers include time constraints, lack of knowledge, lack of resources, negative attitude towards EBM, lack of training, and financial constraints [14-16].
To enhance EBM implementation at all levels of the health system, Ethiopia arranged a workshop on evidence-based healthcare for different health professionals [17]. Despite the effort underway, many Ethiopian healthcare professionals continue to provide health care as previously provided without the inclusion of EBM in their clinical practice [18,19]. Ethiopia has some unique features that add an extra layer of complexity to EBM implementation, such as a small culture of using evidence in health systems at all levels and an extreme shortage of health care providers who specialize in synthesizing evidence for policy design [20]. In countries facing these conditions, the need to implement effective and efficient health care strategies is even more important. A locally designed implementation plan that takes into account context-specific barriers and strategies is essential [21].
The first step in overcoming EBM implementation failures is to assess and identify barriers. Insight on barriers facilitates interventions and provides health policy directions aimed at optimizing best practices. Furthermore, evidence on these barriers is important in an attempt to close the prevailing knowledge-to-practice gap [22]. Researchers also note that knowledge of barriers to EBM improves compliance with EBM programs [23]. Some studies have been conducted in various parts of Ethiopia to understand the barriers of EBM. However, there is not a single comprehensive study that combines the results of these studies and provides a clear view of the barriers. Thus, this study aimed to identify barriers to EBM implementation in Ethiopia through a systematic literature Study. This study will contribute to the breadth of literature on EBM, which is essential to designing effective interventions for the successful implementation of EBM.
A systematic literature Study was conducted according to the Preferred Reporting Items for Systematic Studies and Meta-Analyses (PRISMA) [24]. Following these guidelines, we developed a search strategy and eligibility criteria before conducting a Study. After that, searches were conducted and retrieved articles were assessed in a two-step screening process based on pre-defined eligibility criteria. After identifying the studies that qualify for this Study, relevant data were collected from each study. Details of the Study procedure are given below.
Information sources and search strategy
PubMed, EBSCO, Google Scholar, and Semantic Scholar were searched to find relevant articles. To increase the chances of identifying all research conducted in Ethiopia, two common search terms, separated by operator "OR", were used: "evidence-based medicine" and "Ethiopia" or "evidence-based practice" and "Ethiopia".
Eligibility criteria
The following selection criteria were used to identify articles for eligibility: 1) articles published in peer-Reviewed journals, but unpublished work was excluded, 2) articles assessing barriers to EBM/EBP, but not other aspects of EBM/EBP, 3) articles based on empirical studies, and 4) articles where the country of data collection in Ethiopia.
Screening and selection
After searching, the identified articles were screened in two stages. The first stage involves screening the titles and abstracts based on the eligibility criteria, followed by a Study of the full text of the articles with similar criteria. Initially, two independent Studies examined all titles and abstracts for eligible articles. Articles that fail to meet inclusion criteria are removed from the list. Differences regarding exclusions between the two Studiers were resolved through discussion. Finally, all Studiers individually evaluated the full text of each article and made a final selection of important studies for inclusion.
Quality assessment
Methodological quality assessment of studies was conducted using standard quality assessment criteria for evaluation of primary research papers (Qualsyst tool) [25]. Different questions were posed for qualitative and quantitative studies and in the case of mixed-method studies, both questionnaires were used. The tool has a checklist of 14 question items for assessing quantitative and 10 questions for qualitative studies and each item is assigned a score of 0 (not addressed), 1 (partially addressed), and 2 (fully addressed). The overall quality score was calculated by adding the total score in all the items and dividing them by the possible maximum score. Papers were included if they scored at least 50% of the total possible points, providing a relatively generous cut-off point in the standard quality assessment criteria for evaluating basic research papers.
Data extraction and analysis
Studies that met the inclusion criteria were further analyzed and the following items were extracted from each study: research method (quantitative, qualitative, and mixed), data collection methods (interview, questionnaire), number of participants, and sampling methods. Finally, the empirical results about barriers to EBM were extracted from each study. Meta-analysis of results was not possible due to differences between studies in terms of research methods and sample types. However, the analytical method used by previous systematic Studies [26,27] was used in this study. In this approach, the barriers were analyzed according to the frequency of occurrence in the literature. This approach can produce reliable results in our case, as it can give a clear picture of what barriers were identified empirically, by how many studies, and how frequent are these barriers among the results.
Study selection
The selection process and the associated inclusion criteria are presented in Figure 1. A total of 3,164 articles were identified for preliminary screening. Then, 1,710 articles were removed after being identified as duplicates. After the duplicates were removed, the titles and abstracts of 1,454 articles were screened for eligibility. Leaving 1370 articles based on title and abstract screening, 84-articles were presented for full-text screening. A total of 73 studies were excluded after the full-text screening. Accordingly, 11 articles were included in the Study.
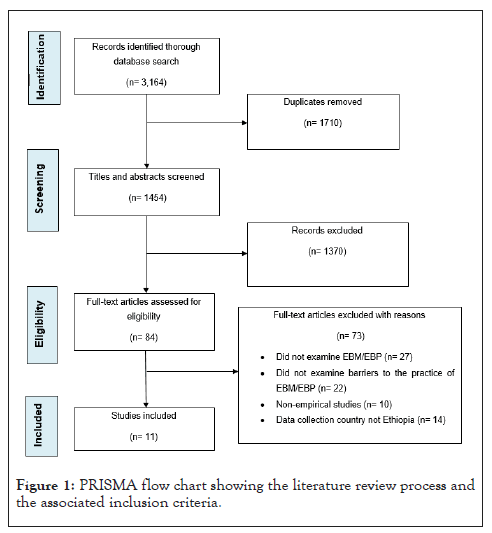
Figure 1: PRISMA flow chart showing the literature review process and the associated inclusion criteria.
Characteristics of included studies
Table 1 provides the characteristics of included studies. Out of the 11 articles included in the Study, nine studies used a quantitative research method and three studies used a mixed approach. All of the identified studies were conducted in the hospital setting. Different types of participants were involved in the data collection process in the included studies. Six studies involved a single sample type such as physicians and nurses [28-32]. The remaining studies involved a mix of different health professionals such as nurses and midwives, physicians, and nurses [33-37].
| Reference/Year of publication | Type of research | Data collection method | Number of participants/ Sampling technique |
|---|---|---|---|
| [28]/ 2019 |
Quantitative | Questionnaire | 137/ Stratified random sampling |
| [34]/ 2020 |
Quantitative | Questionnaire | 415/ Stratified sampling |
| [35]/ 2017 |
Quantitative | Questionnaire | 438/ Stratified random sampling |
| [29]/ 2015 |
Mixed | Questionnaire and in-depth interview | 406/ Random sampling |
| [30]/ 2021 |
Quantitative | Questionnaire | 684/ Random sampling |
| [33]/ 2021 |
Quantitative | Questionnaire | 826/ Random sampling |
| [32]/ 2018 |
Quantitative | Questionnaire | 333/ Random sampling |
| [37]/ 2016 |
Quantitative | Questioner | 144/ Sampling method not provided |
| [31]/ 2018 |
Quantitative | Questionnaire | 223/ Sampling method not provided |
| [18]/ 2019 |
Mixed | Questionnaire | 270/ Stratified random sampling |
| and in-depth interview | |||
| [36]/ 2015 |
Quantitative | Questionnaire | 403/ Stratified random sampling |
Table 1: Characteristics of the included studies.
Barriers to the implementation of EBM in Ethiopia
The analysis identified 20 barriers spread across the 11 studies, as shown in Table 2. The 20 barriers are organized by the frequency of occurrences among the studies, with the most frequently listed first. Lack of EBM knowledge and insufficient resources each appeared in seven of the eleven studies (63.6%). Lack of time to practice EBM appeared in five of the eleven studies (45.5%). Lack of EBM training appeared in four of the eleven studies (36.4%). Difficulty in interpreting research findings, lack of management support, patient overload, and negative attitude towards EBM, each appeared in three of the eleven studies (27.3%). Lack of skill to search for evidence and poor access to research evidence each appeared in two of the eleven studies (18.2%). Ten barriers: Inability to retrieve evidence, inability to evaluate the outcome of EBM practice, lack of research experience, lack of EBM guidelines, lack of self-efficacy to practice EBM, lack of information sources, lack of investment by health authorities, lack of financial gain in practicing EBM, inability to understand statistical terms used in research articles, and lack of autonomy to change practice each appeared once in the eleven studies (9.1%).
| No. | Barriers | References | Frequency | % |
|---|---|---|---|---|
| 1 | Lack of EBM knowledge | [28-31], [32, 33], [36] | 7 | 63.6 |
| 2 | Insufficient resources | [28], [18, 30, 31], [34, 35], [37] | 7 | 63.6 |
| 3 | Lack of time to practice EBM | [28-30], [18], [35] | 5 | 45.5 |
| 4 | Lack of EBM training | [30], [34-36] | 4 | 36.4 |
| 5 | Difficulty in interpreting research findings | [28], [30], [18] | 3 | 27.3 |
| 6 | Lack of management support | [29, 30], [34] | 3 | 27.3 |
| 7 | Patient overload | [29, 30], [37] | 3 | 27.3 |
| 8 | Negative attitude towards EBM | [30], [33], [36] | 3 | 27.3 |
| 9 | Lack of adequate search skill | [29, 30] | 2 | 18.2 |
| 10 | Poor access to research evidence | [18], [37] | 2 | 18.2 |
| 11 | Inability to retrieve evidence | [28] | 1 | 9.1 |
| 12 | Inability to evaluate the outcome of practicing EBM | [28] | 1 | 9.1 |
| 13 | Lack of research experience | [30] | 1 | 9.1 |
| 14 | Lack of EBM guidelines | [30] | 1 | 9.1 |
| 15 | Lack of self-efficacy to practice EBM | [33] | 1 | 9.1 |
| 16 | Lack of information sources | [32] | 1 | 9.1 |
| 17 | Lack of investment by health authorities | [37] | 1 | 9.1 |
| 18 | Lack of financial gain in practicing EBM | [37] | 1 | 9.1 |
| 19 | Inability to understand statistical terms used in research articles | [31] | 1 | 9.1 |
| 20 | Lack of autonomy to change practice | [18] | 1 | 9.1 |
Table 2: Barriers to the implementation of EBM in Ethiopia.
Quality of included studies
The mean quality score of all included studies was 72%, with a range of 67% to 95%. The mean quality score of quantitative studies was 73% (range from 70% to 95%) and the mean quality score of mixed method studies was 70% (range from 67% to 74%). Tables 3 and 4 shows the overview of the score of the articles for quantitative and mixed method studies respectively.
| Criteria | [28] | [34] | [35] | [30] | [33] | [32] | [37] | [31] | [36] |
|---|---|---|---|---|---|---|---|---|---|
| Question/objective sufficiently described | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 |
| Study design evident and appropriate | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 |
| Method of subject/comparison group selection or source of information/input variables described and appropriate | 1 | 2 | 1 | 2 | 1 | 1 | 2 | 2 | 1 |
| Subject (and comparison group, if applicable) characteristics | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 |
| sufficiently described | |||||||||
| If the interventional and random allocation was possible, | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| was it described | |||||||||
| If interventional and blinding of investigators was possible, | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| was it reported | |||||||||
| If interventional and blinding of subjects as possible, | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| was it reported | |||||||||
| Outcome and (if applicable) exposure measure(s)well defined | 2 | 1 | 1 | 2 | 2 | 1 | 1 | 1 | 1 |
| and robust to measurement/misclassification bias? Means of assessment reported? | |||||||||
| Sample size appropriate | 2 | 2 | 2 | 2 | 2 | 2 | 1 | 2 | 1 |
| Analytic methods described/justified and appropriate? | 1 | 2 | 2 | 2 | 2 | 1 | 1 | 1 | 2 |
| Some estimate of variance is reported for the main results | 1 | 0 | 1 | 1 | 2 | 1 | 0 | 1 | 1 |
| Controlled for confounding | 2 | 1 | 1 | 1 | 1 | 1 | N/A | 2 | 2 |
| Results reported in sufficient detail | 2 | 2 | 2 | 2 | 2 | 1 | 1 | 2 | 2 |
| Conclusions supported by the results | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 1 | 1 |
| Overall quality score=total score/possible maximum score | 19/22 | 18/22 | 18/22 | 20/22 | 21/22 | 16/22 | 14/20 | 18/22 | 17/22 |
| 0.86 | 0.82 | 0.82 | 0.91 | 0.95 | 0.73 | 0.7 | 0.82 | 0.77 |
Table 3: Quality assessment results of quantitative studies.
| Quantitative criteria | [29] | [18] |
|---|---|---|
| Question/objective sufficiently described | 2 | 2 |
| Study design evident and appropriate | 2 | 2 |
| Method of subject/comparison group selection or source of information/input variables described and appropriate | 2 | 1 |
| Subject (and comparison group, if applicable) characteristics sufficiently described | 1 | 2 |
| If the interventional and random allocation was possible, was it described | N/A | N/A |
| If interventional and blinding of investigators was possible, was it reported | N/A | N/A |
| If interventional and blinding of subjects wasssification possible, was it reported | N/A | N/A |
| Outcome and (if applicable) exposure measure(s) well defined | 1 | 1 |
| and robust to measurement/muscle bias? Means of assessment reported? | ||
| Sample size appropriate | 2 | 2 |
| Analytic methods described/justified and appropriate? | 2 | 2 |
| Some estimate of variance is reported for the main results | 1 | 0 |
| Controlled for confounding | 2 | 2 |
| Results reported in sufficient detail | 2 | 2 |
| Conclusions supported by the results | 2 | 2 |
| Qualitative criteria | ||
| Question/objective sufficiently described | 1 | 1 |
| Study design evident and appropriate | 2 | 2 |
| The context for the study clear | 2 | 2 |
| Connection to a theoretical framework/wider body of knowledge | 0 | 0 |
| Sampling strategy described, relevant and justified | 1 | 2 |
| Data collection methods clearly described and systematic | 1 | 2 |
| Data analysis clearly described and systematic | 1 | 2 |
| Use of verification procedure (s) to establish credibility | 0 | 0 |
| Conclusions supported by the results | 1 | 2 |
| Reflexivity of the account | 0 | 0 |
| Overall quality score=total score/possible maximum score | 28/42=67% | 31/42=74% |
Table 4: Quality assessment results of mixed-method studies.
Our comprehensive Study identified a variety of potential barriers to the implementation of EBM in Ethiopia. The topmost frequently reported barriers are lack of EBM knowledge, inadequate resources, inadequate time, lack of EBM training, difficulty in interpreting research findings, lack of management support, overloading of patients, and negative attitude towards EBM.
One of the most important barriers identified in this study was the lack of EBM knowledge. This finding is consistent with previous systematic Studies, which have identified the lack of knowledge as the most frequently reported barrier to implementing EBM. Furthermore, evidence from Malaysia shows that lack of knowledge is a common obstacle to implementing EBM [38]. The possible explanation for this could be knowledge about EBM may increase their appraisal skills and give them more confidence in implementing EBM. Thus, EBM courses need to be incorporated at all levels of medical education to improve healthcare providers' skills important for applying EBM in their clinical practices. In addition, conducting EBM workshops is an effective awareness-raising strategy. The use of EBM professionals in health care organizations as a guide for other staffs can be an effective way to compensate for the poor knowledge of clinical staff in the EBM area.
Another major barrier to EBM implementation is the lack of resources. A systematic Study of EBM in low and middle-income countries has also suggested that resource constraints are one of the major obstacles to EBM implementation. To solve this problem, it is necessary to provide adequate resources. If this is not possible, low-cost strategies can be used to implement EBM. Unfortunately, sometimes there are enough resources but we cannot use them properly. Therefore, proper planning is required for proper resource allocation.
The results of this study are consistent with previous systematic Studies [39] and show that time constraints are one of the most common barriers to EBM implementation. Similarly, time constraints have been reported as one of the major obstacles to EBM implementation in low-income countries [40]. One of the possible reasons for lack of time might be healthcare professionals' high workload. To overcome the time limit, the workload of the clinicians needs to be reduced or more clinicians need to be hired. Lack of competence of clinicians in time management may also be another reason for lack of time. It may be useful to conduct a time management workshop to resolve this issue.
According to the result of this study, lack of EBM training is one of the most frequently reported barriers. In line with this finding, studies mentioned that inadequate training was a major barrier to implementing EBM. The reason could be that training may help healthcare providers to be clear more about the steps of practicing EBM. Findings from other studies also support the idea that training enhances healthcare professionals' knowledge and skills to implement EBM in their daily clinical service.
Lack of support from the management level was also identified as a significant obstacle in the implementation of EBM. Consistently, several studies have suggested that inadequate support from managers may be a barrier to implementing EBM [41-43]. Therefore, managers at all health system levels must be committed to implementing EBM. Policies and guidelines can be developed to overcome this obstacle so that people are committed to implementing EBM. Another way to promoting a culture of EBP support should be emphasizing the importance of EBM and its positive effects in healthcare quality. Providing financial and moral incentives to enhance cooperation in EBM may also be effective in this regard. Taking EBM into consideration when evaluating employees can also enhance their sense of motivation, support, and cooperation.
The results of this study have several policy implications. Our findings provided an early roadmap for planning a national policy for EBM implementation projects at all levels of health systems in Ethiopia. EBM policymakers and implementers such as hospital managers and project leaders can use the results to understand what constraints are present in their specific situations and to formulate evidence-based strategies to overcome them. Policymakers and administrators can also use this information as a practical guide to plan and design intervention programs for the sustainable implementation of EBM in Ethiopia. There are some limitations to this study. Although the authors conducted extensive searches, only a limited number of articles (n=11) were found. This may be due to limited research on EBM in Ethiopia.
In this paper, barriers to EBM implementation in Ethiopia are identified through a systematic Study of the literature. The main barriers reported in the literature are lack of EBM knowledge, insufficient resources, insufficient time, lack of EBM training, difficulty in interpreting research results, lack of management support, and negative attitude towards EBM. Context-specific strategies are needed to overcome the reported barriers. Common barriers can be addressed by using locally available, low-cost resources that require multiple strategies rather than single strategies. Intervention programs on awareness-raising, training, resource allocation and curriculum issues are needed to ensure the successful implementation of EBM in Ethiopia. Therefore, providing EBM training for healthcare professionals to thoroughly search EBM resources and critically appraise the evidence on a daily or weekly basis is essential to ensure that they have the necessary knowledge and skills to implement EBM in real clinical practice. Future researchers should build on our findings in order to build an EBM implementation framework that is sensitive to the historical, cultural, economic, workforce, and social needs of the Ethiopian health systems.
The authors received no specific funds for this study.
The authors have no conflict of interest to disclose.
All data generated or analyzed during this study are included in the article.
This study does not involve human participants.
DEY and ABE were responsible for the conception of the study. DEY, MYZ, and MSG implemented the search strategy. DGM and DNM conducted a Study of titles and abstracts. DEY wrote the manuscript with input from all authors. All authors contributed to the analysis and interpretation of data. All authors revised and approved the final version of the manuscript.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Yehualashet DE, Eshetu AB, Zeleke MY, Gebremedihn MS, Mengesha DG, Mamo DN (2022) Barriers to the Implementation of Evidence Based Medicine in Ethiopia: A Systematic Study. Emergency Med. 12:245
Received: 05-Jul-2022, Manuscript No. EGM-22-18700; Editor assigned: 08-Jul-2022, Pre QC No. EGM-22-18700 (PQ); Reviewed: 22-Jul-2022, QC No. EGM-22-18700; Revised: 29-Jul-2022, Manuscript No. EGM-22-18700 (R); Published: 05-Aug-2022 , DOI: 10.4172/2165-7548.22.12.245
Copyright: © 2022 Yehualashet DE, et al. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Sources of funding : The authors received no specific funds for this study.