Case Report - (2024)Volume 8, Issue 2
Background: Point of Care Ultrasonography (POCUS) is safe and rapidly evolving diagnosis modality and its now utilized by health care and professionals, the technology has been touted as visual stethoscope of the 21st century, abdominal pain continues to pose diagnostic challenges for emergency clinicians. In many cases, the differential diagnosis is wide.
Case presentation: A case of 50-year-old man was presented to the emergency department for evaluation of abdominal pain that started since 3 weeks, with fullness, bloating and occasional pain even though he cannot eat well probably, seen in another clinics and treated for Irritable Bowel Syndrome (IBS). The symptoms are progressively increasing last few days.
A Physical examination of the patient revealed normal vital signs, a distended and painless abdomen by deep palpation, no organomegaly or lymphadenopathy, his initial labs, show normal. Bedside Ultrasonography (US) showed ascites and distended intestinal loops, the patient was admitted to the medical ward, further labs and radiological study was done and diagnosed as small bowel lymphoma.
Conclusion: We present the case report to focus on value of bedside US for guiding the Emergency (ER) medicine physician assessment or even diagnosis besides the other skills.
Intestinal lymphoma; Abdominal pain; Ultrasonography; Irritable bowel syndrome
Abdominal pain complaints comprise about 5% of all Emergency Department (ED) visits. Many of these causes will be benign and self-limited, while others are medical urgencies or even surgical emergencies. As with any complaint in the ED, the worst diagnosis is always entertained first. Therefore, there is one thought, which the ED practitioner must maintain in the foreground of his mind is that ‘Is there a life-threatening process?’ (Table 1).
| Characteristics | Values |
|---|---|
| Abdominal pain of unknown origin | 41.3% |
| Gastroenteritis | 6.9% |
| Pelvic inflammatory disease | 6.7% |
| Urinary tract infection | 5.2% |
| Ureteral stone | 4.3% |
| Appendicitis | 4.3% |
| Acute cholecystitis | 2.5% |
| Intestinal obstruction | 2.5% |
| Constipation | 2.3% |
| Duodenal ulcer | 2.0% |
| Dysmenorrhea | 1.8% |
| Simple pregnancy | 1.8% |
| Pyelonephritis | 1.7% |
| Gastritis | 1.4% |
| Others | 12.8% |
Table 1: Common diagnoses of non-traumatic abdominal pain in the Emergency Department (ED) patients.
A pilot observational study showed that Emergency Physician (EP) performed US appears to positively impact decision-making and the diagnostic workup of patients with nonspecific abdominal pain as determined by the nursing triage. In 128 patients, 58 (45%, 95% Confidence Interval (CI), 36%-54%) had an improvement in diagnostic accuracy and planned diagnostic workup using US [1,2].
Emergency department ultrasonography
Includes all critical care ultrasonography, extended abdominal, testicular, early obstetric, musculoskeletal and ocular. Typically, single examination for diagnosis and disposition. Frequently leads to decision to discharge from hospital [3].
The patient was 50-year-old male who presented to ER complain of abnormal abdominal pain (pain score was 5) since 3 weeks and fullness, progressive course, loose of weight cannot eat well (feeling of distension) has been seen in the LHC and another outside clinic, treated symptomatically but not improve, he is Hypertension (HTN), type 2 Diabetes Mellitus (DM) and post Coronary Artery Bypass Graft (CABG) surgery in 2015, he is on Concor, Sitagliptin/Glucophage and aspirin, vitally stable, RBG 208 mg, afebrile . By examination not distressed but his abdomen looks distended, soft no guarding or localized tenderness, shifting dullness not done. Initial blood work done and abdominal X-ray; all were within normal, bed side US done by the ER physician which shows ascites and dilated intestinal loops (Figures 1 and 2).
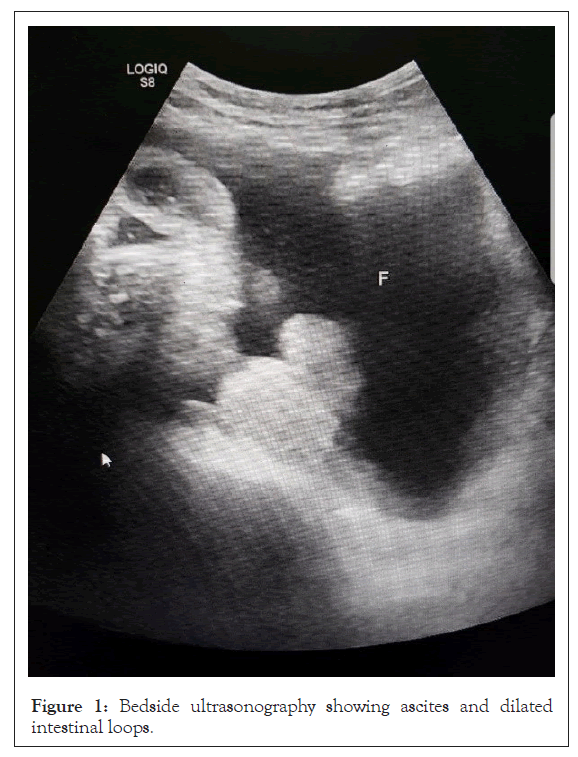
Figure 1: Bedside ultrasonography showing ascites and dilated intestinal loops.
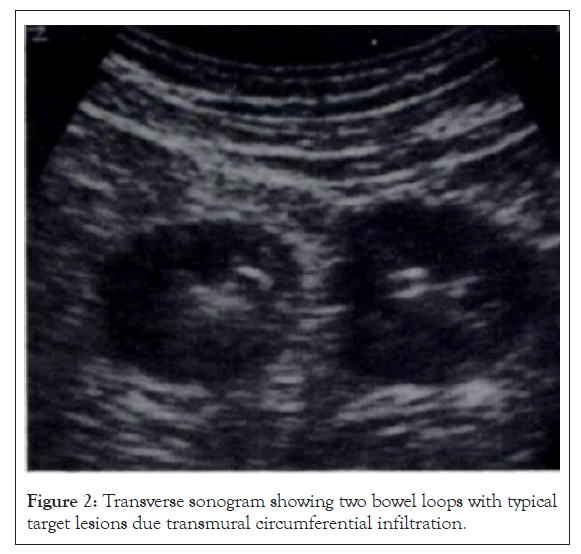
Figure 2: Transverse sonogram showing two bowel loops with typical target lesions due transmural circumferential infiltration.
Patient has been admitted in the medical ward and further study, abdominal and Computed Tomography (CT) chest and abdomen done that showed significant ascites with diffuse small bowel wall circumferential thickening involving the jejunal loops also was showing dilation of the lumen and involving multiple large segments and associated with numerous enlarged mesenteric and retroperitoneal lymph nodes with infiltration of mesentery, without luminal obstruction of the involved segments, normal spleen size and the liver showed diffuse heterogenous appearance without focal lesions, jejunal biopsy has been done and final diagnosis was T cell non-Hodgkin intestinal lymphoma.
Emergency US is synonymous with the terms clinical, bedside, point-of-care, focused and physician performed, but is part of a larger field of clinical ultrasonography. In this document, Endoscopic Ultrasound (EUS) refers to US performed by emergency physicians or clinicians in the emergency setting, while clinical ultrasonography refers to a multidisciplinary field of US use by clinicians at the point-of-care (Table 2) [4].
| Types of ultrasound | Definition |
|---|---|
| Resuscitative | US use directly related to a resuscitation |
| Diagnostic | US utilized a diagnostic imaging capacity |
| Symptom or sign-based | US used in a clinical pathway based upon the patient’s symptoms or sign (eg., shortness of breath) |
| Procedural guidance | US used as an aid to guide a procedure |
| Therapeutic and monitoring | US use in therapeutics or physiological monitoring |
| Consultative ultrasound | A written or electronic request for an US examination and interpretation for which the patient is transported to a laboratory or imaging department outside of the clinical setting |
| Emergency ultrasound | Performed and interpreted by the provider as an emergency procedure and directly integrated into the care of the patient |
| Clinical ultrasound | US used in the clinical setting, distinct from the physical examination, that adds anatomic, functional and physiologic information to the care of the acutely ill patient |
| Educational ultrasound | US performed in a non-clinical setting by medical students or other clinician trainees to enhance physical examination skills. Exams usually performed on cadavers or live models |
Note: US: Ultrasound.
Table 2: Relevant ultrasound definitions.
Primary gastrointestinal tract lymphoma account for approximately 0.9% off all Gastrointestinal Tract (GIT) tumors, symptoms are usually nonspecific and patient typically suffer from abdominal pain (65%), with bloody stool (27%), abdominal mass (20%), nausea, vomiting fatigue, loose of weight, symptoms of bowel obstruction or change of bowel habits [5,6]. The majority of GI lymphomas are of B-cell origin, while just 8%-10% show a T-cell origin, most low-grade B-cell GI lymphomas are of Mucosa-Associated Lymphoid Tissue (MALT) type, while enteropathy-associated T-cell lymphoma is the most common primary gastrointestinal T-cell lymphoma [7].
Lymphoma with serous effusion are common but prevalence varies in different cavities. The frequency of pleural effusion is 20%-30%, in Non-Hodgkin Lymphoma (NHL) and Hodgkin disease; however, ascites is rare presentation of lymphomas [8]. According to Vakar-Lopez, et al., [9] only 20 cases of lymphoma with ascites are the initial presentation have been reported.
In another analysis of 100 patients with ascites, Mahmood, et al., [10] reported lymphoma as the underlying cause of only 2% of cases. CT is the preferred modality also Magnetic Resonance Imaging (MRI) and US for evaluation of hepatic lymphoma and diagnosis of gastric lymphoma [11].
In this case, the presentation of the patient was sub-acute, about 3-4 weeks since start his complain, the bed side ER US gave alarming sings for admission and further rapid diagnosis. Its known that the utility of bedside abdominal US for identification of intraperitoneal fluids has be recognized since 1980s [12-14].
Finally, when US used as preliminary imaging investigation in patients with abdominal symptoms, such as abdominal pain or changes in bowel habits, US can identify abnormal intestinal findings or lesions that suggest intestinal diseases which may not primarily have been suspected The detection of these signs in patients with abdominal complaints and changes in bowel habit can adequately drive further investigations. Moreover, intestinal US can detect masses and neoplastic lesions of the gastrointestinal tract, in particular when in advanced stage. In contrast, the role of US in detecting or suggesting gastrointestinal functional disorders is not established and needs further investigation.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Shehabeldin MA (2024) Bedside Ultrasonography (US) in Approach the Diagnosis of a Case of Intestinal Lymphoma Presented with Sub- Acute Vague Abdominal Pain in ER: A Case Report. Acute Chronic Dis. 8:216.
Received: 03-May-2024, Manuscript No. ACDR-24-31007; Editor assigned: 06-May-2024, Pre QC No. ACDR-24-31007 (PQ); Reviewed: 20-May-2024, QC No. ACDR-24-31007; Revised: 27-May-2024, Manuscript No. ACDR-24-31007 (R); Published: 04-Jun-2024 , DOI: 10.35248/ACDR.24.8.216
Copyright: © 2024 Shehabeldin MA. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.